Cushing syndrome, also known as hypercortisolism, is a condition characterized by prolonged exposure to elevated levels of cortisol, a steroid hormone produced by the adrenal glands. This condition can arise due to various causes, including endogenous overproduction by the adrenal glands or exogenous corticosteroid therapy. It affects multiple body systems, leading to systemic complications that require attention in various healthcare disciplines, including dentistry.
Dentists often encounter patients with underlying systemic conditions, including Cushing syndrome, making it crucial to understand its implications for dental treatment. This article provides an overview of Cushing syndrome, its pathophysiology, clinical manifestations, diagnosis, and management. Additionally, it emphasizes the importance of recognizing its implications in dentistry and highlights precautions dentists should take when treating affected individuals.
Table of Contents
TogglePathophysiology and Causes of Cushing Syndrome
Cushing syndrome arises due to excessive cortisol levels in the body. Cortisol, produced by the adrenal cortex, plays a vital role in regulating metabolism, immune responses, and stress adaptation. Its overproduction leads to a wide range of physiological disruptions.
Exogenous Causes
Prolonged use of corticosteroid medications (e.g., prednisone) for conditions such as asthma, rheumatoid arthritis, or organ transplantation.
Endogenous Causes
- Pituitary Adenomas (Cushing Disease)
- Adrenal Tumors
- Ectopic ACTH Production
Pituitary Adenomas (Cushing Disease)
Benign tumors in the pituitary gland that secrete adrenocorticotropic hormone (ACTH), stimulating cortisol production.
Adrenal Tumors
Either benign or malignant growths in the adrenal glands leading to autonomous cortisol secretion.
Ectopic ACTH Production
Rare tumors outside the pituitary gland (e.g., lung cancer) that secrete ACTH.
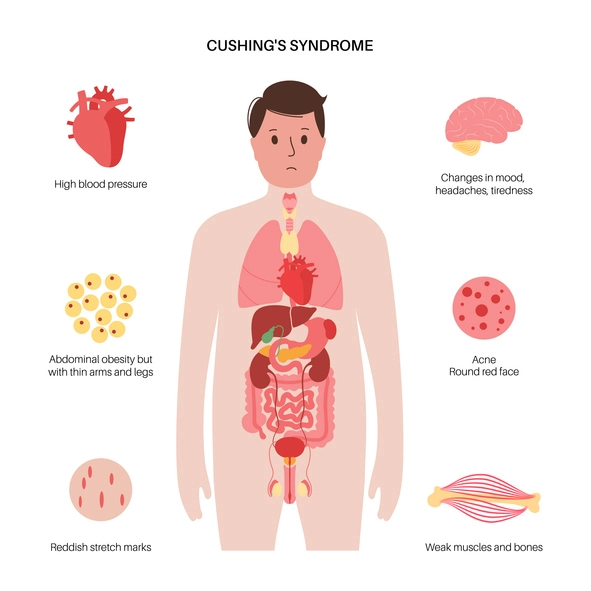
Clinical Manifestations
Cushing syndrome presents with a range of symptoms and signs, many of which are relevant to dental practitioners:
General Symptoms
- Weight Gain – Particularly in the face, neck, and trunk (central obesity).
- Moon Face – Round and full facial appearance due to fat deposition.
- Skin Changes – Thinning of the skin, easy bruising, and purple striae (stretch marks).
- Hypertension and Hyperglycemia – Common due to cortisol’s effects on blood pressure and glucose metabolism.
- Osteoporosis – Increased bone fragility and susceptibility to fractures.
- Immunosuppression – Higher susceptibility to infections, including oral infections.
Oral and Dental Manifestations
- Delayed Wound Healing – Cortisol impairs tissue repair, which can complicate dental procedures such as extractions and surgeries.
- Oral Infections – Increased risk of candidiasis, gingivitis, and periodontitis due to immunosuppression.
- Bone Loss – Exacerbated periodontal disease due to reduced bone density and poor bone turnover.
- Dry Mouth (Xerostomia) – Possible side effect of medications or systemic effects of the syndrome.
Diagnosis of Cushing Syndrome
Diagnosing Cushing syndrome involves clinical evaluation, biochemical testing, and imaging studies. Dentists should be aware of the diagnostic criteria to identify potential cases during routine check-ups.
Diagnostic Steps
1. Clinical History and Physical Examination
Identifying characteristic symptoms like central obesity, facial rounding, and skin changes.
2. Biochemical Testing
- 24-Hour Urinary Free Cortisol Test – Measures cortisol excretion in urine.
- Low-Dose Dexamethasone Suppression Test – Assesses the ability of exogenous steroids to suppress cortisol production.
- Late-Night Salivary Cortisol – Detects loss of cortisol diurnal rhythm.
3. Imaging
MRI or CT scans to identify pituitary or adrenal tumors.
