Oral wound healing is a complex and intricate process that plays a crucial role in maintaining oral health and overall well-being. From minor cuts and abrasions to more significant surgical interventions, the oral cavity is prone to a variety of injuries that necessitate effective wound healing mechanisms. In this article, we will delve into the intricate processes involved in oral wound healing, the factors influencing the healing process, and the significance of proper wound care to ensure optimal recovery.
Table of Contents
ToggleThe Phases of Oral Wound Healing
Oral wound healing is a dynamic process that occurs in several overlapping phases, each with its own distinct characteristics and functions. These phases include:
- Hemostasis
- Inflammation
- Proliferation
- Maturation
Hemostasis
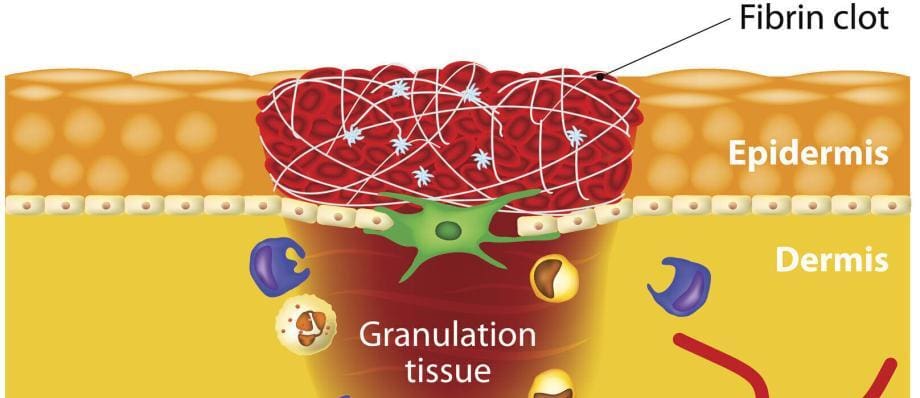
The initial phase of oral wound healing is hemostasis, which involves the formation of blood clots to prevent excessive bleeding. Platelets play a pivotal role in this phase by adhering to the injured blood vessel walls and releasing clotting factors. The clot formation creates a temporary barrier that helps control bleeding and creates a foundation for subsequent healing processes.
Inflammation
Following hemostasis, the inflammation phase begins. This phase is marked by the influx of immune cells, such as neutrophils and macrophages, to the wound site. These cells help clear away debris, pathogens, and damaged tissue. Inflammation also promotes the release of growth factors that stimulate the proliferation of cells necessary for tissue repair.
Proliferation
During the proliferation phase, the body focuses on rebuilding the damaged tissue. Fibroblasts play a central role in this phase by producing collagen, a critical protein that provides structural support to the wound. As collagen accumulates, it forms a framework for cell migration and tissue regeneration. Additionally, new blood vessels, or angiogenesis, begin to form, ensuring adequate oxygen and nutrient supply to the healing area.
Maturation
The final phase, maturation, involves the remodeling of the tissue that was formed during the proliferation phase. Collagen fibers undergo realignment, becoming more organized and acquiring increased tensile strength. This phase can last for an extended period, and the scar tissue gradually gains strength and functional integrity.
Factors Influencing Oral Wound Healing
Several intrinsic and extrinsic factors can significantly impact the oral wound healing process. Understanding these factors can aid in optimizing wound healing outcomes.
- Systemic Factors
- Nutrition
- Local Factors
- Medications
- Tobacco and Alcohol Use
- Oral Hygiene
Systemic Factors
Various systemic factors, such as age, overall health, and systemic diseases, can influence oral wound healing. Elderly individuals may experience delayed wound healing due to reduced cellular activity and diminished immune function. Conditions like diabetes and immune disorders can compromise the body’s ability to mount an effective healing response.
Nutrition
A balanced nutrition and adequate diet is essential for optimal wound healing. Nutrients like vitamin C, zinc, and protein play crucial roles in collagen synthesis and immune function. Deficiencies in these nutrients can impair wound healing and lead to complications.
Local Factors
The specific location of the oral wound can impact healing. Areas with high mechanical stress, such as the tongue, may experience slower healing due to constant movement and disruption of the wound site. Additionally, the presence of microorganisms in the oral cavity can lead to infections that impede the healing process.
Medications
Certain medications, such as immunosuppressants and steroids, can interfere with wound healing by suppressing the immune response and reducing inflammation. It’s important for healthcare providers to consider these factors when managing oral wounds in patients taking such medications.
Tobacco and Alcohol Use
Tobacco smoking and excessive alcohol consumption have been shown to have detrimental effects on wound healing. Nicotine restricts blood flow and oxygen delivery to the wound site, while alcohol can impair immune function and delay the healing process.
