Bone loss in the teeth, medically referred to as alveolar bone resorption, is a significant dental condition that affects millions of people worldwide. It is a gradual process in which the jawbone supporting the teeth deteriorates, ultimately leading to tooth loss if left untreated. This condition can have a profound impact on oral health, aesthetics, and overall well-being. Understanding the causes, effects, and treatment options for bone loss in teeth is crucial for both prevention and management.
Table of Contents
ToggleWhat is Alveolar Bone?
The alveolar bone is the part of the jawbone that supports and holds the teeth in place. It surrounds the roots of the teeth and provides the necessary stability for proper chewing and speaking. This bone is constantly remodeled throughout life through a balance between bone formation and resorption, which is mediated by specialized cells called osteoblasts (bone-building cells) and osteoclasts (bone-resorbing cells). Under normal circumstances, this balance maintains the integrity of the jawbone. However, when the resorption of bone exceeds its formation, bone loss occurs.
Types of Bone Loss
Bone loss in the mouth primarily occurs in two forms:
- Horizontal bone loss
- Vertical bone loss
Horizontal bone loss
This involves a uniform reduction in the height of the alveolar bone around multiple teeth.
Vertical bone loss
This occurs in localized areas, creating pockets around specific teeth where the bone has receded more deeply in certain spots than others.
While both types of bone loss can lead to serious complications, vertical bone loss tends to be more aggressive and challenging to treat.
Causes of Bone Loss in Teeth
Several factors can contribute to bone loss in the jaw. These causes can be broadly categorized into periodontal diseases, tooth-related issues, and systemic health factors.
- Periodontal (Gum) Disease
- Tooth Loss and Missing Teeth
- Dentures and Ill-fitting Prosthetics
- Trauma or Injury to the Jaw
- Osteoporosis
- Malocclusion (Improper Bite) and Teeth Grinding
Periodontal (Gum) Disease
The most common cause of bone loss in teeth is periodontal disease, also known as gum disease. Periodontal disease is an inflammatory condition affecting the gums and the structures supporting the teeth, including the alveolar bone. It typically progresses in two stages: gingivitis (milder gum inflammation) and periodontitis (more severe, affecting deeper structures).
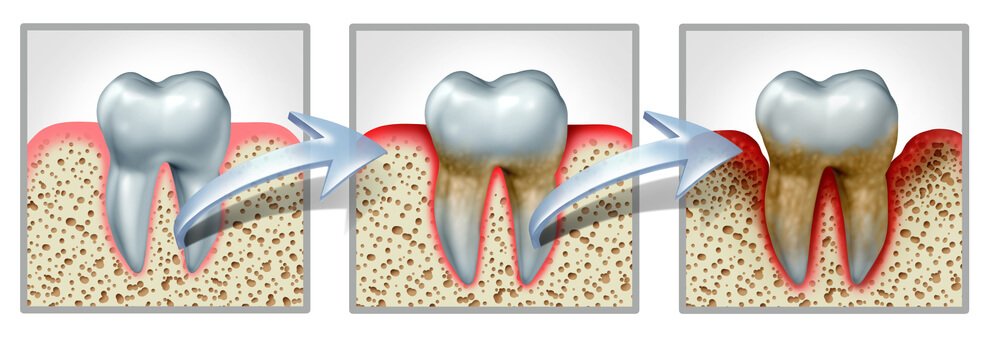
When bacteria in dental plaque build up on the teeth and gums, the body mounts an immune response to fight off the infection. However, this immune response can sometimes cause more harm than good. In severe cases, the body’s defense mechanisms break down not only the bacteria but also the tissues and bones that support the teeth. As a result, the alveolar bone becomes damaged and eventually resorbed. If left untreated, periodontitis can lead to significant bone loss, loose teeth, and even tooth loss.
Risk Factors for Periodontal Disease
- Poor oral hygiene: Failure to regularly brush and floss can lead to plaque accumulation, which fosters the growth of harmful bacteria that cause gum disease.
- Smoking: Tobacco use is a significant risk factor for periodontal disease. Smoking weakens the immune system and impairs blood circulation, making it harder for the body to fight off infections and heal from damage.
