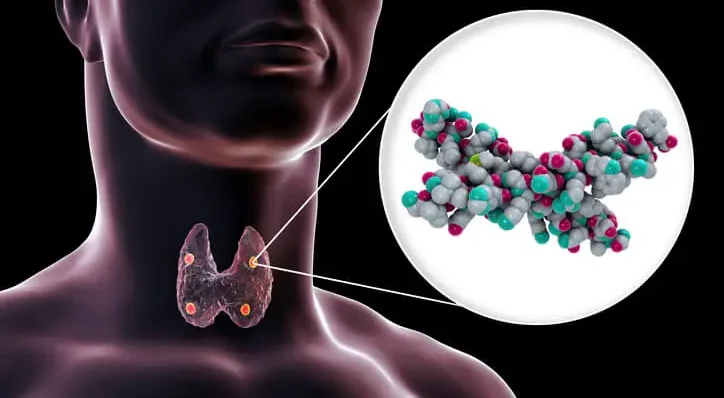
Hyperparathyroidism is a condition characterized by the excessive production of parathyroid hormone (PTH) by the parathyroid glands. These four small glands, located behind the thyroid gland in the neck, play a crucial role in regulating calcium levels in the blood. PTH increases calcium levels by stimulating the release of calcium from bones, increasing calcium absorption in the intestines, and reducing calcium excretion by the kidneys. When PTH levels become abnormally high, it can lead to a variety of systemic effects, including significant dental implications. This article explores the pathophysiology of hyperparathyroidism, its general systemic effects, and its specific impact on dental health and treatment.
Table of Contents
TogglePathophysiology of Hyperparathyroidism
Hyperparathyroidism is classified into three types: primary, secondary, and tertiary.
Primary Hyperparathyroidism
This occurs when there is an inherent problem with the parathyroid glands themselves, usually due to a benign tumor (adenoma) or hyperplasia (enlargement) of the glands. The excessive secretion of PTH leads to hypercalcemia (elevated blood calcium levels).
Secondary Hyperparathyroidism
This is a compensatory response to chronic hypocalcemia (low blood calcium levels), often due to conditions such as chronic kidney disease or vitamin D deficiency. In this case, the parathyroid glands enlarge and secrete more PTH in an attempt to increase blood calcium levels.
Tertiary Hyperparathyroidism
This occurs when secondary hyperparathyroidism becomes autonomous and excessive, often after long-standing secondary hyperparathyroidism. This can happen in patients with chronic kidney disease who have undergone kidney transplantation.
Systemic Effects of Hyperparathyroidism
The excessive secretion of PTH and the resultant hypercalcemia in primary hyperparathyroidism or the complex metabolic alterations in secondary and tertiary hyperparathyroidism lead to a variety of systemic effects, including:
- Skeletal Effects
- Renal Effects
- Gastrointestinal Effects
- Neuromuscular Effects
- Cardiovascular Effects
Skeletal Effects
PTH stimulates osteoclast activity, leading to increased bone resorption. This can result in bone pain, osteopenia, osteoporosis, and an increased risk of fractures.
Renal Effects
Hypercalcemia can lead to nephrolithiasis (kidney stones) and nephrocalcinosis (calcification of the kidneys). In chronic cases, renal insufficiency or failure can occur.
Gastrointestinal Effects
Patients may experience nausea, vomiting, abdominal pain, peptic ulcers, and pancreatitis due to hypercalcemia.
Neuromuscular Effects
Hypercalcemia can cause muscle weakness, fatigue, depression, confusion, and even coma in severe cases.
Cardiovascular Effects
Hypercalcemia can lead to hypertension, arrhythmias, and calcification of cardiac and vascular tissues.
Dental Implications of Hyperparathyroidism
The dental manifestations of hyperparathyroidism are significant and can often be the first indicators of the condition. Dentists play a crucial role in early diagnosis and management of this condition. Here are some key dental implications:
- Oral Bone Changes
- Dental Mobility and Malocclusion
- Periodontal Disease
- Delayed Tooth Eruption
- Soft Tissue Calcifications
- Xerostomia
Oral Bone Changes
Increased osteoclastic activity due to elevated PTH can lead to changes in the jawbones, particularly the mandible. Radiographic examinations may reveal a “ground glass” appearance, loss of lamina dura, and a decrease in bone density. Brown tumors (osteitis fibrosa cystica) can also develop, which are osteolytic lesions that appear as radiolucencies on X-rays and may cause facial swelling and jaw deformities.