Oral Hygiene
Maintaining proper oral hygiene is crucial for preventing infections and promoting oral wound healing. Poor oral hygiene can introduce harmful bacteria to the wound site, leading to complications and delayed healing.
Proper Wound Care for Oral Wounds
Effective wound care is essential to facilitate optimal oral wound healing. Here are some key principles to follow:
- Cleanliness
- Moisture Balance
- Pain Management
- Follow Medical Advice
Cleanliness
Ensure that the wound area is kept clean to prevent infection. Gentle rinsing with saline solution or a prescribed mouthwash can help remove debris and reduce the risk of bacterial growth.
Moisture Balance
Maintaining the appropriate level of moisture at the wound site is crucial for optimal healing. Excess moisture can lead to maceration, while excessive dryness can impede cell migration and proliferation. Consultation with a healthcare provider can guide the appropriate use of wound dressings and moisturizing agents.
Pain Management
Oral wounds can be painful, especially during the initial phases of healing. Proper pain management, as advised by a healthcare professional, can improve patient comfort and compliance with wound care instructions.
Follow Medical Advice
Patients should strictly adhere to the instructions provided by their healthcare provider. This may include avoiding certain foods, practicing good oral hygiene, and attending follow-up appointments.
Advanced Techniques in Oral Wound Healing
In recent years, advancements in medical technology and research have led to the development of innovative techniques that enhance oral wound healing outcomes. These techniques can significantly expedite the healing process and improve the overall quality of tissue regeneration.
Growth Factors and Biologics
Growth factors are natural proteins that play a vital role in cell growth, proliferation, and tissue regeneration. Researchers have explored the use of growth factors, such as platelet-derived growth factor (PDGF) and transforming growth factor-beta (TGF-β), to accelerate oral wound healing. These growth factors can be applied topically or incorporated into biocompatible scaffolds to promote targeted tissue regeneration.
Tissue Engineering and Regenerative Scaffolds
Tissue engineering involves the use of biomaterials and scaffolds to create an environment that supports cell growth and tissue regeneration. In oral wound healing, various biocompatible materials, such as collagen and hydrogels, can be used as scaffolds to facilitate the formation of new tissue. These scaffolds can be engineered to release growth factors or other bioactive molecules, providing a controlled and optimized healing environment.
Laser Therapy
Laser therapy, specifically low-level laser therapy (LLLT), has gained attention for its potential to enhance wound healing. LLLT uses low-intensity lasers or light-emitting diodes to stimulate cellular activity and improve blood circulation at the wound site. This non-invasive approach can accelerate wound closure, reduce inflammation, and alleviate pain.
Platelet-Rich Plasma (PRP)
Platelet-rich plasma (PRP) is a regenerative technique that involves isolating and concentrating platelets from the patient’s own blood. These platelets are rich in growth factors and cytokines that promote tissue repair. PRP can be applied directly to oral wounds to stimulate healing and enhance the formation of new tissue.
3D Printing and Bioprinting
Three-dimensional (3D) printing and bioprinting have revolutionized the field of tissue engineering and wound healing. Researchers can create intricate structures and custom-designed implants using biocompatible materials and cells. In oral wound healing, 3D-printed scaffolds can be tailored to match the patient’s anatomy, providing a precise and effective platform for tissue regeneration.
Nanotechnology
Nanotechnology involves manipulating materials at the nanoscale to create novel therapeutic approaches. Nanoparticles can be engineered to deliver drugs, growth factors, or antimicrobial agents directly to the wound site. This targeted delivery enhances the therapeutic effect while minimizing potential side effects.
Future Directions and Challenges
While these advanced techniques show great promise, challenges still exist in translating these innovations from the laboratory to clinical practice. Regulatory approvals, cost considerations, and long-term safety assessments are important factors that need to be addressed. Additionally, patient-specific factors, such as individual variability in wound healing response, must be taken into account when implementing these techniques.
Research in the field of oral wound healing continues to evolve, with ongoing studies focusing on improving our understanding of cellular interactions, immune responses, and the molecular mechanisms that drive the healing process. Collaborations between clinicians, researchers, and engineers are crucial for developing effective and practical solutions that can be seamlessly integrated into clinical practice.
Conclusion
Oral wound healing is a complex process that involves intricate interactions between cells, growth factors, and various physiological systems. Understanding the phases of wound healing and the factors that influence the process is essential for healthcare providers and patients alike. By promoting a comprehensive approach to wound care, individuals can optimize their chances of a successful and timely recovery, ultimately leading to improved oral health and overall well-being.