- Genetic predisposition: Some individuals may have a genetic susceptibility to gum disease, making them more prone to developing periodontal conditions despite good oral hygiene.
- Diabetes: People with diabetes are at a higher risk of developing gum disease due to impaired immune function and healing capabilities.
- Hormonal changes: Hormonal fluctuations, such as those experienced during pregnancy, menopause, or menstruation, can increase the risk of gum disease by making the gums more sensitive and susceptible to inflammation.
- Medications: Certain medications, such as those that reduce saliva flow (antihistamines, antidepressants, etc.), can contribute to gum disease by promoting dry mouth, which facilitates bacterial growth.
Tooth Loss and Missing Teeth
Bone loss can also occur when teeth are missing. When a tooth is lost, the alveolar bone that once supported it no longer has a functional purpose, and as a result, the bone begins to deteriorate. This is because the jawbone relies on the mechanical stimulation from chewing to maintain its density. Without the pressure and stimulation that comes from having teeth in place, the bone loses its strength and density.
In the first year following tooth loss, up to 25% of the bone volume in the affected area can be lost. This process continues over time, leading to further bone resorption. The longer the tooth remains missing, the greater the extent of bone loss.
Dentures and Ill-fitting Prosthetics
For individuals who have lost teeth and rely on dentures or other prosthetic devices, bone loss can still be an issue. Traditional removable dentures do not provide the same stimulation to the jawbone that natural teeth do. As a result, the bone underneath the denture continues to resorb over time, leading to a gradual reduction in bone volume.
Ill-fitting dentures, in particular, can exacerbate bone loss. If a denture does not fit properly, it can cause uneven pressure on certain areas of the jawbone, accelerating the resorption process. This leads to a vicious cycle where bone loss causes dentures to become loose, and loose dentures cause further bone loss.
Trauma or Injury to the Jaw
Trauma or injury to the jaw, whether due to accidents, falls, or sports-related injuries, can lead to localized bone loss. When the bone or surrounding structures are damaged, the body may resorb the injured bone tissue as part of the healing process. This is especially true if the trauma leads to tooth loss or damage to the roots of the teeth.
Osteoporosis
Osteoporosis is a systemic condition characterized by the weakening of bones throughout the body, including the jawbone. People with osteoporosis have an increased risk of bone loss in their jaws, which can result in tooth loss. Research has shown a strong correlation between osteoporosis and the severity of periodontitis. Women, in particular, are more prone to osteoporosis-related bone loss, especially after menopause due to a decline in estrogen levels.
Malocclusion (Improper Bite) and Teeth Grinding
Malocclusion, or misalignment of the teeth, can place excessive stress on certain areas of the jawbone, leading to bone resorption over time. Similarly, teeth grinding (bruxism) can create excessive pressure on the teeth and their supporting structures, which can accelerate bone loss. These conditions can result in uneven bone distribution and the formation of bone defects around certain teeth.
Effects of Bone Loss in Teeth
The consequences of bone loss in teeth extend beyond the obvious impact on oral health. The effects can be functional, aesthetic, and psychological, affecting various aspects of a person’s quality of life.
- Tooth Mobility and Loss
- Changes in Facial Appearance
- Difficulty Chewing and Speaking
- Impact on Oral Health
- Psychological and Emotional Effects
Tooth Mobility and Loss
As the alveolar bone deteriorates, the teeth become less stable. This leads to tooth mobility, where teeth may shift or feel loose in their sockets. Over time, if the bone loss is not addressed, the teeth may become too loose to remain in place, leading to tooth loss. The loss of teeth further compounds the problem, as it can lead to additional bone loss in the affected area.
Changes in Facial Appearance
The alveolar bone plays a critical role in supporting the structure of the face. When bone loss occurs, especially after tooth loss, it can lead to visible changes in facial appearance. The jawbone shrinks, causing the face to sag and creating a sunken or prematurely aged look. This is particularly noticeable around the cheeks and mouth, where the lips may appear thinner and the lower face shorter.
Difficulty Chewing and Speaking
Bone loss and the associated tooth mobility can make it difficult to chew food properly. This can affect a person’s ability to eat a balanced diet, as they may avoid certain foods that are hard to chew, such as fruits, vegetables, and meat. Additionally, speech can be affected, especially if multiple teeth are lost or become loose. Proper pronunciation of certain sounds relies on the position and stability of the teeth.
