Osseointegration is a fundamental concept in modern dentistry and orthopedics, playing a pivotal role in the success of various implant procedures. It involves the direct and structural connection between living bone and the surface of a load-bearing artificial implant. This process enables the implant to function seamlessly within the body, providing stability and support for prosthetic devices like dental implants and joint replacements. In this article, we will delve into the intricacies of osseointegration, its history, mechanisms, applications, and advancements in the field.
History and Evolution
The term “osseointegration” was first coined by Per-Ingvar Brånemark, a Swedish orthopedic surgeon and researcher, in the 1950s. Dr. Brånemark observed that titanium could fuse with bone tissue and coined the term to describe this phenomenon. His groundbreaking research laid the foundation for modern dental implantology.
Dr. Brånemark’s discovery marked a paradigm shift in the world of orthopedic and dental implants. Prior to osseointegration, the main focus was on creating stable mechanical connections between implants and the body, often leading to issues of instability, discomfort, and ultimately implant failure.
Mechanisms of Osseointegration
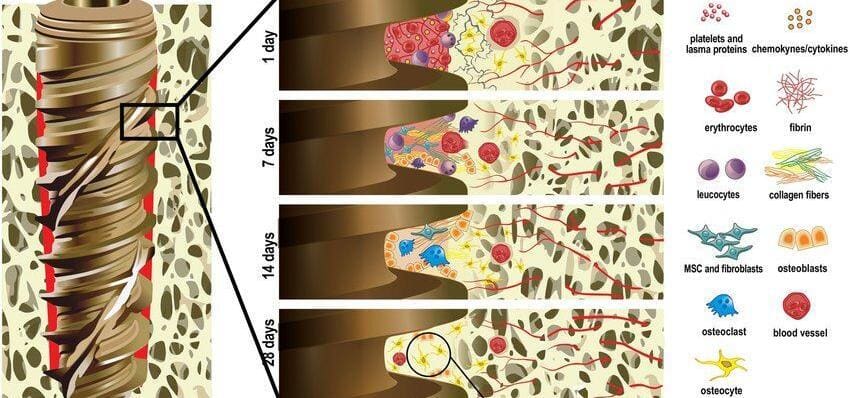
Osseointegration is a biological process that involves several stages, primarily characterized by the interaction between the implant surface and the bone tissue.
- Initial Contact and Protein Adsorption
- Cell Attachment
- Matrix Formation
- Remodeling
Initial Contact and Protein Adsorption
When an implant is placed in bone, it makes initial contact with the bone surface. Proteins from the blood then adhere to the implant surface, facilitating the attachment of bone-forming cells.
Cell Attachment
Cells from the surrounding bone, such as osteoblasts and fibroblasts, attach to the implant surface. Osteoblasts are responsible for the formation of new bone, while fibroblasts contribute to the formation of connective tissue.
Matrix Formation
Osteoblasts produce a mineralized extracellular matrix, which ultimately forms bone. This matrix solidifies and integrates with the implant surface, creating a strong connection.
Remodeling
The bone around the implant undergoes continuous remodeling, adapting to the stress and strains placed upon it. This ensures a strong and stable integration over time.
Applications in Dentistry
Osseointegration has revolutionized the field of dentistry, particularly in the realm of dental implants. Dental implants are artificial tooth roots made of biocompatible materials like titanium. These implants are surgically placed into the jawbone, providing a stable foundation for replacement teeth, bridges, or dentures.
The success of dental implants largely depends on the degree of osseointegration achieved between the implant and the surrounding bone. Proper osseointegration ensures the stability and longevity of the implant, enabling patients to regain natural biting and chewing functions, along with an aesthetically pleasing smile.
What Conditions Can Affect Osseointegration?
Osseointegration, the process of direct integration between an implant and living bone, can be influenced by various conditions. It’s essential to consider both patient-specific factors and aspects related to the implant itself. Here are some key conditions that can affect osseointegration:
- Bone Quality and Quantity
- Patient Health and Medical History
- Smoking and Tobacco Use
- Infection and Inflammation
- Implant Surface Characteristics
- Surgical Technique and Implant Placement
- Biocompatibility and Material Selection
- Postoperative Care and Compliance
- Age and Hormonal Factors
- Medications and Treatments
Bone Quality and Quantity
The density, structure, and volume of the bone at the implant site significantly impact osseointegration. Insufficient bone quantity or poor bone quality may lead to compromised osseointegration.
Patient Health and Medical History
Certain medical conditions and systemic factors can affect osseointegration. Patients with diabetes, osteoporosis, autoimmune disorders, or a history of radiation therapy may experience challenges in bone healing and integration.