Dental Mobility and Malocclusion
The reduction in bone density and structural integrity can lead to loosening of teeth, increased mobility, and potential malocclusion. Patients may report changes in their bite or difficulties with chewing.
Periodontal Disease
The altered bone metabolism and decreased bone density make patients more susceptible to periodontal disease. There may be rapid progression of periodontal pockets, gingival recession, and tooth loss.
Delayed Tooth Eruption
In children and adolescents, hyperparathyroidism can cause delayed eruption of teeth. This can lead to misalignment and occlusion issues, requiring orthodontic intervention.
Soft Tissue Calcifications
Hypercalcemia can lead to calcifications in the soft tissues of the oral cavity, including the salivary glands. This can present as sialolithiasis (salivary gland stones) causing pain and swelling, particularly when eating.
Xerostomia
Patients with hyperparathyroidism may experience xerostomia (dry mouth), which can increase the risk of dental caries, oral infections, and mucosal lesions. This is often a secondary effect due to medication or associated conditions like renal failure.
Diagnosis and Management in Dental Practice
Dentists should be vigilant for signs of hyperparathyroidism during routine examinations, especially in patients presenting with unexplained oral symptoms or radiographic anomalies. The diagnostic process involves:
- Medical History and Clinical Examination
- Radiographic Analysis
- Laboratory Tests
Medical History and Clinical Examination
Detailed medical history should be taken to identify any symptoms or conditions that may suggest hyperparathyroidism. Clinical examination of the oral cavity, teeth, and jaws is essential.
Radiographic Analysis
Panoramic and periapical radiographs can reveal bone density changes, loss of lamina dura, and presence of osteolytic lesions. Advanced imaging techniques like cone-beam computed tomography (CBCT) may be utilized for detailed assessment.
Laboratory Tests
If hyperparathyroidism is suspected, referral for laboratory tests including serum calcium, PTH levels, and renal function tests is crucial for diagnosis and differentiation of the type of hyperparathyroidism.
Dental Management Strategies
Management of dental patients with hyperparathyroidism involves a multidisciplinary approach, considering both the dental and medical aspects of the condition. Key strategies include:
- Pre-treatment Planning
- Preventive Care
- Periodontal Therapy
- Management of Tooth Mobility
- Orthodontic Considerations
- Monitoring and Follow-up
Pre-treatment Planning
Prior to any dental treatment, a thorough assessment and stabilization of the patient’s systemic condition is essential. Collaboration with the patient’s endocrinologist or primary care physician is recommended to ensure optimal management of PTH levels and calcium homeostasis.
Preventive Care
Emphasis on preventive dental care is crucial. This includes regular dental check-ups, professional cleanings, and patient education on maintaining good oral hygiene. Use of fluoride treatments and remineralizing agents can help reduce the risk of dental caries and tooth decay.
Periodontal Therapy
Aggressive management of periodontal disease is necessary due to the increased susceptibility. Non-surgical treatments such as scaling and root planing, along with adjunctive therapies like antimicrobial agents, may be employed. In advanced cases, surgical intervention may be required.
Management of Tooth Mobility
For patients with significant tooth mobility, splinting of teeth may be considered to stabilize the dentition and improve function. In cases of severe bone loss, bone grafting and regenerative procedures might be necessary.
Orthodontic Considerations
In younger patients with delayed tooth eruption or malocclusion, orthodontic evaluation and treatment planning are important. Coordination with orthodontists to manage these patients effectively is essential.
Monitoring and Follow-up
Regular monitoring of the patient’s oral and systemic health is crucial. Dentists should maintain close communication with the patient’s healthcare team to monitor any changes in the patient’s condition and adjust dental treatment plans accordingly.