Impact on Oral Health
Bone loss creates pockets or gaps between the gums and the teeth, which can trap food particles and bacteria. These pockets are difficult to clean with regular brushing and flossing, making them breeding grounds for further bacterial growth. This increases the risk of developing infections, abscesses, and further periodontal disease, perpetuating a cycle of bone loss and deterioration.
Psychological and Emotional Effects
The aesthetic and functional consequences of bone loss can have a significant impact on a person’s self-esteem and confidence. Individuals who experience tooth loss or facial changes may feel embarrassed about their appearance, leading to social withdrawal or a reluctance to smile or speak in public. These psychological effects can have a profound impact on one’s overall quality of life.
Diagnosis of Bone Loss
The diagnosis of bone loss typically involves a combination of clinical examination and diagnostic imaging. Dentists and periodontists can assess the condition of the gums, teeth, and surrounding bone using the following methods:
- Dental X-rays
- CT Scans and 3D Imaging
- Periodontal Probing
Dental X-rays
X-rays are one of the most common tools used to diagnose bone loss. They provide a clear image of the bone surrounding the teeth and can show areas where the bone has deteriorated. Panoramic X-rays, which capture a broad view of the entire jaw, are particularly useful for assessing bone density and identifying areas of significant bone loss.
CT Scans and 3D Imaging
For more detailed imaging, dentists may use cone beam computed tomography (CBCT) or other 3D imaging techniques. These advanced diagnostic tools provide a more comprehensive view of the jawbone, allowing for precise measurements of bone loss and helping in treatment planning, especially in cases involving dental implants.
Periodontal Probing
During a periodontal examination, the dentist may use a probe to measure the depth of the gum pockets around the teeth. Deeper pockets indicate more advanced periodontal disease and are often associated with greater bone loss.
Treatment Options for Bone Loss
Treating bone loss in teeth involves addressing both the underlying causes and the damage that has already occurred. While the goal is often to stop further bone loss, modern dentistry also offers solutions to regenerate lost bone and restore oral health. Treatment plans may vary depending on the extent of bone loss, the cause, and the patient’s overall health. Below are the primary treatment options:
- Non-Surgical Treatments
- Surgical Treatments
- Dental Implants
- Platelet-Rich Plasma (PRP) Therapy
- Medications for Bone Regeneration
- Lifestyle Changes and Prevention
Non-Surgical Treatments
- Scaling and Root Planing
- Antibiotic Therapy
Scaling and Root Planing
Scaling and root planing is a deep cleaning procedure aimed at removing plaque and tartar buildup from beneath the gumline. This is often the first line of defense against periodontal disease and is performed under local anesthesia. The procedure helps eliminate bacteria from the pockets around the teeth, reducing inflammation and giving the bone a chance to heal.
Scaling involves removing the hardened plaque (tartar) from the surface of the teeth, especially in the deep pockets created by bone loss.
Root planing smooths the tooth root to discourage further bacterial buildup and help the gums reattach to the tooth.
For mild to moderate cases of periodontal disease, this procedure can help prevent further bone deterioration. However, it may not be effective in treating advanced bone loss.
Antibiotic Therapy
In some cases, dentists may prescribe antibiotics to control bacterial infection in the gums. Antibiotics can be administered orally or placed directly into the gum pockets to target the specific areas of infection. Antibiotic gels or mouth rinses may also be used as adjunctive therapy following scaling and root planing. While antibiotics can help manage the infection, they do not reverse bone loss but can halt its progression.
Surgical Treatments
- Flap Surgery
- Bone Grafting
- Guided Tissue Regeneration (GTR)
- Soft Tissue Grafting
Flap Surgery
Flap surgery, also known as pocket reduction surgery, is a more invasive treatment option for advanced periodontal disease. During this procedure, the dentist or periodontist makes small incisions in the gums to lift back the tissue and expose the roots of the teeth and the underlying bone. This allows for more thorough cleaning of the root surfaces and the removal of any infected tissue.