Smoking and Tobacco Use
Tobacco use, particularly smoking, can significantly hinder osseointegration. Nicotine and other harmful substances in tobacco can impair blood flow, delay wound healing, and reduce bone density, all of which negatively affect the integration of the implant with bone.
Infection and Inflammation
Pre-existing or postoperative infections can disrupt the osseointegration process. Inflammation at the surgical site can impede healing and the formation of the bone-implant interface.
Implant Surface Characteristics
The surface properties of the implant, including roughness, topography, and composition, play a crucial role in osseointegration. Implants with appropriate surface modifications enhance the speed and quality of bone integration.
Surgical Technique and Implant Placement
The precision and skill used during implant surgery significantly affect osseointegration. Proper implant placement, adequate primary stability, and atraumatic surgical techniques are crucial for successful osseointegration.
Biocompatibility and Material Selection
The choice of implant material is vital. Biocompatible materials, such as titanium and its alloys, are commonly used due to their excellent biocompatibility and ability to integrate with bone. Allergies or adverse reactions to implant materials can impede osseointegration.
Postoperative Care and Compliance
Following proper postoperative care instructions and maintaining good oral hygiene is essential for successful osseointegration. Neglecting postoperative care can lead to complications that affect the integration process.
Age and Hormonal Factors
Age-related factors and hormonal changes, particularly in postmenopausal women, can influence bone density and healing rates, potentially affecting osseointegration.
Medications and Treatments
Certain medications, such as bisphosphonates used to treat osteoporosis, may impact bone healing and integration with implants.
Understanding and managing these factors are critical for clinicians to optimize osseointegration and achieve successful outcomes in implant dentistry and orthopedics. Tailoring treatment plans based on individual patient characteristics and careful consideration of these conditions can significantly enhance the chances of successful osseointegration.
Advancements and Innovations
In recent years, continuous research and advancements in materials and surgical techniques have further enhanced osseointegration outcomes.
- Improved Implant Surface Modifications
- Computer-Aided Design and Manufacturing (CAD/CAM)
- Stem Cell and Growth Factor Applications
Improved Implant Surface Modifications
Innovations in implant surface treatments, such as sandblasting, acid etching, and incorporation of bioactive coatings, have significantly enhanced osseointegration by promoting faster and more effective bone integration.
Computer-Aided Design and Manufacturing (CAD/CAM)
CAD/CAM technology allows for precise planning and customization of implant placement based on individual patient anatomy. This technology ensures optimal positioning and alignment of implants, enhancing osseointegration outcomes.
Stem Cell and Growth Factor Applications
Research is ongoing in utilizing stem cells and growth factors to stimulate and accelerate bone growth and osseointegration around implants. These bioengineering approaches hold promise for further improving implant success rates.
Future Prospects and Conclusion
The future of osseointegration is incredibly promising, with ongoing research and development poised to revolutionize implantology and further improve patient outcomes. Here are some potential future directions and advancements that may shape the field:
- Biological Implant Coatings
- 3D Printing and Nanotechnology
- Drug Delivery Systems
- Regenerative Medicine and Tissue Engineering
- Personalized Medicine
Biological Implant Coatings
Researchers are exploring the potential of incorporating biological coatings on implant surfaces. These coatings may mimic the natural composition of bone, promoting a more seamless integration with the surrounding tissue.
3D Printing and Nanotechnology
3D printing and nanotechnology offer exciting opportunities for creating implants with highly intricate structures and precise surface modifications. These advancements can optimize implant geometry and surface features for enhanced osseointegration.
Drug Delivery Systems
Incorporating drug delivery systems into implant designs can enable controlled and localized release of therapeutic agents to enhance osseointegration. This approach can promote bone growth and inhibit inflammation or infection, improving the success rates of implants.
Regenerative Medicine and Tissue Engineering
Integration of regenerative medicine principles and tissue engineering techniques may allow for the creation of implantable devices that can actively support tissue regeneration, further enhancing osseointegration.
Personalized Medicine
Advancements in genetics and personalized medicine may enable tailored implant designs and treatment plans based on an individual’s genetic makeup and bone characteristics. This could significantly enhance osseointegration success rates.
Conclusion
Osseointegration is a fundamental biological process that has revolutionized the field of implantology, providing countless individuals with improved oral health and overall well-being. The journey from its discovery by Dr. Per-Ingvar Brånemark to the current state of advanced research and technology showcases the immense potential that osseointegration holds in the realm of modern healthcare.
As we move forward, embracing and furthering these advancements in osseointegration will undoubtedly lead to even more effective, safe, and long-lasting solutions for patients seeking implant-based treatments. The interdisciplinary collaboration between researchers, clinicians, engineers, and material scientists will be instrumental in realizing these potential advancements and bringing them into clinical practice, ultimately benefiting individuals seeking improved quality of life through implant-based therapies.