Importance of Cushing Syndrome in Dentistry
Dentists must consider the systemic effects of Cushing syndrome when planning and performing dental treatments. Its manifestations can significantly impact oral health, wound healing, and the overall success of dental procedures.
Key Considerations in Dentistry
- Delayed Healing and Surgical Complications
- Infection Risk
- Bone Fragility
- Medication Interactions
- Management of Xerostomia
Delayed Healing and Surgical Complications
The impaired wound healing associated with Cushing syndrome increases the risk of post-operative complications such as infections and dehiscence after oral surgeries.
Infection Risk
Immunosuppression raises susceptibility to oral infections, including bacterial and fungal infections. Early identification and management of oral infections are crucial.
Bone Fragility
Patients with osteoporosis are at higher risk of jaw fractures during extractions or trauma. The dentist must handle procedures delicately to prevent complications.
Medication Interactions
Many patients with Cushing syndrome are on corticosteroid therapy, necessitating careful assessment of drug interactions and possible steroid supplementation during dental procedures.
Management of Xerostomia
Dry mouth can exacerbate caries risk and oral discomfort. Dentists should provide guidance on maintaining oral hydration and recommend appropriate salivary substitutes or stimulants.
Precautions for Dentists When Treating Patients with Cushing Syndrome
Dentists should adopt a multidisciplinary approach when managing patients with Cushing syndrome, involving endocrinologists and primary care physicians to ensure comprehensive care.
Pre-Treatment Evaluation
- Obtain a thorough medical history, including details about Cushing syndrome, medication use, and systemic complications.
- Assess the patient’s current cortisol levels and adrenal function to evaluate the need for perioperative steroid supplementation.
Treatment Planning
- Minimizing Invasive Procedures
- Steroid Supplementation
- Antibiotic Prophylaxis
- Radiographic Assessment
Minimizing Invasive Procedures
When possible, avoid invasive dental procedures in uncontrolled cases. Postpone elective surgeries until the syndrome is better managed.
Steroid Supplementation
Patients on long-term corticosteroid therapy may require stress dose steroids before and after major dental procedures to prevent adrenal insufficiency.
Antibiotic Prophylaxis
Consider antibiotic coverage for procedures that carry a high risk of infection.
Radiographic Assessment
Evaluate bone density through radiographs before extractions or implant placements to assess fracture risk.
Intraoperative Care
- Employ gentle surgical techniques to minimize trauma and promote better healing.
- Ensure strict aseptic protocols to reduce infection risk.
Postoperative Care
- Monitor closely for signs of delayed healing or infection.
- Advise patients on maintaining good oral hygiene and provide instructions to manage potential complications such as dry mouth and increased caries risk.
Patient Education and Communication
Educating patients about their condition and its impact on oral health is vital. Dentists should provide tailored advice on maintaining oral hygiene, recognizing signs of infections, and managing side effects of medications. Collaboration with other healthcare providers ensures that the patient’s systemic health is well-coordinated with dental care.
Frequently Asked Questions (FAQs)
Can a dentist diagnose Cushing syndrome?
No, a dentist cannot diagnose Cushing syndrome but can recognize oral and systemic signs suggestive of the condition and refer the patient to an endocrinologist for further evaluation.
How does Cushing syndrome affect oral health?
Cushing syndrome increases the risk of oral infections, periodontal disease, dry mouth, and delayed wound healing. It also contributes to bone loss, which can impact dental procedures like extractions and implants.
Can a patient with Cushing syndrome undergo dental surgery?
Yes, but precautions must be taken. The dentist should assess the patient’s adrenal function, ensure adequate steroid coverage if needed, and use careful surgical techniques to minimize complications.
Are dental implants safe for patients with Cushing syndrome?
Dental implants can be placed, but due to increased bone fragility and impaired healing, dentists must evaluate bone quality and consider alternative treatments if necessary.
What oral hygiene measures should patients with Cushing syndrome take?
Patients should maintain excellent oral hygiene by brushing twice a day, flossing regularly, using fluoride toothpaste, and staying hydrated to manage dry mouth. Regular dental check-ups are essential to prevent infections.
Should patients with Cushing syndrome stop their steroid medication before dental procedures?
No, patients should not stop their steroids without medical supervision. In some cases, additional steroids may be required to prevent adrenal insufficiency.
Conclusion
Cushing syndrome is a complex endocrine disorder with significant implications for dental practice. Understanding its pathophysiology, clinical manifestations, and systemic impact enables dentists to provide safe and effective care to affected patients. By adopting a multidisciplinary approach, implementing appropriate precautions, and prioritizing patient education, dentists can minimize complications and enhance treatment outcomes for individuals with Cushing syndrome. Recognizing the importance of this condition in dentistry underscores the need for continuous learning and collaboration in providing holistic care.