Once the area is cleaned, the gum tissue is repositioned and stitched back into place. In some cases, the bone may be reshaped to reduce the size of the gum pockets. Flap surgery can help prevent further bone loss, although it does not restore lost bone.
Bone Grafting
Bone grafting is a common surgical procedure used to rebuild lost bone in the jaw. This is often necessary when significant bone loss has occurred, especially for patients planning to receive dental implants or who are at risk of losing more teeth. Bone grafts involve transplanting bone material to the affected area to encourage the growth of new bone cells.
- Autografts: Bone is taken from another part of the patient’s body, such as the chin or hip.
- Allografts: Bone material is sourced from a human donor, usually from a bone bank.
- Xenografts: Bone material is derived from animals, typically cows.
- Alloplastic grafts: Synthetic materials are used to stimulate bone growth.
After the graft is placed, the body gradually integrates the new material, and natural bone regeneration occurs. Bone grafting can take several months to heal, but it can effectively restore lost bone density and provide a stable foundation for future dental restorations.
Guided Tissue Regeneration (GTR)
Guided tissue regeneration is a specialized surgical procedure used to encourage the regrowth of bone and tissue around teeth affected by periodontal disease. During this procedure, a biocompatible membrane is placed between the gum and bone to prevent unwanted tissue from growing into the space where the bone needs to regenerate. This membrane acts as a barrier, allowing the bone and connective tissues to grow and repair themselves.
GTR is often combined with bone grafting to enhance the regrowth process. Over time, the membrane is resorbed by the body, and the regenerated bone helps to stabilize the teeth.
Soft Tissue Grafting
In cases where gum recession accompanies bone loss, soft tissue grafting may be performed to restore the health and appearance of the gums. Gum recession often leads to the exposure of the tooth root, making it more susceptible to decay, sensitivity, and further bone loss. Soft tissue grafting involves taking tissue from another area of the mouth, typically the roof of the mouth, and attaching it to the affected area to cover exposed roots and promote gum regeneration.
Dental Implants
Dental implants are one of the most effective long-term solutions for replacing missing teeth and preventing further bone loss. Unlike traditional dentures or bridges, dental implants are surgically placed into the jawbone, where they fuse with the bone through a process called osseointegration. This integration mimics the function of natural tooth roots, providing the necessary stimulation to maintain bone density and prevent further bone resorption.
Types of Implants
- Endosteal implants: These are the most common type of dental implants and are placed directly into the jawbone.
- Subperiosteal implants: These implants are placed on top of the jawbone but beneath the gum tissue. They are often used in cases where there is not enough bone height for endosteal implants.
For patients with significant bone loss, bone grafting may be required before dental implants can be placed to ensure there is enough bone volume to support the implant.
Dental implants offer several benefits, including improved chewing function, enhanced aesthetics, and prevention of further bone loss. However, they require a healthy amount of bone to be successful, making early intervention for bone loss critical.
Platelet-Rich Plasma (PRP) Therapy
Platelet-rich plasma (PRP) therapy is a regenerative treatment that uses a patient’s own blood to promote healing and tissue regeneration. PRP is rich in growth factors that stimulate bone and tissue repair. In the context of bone loss in teeth, PRP can be used in conjunction with bone grafting or other surgical procedures to accelerate the healing process and enhance bone regeneration.
During PRP therapy, a small amount of blood is drawn from the patient, processed to concentrate the platelets, and then applied to the treatment area. This promotes faster recovery and can improve the outcome of bone regeneration procedures.
Medications for Bone Regeneration
In some cases, dentists may recommend medications to stimulate bone regeneration or slow the progression of bone loss. These medications include:
- Bisphosphonates: Often used to treat osteoporosis, bisphosphonates can help prevent further bone resorption by inhibiting the activity of osteoclasts, the cells responsible for bone breakdown. However, there are some concerns about the use of bisphosphonates in dentistry, as they have been associated with a rare condition called osteonecrosis of the jaw.
- Bone Morphogenetic Proteins (BMPs): BMPs are proteins that stimulate bone growth and are sometimes used in bone grafting procedures to enhance bone regeneration.
Lifestyle Changes and Prevention
Preventing further bone loss requires a proactive approach to oral health and overall well-being. The following lifestyle changes and preventive measures can help minimize the risk of bone loss:
- Maintain excellent oral hygiene: Regular brushing and flossing are essential to prevent plaque buildup and the progression of periodontal disease.
- Regular dental check-ups: Routine dental visits allow for early detection of gum disease and bone loss. Professional cleanings help remove tartar and plaque that cannot be removed with regular brushing alone.
- Quit smoking: Smoking is a significant risk factor for both gum disease and bone loss. Quitting smoking can improve oral health and slow the progression of bone loss.
- Manage systemic conditions: Conditions such as diabetes and osteoporosis can contribute to bone loss in the jaw. Managing these conditions with appropriate medical care can reduce the risk of complications in the mouth.
- Eat a balanced diet: A diet rich in calcium, vitamin D, and other nutrients is crucial for maintaining healthy bones. Foods such as dairy products, leafy greens, nuts, and fish provide the essential nutrients needed for bone health.
- Avoid excessive alcohol consumption: Excessive alcohol intake can contribute to bone loss and impair overall oral health.
- Wear protective gear: If you engage in contact sports or activities where injury to the jaw is possible, wearing a mouthguard can protect against trauma that may lead to bone loss.
Frequently Asked Questions (FAQs)
What does dental bone loss feel like?
Dental bone loss often doesn’t cause noticeable symptoms in the early stages. However, as it progresses, you may experience loose teeth, receding gums, increased tooth sensitivity, difficulty chewing, or even pain in the affected areas.
Can you reverse dental bone loss?
While dental bone loss cannot be completely reversed, it can be slowed down and, in some cases, partially regenerated with treatments like bone grafts, guided tissue regeneration, and certain lifestyle changes.
What is the best treatment for bone loss in teeth?
The best treatment depends on the severity of bone loss. Common treatments include bone grafts, periodontal therapy, dental implants, and medications to promote bone growth. In mild cases, improved oral hygiene and diet changes may help slow progression.
Can teeth with bone loss be saved?
Yes, teeth with bone loss can often be saved if treated early. Deep cleanings, gum grafts, bone grafting, and proper oral care can help stabilize teeth and prevent further damage.
How to repair bone loss in teeth naturally?
Natural approaches include maintaining excellent oral hygiene, eating a calcium and vitamin D-rich diet, using fluoride toothpaste, and avoiding smoking or excessive alcohol. However, severe bone loss typically requires professional intervention.
When is it too late to save my teeth?
It’s too late to save a tooth when there is severe bone loss, excessive mobility, or an infection that cannot be treated. In such cases, extraction and possible replacement with a dental implant or bridge may be necessary.
How to build bone back in teeth?
Bone regeneration may be possible through bone grafting, guided bone regeneration, and a nutrient-rich diet that includes calcium, phosphorus, and vitamin D. In some cases, specialized medications may help stimulate bone growth.
What is the best toothpaste for receding gums?
Toothpaste formulated for gum health, such as those containing fluoride, stannous fluoride, or aloe vera, can help. Some popular options include Sensodyne Pronamel, Parodontax, and Crest Gum Detoxify.
Can salt water tighten loose teeth?
Salt water rinses can help reduce gum inflammation and fight bacteria, but they do not tighten loose teeth caused by bone loss. If you have loose teeth, consult a dentist for treatment options.
Conclusion
Bone loss in teeth is a serious dental condition that can lead to significant oral health complications if left untreated. The causes of bone loss are varied, with periodontal disease being the leading factor. However, other factors such as missing teeth, ill-fitting dentures, trauma, osteoporosis, and improper bite can also contribute to bone resorption.
The effects of bone loss extend beyond tooth stability, affecting facial appearance, chewing ability, and overall quality of life. Fortunately, modern dentistry offers a range of treatment options to stop bone loss, regenerate lost bone, and restore oral function. Non-surgical methods such as scaling and root planing can help in the early stages, while surgical interventions like bone grafting, guided tissue regeneration, and dental implants provide more advanced solutions.
Preventing bone loss requires a commitment to good oral hygiene, regular dental visits, and lifestyle modifications such as quitting smoking and managing systemic health conditions. By understanding the causes and treatments for bone loss, individuals can take proactive steps to protect their oral health and preserve their teeth for a lifetime.