Conclusion
Hyperparathyroidism is a complex endocrine disorder with significant systemic and dental implications. Dental professionals play a vital role in the early detection and management of this condition. By understanding the pathophysiology, recognizing the oral manifestations, and implementing appropriate dental management strategies, dentists can significantly contribute to the overall health and well-being of patients with hyperparathyroidism. Multidisciplinary collaboration and a patient-centered approach are key to achieving optimal outcomes in these patients.
Frequently Asked Questions about Hyperparathyroidism
Is hyperparathyroidism life-threatening?
Hyperparathyroidism is not usually immediately life-threatening, but if it goes untreated for a long period, it can become dangerous. Persistently high calcium levels caused by overactive parathyroid glands can lead to serious long-term health problems, including osteoporosis (weakened bones), kidney stones, chronic kidney disease, high blood pressure, heart rhythm problems, and even stroke. In rare and extreme cases, a condition called hypercalcemic crisis—marked by dangerously high calcium levels—can become a medical emergency. With early diagnosis and proper treatment, however, most complications can be avoided and the condition can be effectively managed or cured.
What are the symptoms of parathyroid disease?
Parathyroid disease, especially hyperparathyroidism, can produce a wide range of symptoms that often develop gradually and may be mistaken for aging or other conditions. Common symptoms include:
- Chronic fatigue or low energy
- Muscle weakness
- Depression, anxiety, or mood swings
- Joint or bone pain (especially in the arms, legs, or back)
- Osteoporosis or frequent fractures
- Abdominal pain, bloating, or ulcers
- Nausea, constipation, or loss of appetite
- Frequent urination and excessive thirst
- Kidney stones
- Poor concentration, confusion, or memory problems (“brain fog”)
Some people experience only mild or vague symptoms, while others have multiple severe symptoms that significantly affect quality of life.
What foods should people with hyperparathyroidism avoid?
Diet doesn’t cause hyperparathyroidism, but it can impact how the disease affects your body. If you have high calcium levels, you may be advised to avoid or limit:
- High-calcium foods like milk, cheese, yogurt, and fortified plant-based milks
- Calcium supplements, unless specifically prescribed
- High-phosphorus foods, such as red meats, organ meats, processed foods, and colas
- High-sodium foods, including salty snacks, canned soups, and fast food, which can cause more calcium loss in urine
Staying hydrated and following a balanced, kidney-friendly diet can help support your overall health while managing hyperparathyroidism. Always consult your healthcare provider or a dietitian before making major dietary changes.
Can hyperparathyroidism be cured?
Yes, primary hyperparathyroidism is most often cured by a surgical procedure called parathyroidectomy, where the overactive gland(s) are removed. It has a high success rate—over 95% when performed by experienced surgeons.
Secondary hyperparathyroidism, typically associated with kidney disease or vitamin D deficiency, is more complex and often requires medical management, including medications like vitamin D analogs, phosphate binders, or even dialysis. In some cases, surgery may still be needed if medical treatment fails.
Early diagnosis improves the chances of successful treatment and reversal of symptoms.
What is the life expectancy of someone with hyperparathyroidism?
When properly treated, especially through surgery for primary hyperparathyroidism, life expectancy is usually normal or close to normal. However, untreated or poorly managed hyperparathyroidism can lead to significant long-term health issues such as fractures, kidney damage, and cardiovascular complications, which can reduce quality of life and lifespan. Prompt treatment and regular monitoring are key to maintaining health and longevity.
How do you feel when you have hyperparathyroidism?
Many people with hyperparathyroidism feel chronically tired or “run down.” Common experiences include:
- Feeling mentally foggy or forgetful
- Difficulty focusing
- Low motivation or energy
- Achy bones or muscles
- Irritability or emotional sensitivity
- A general sense of being unwell
Patients often describe it as feeling older than they are, or not feeling like themselves anymore. Many report significant improvement in mood and energy after treatment.
Does parathyroid disease affect weight?
Parathyroid disease doesn’t directly cause weight gain or weight loss. However, it can indirectly affect weight through symptoms like fatigue, reduced activity, and changes in appetite. Some people may gain weight due to inactivity or emotional eating linked to mood swings, while others may lose weight due to nausea or poor appetite. Hormonal imbalances can also subtly affect metabolism, but more research is needed in this area.
How do you feel when your calcium is high?
High blood calcium (hypercalcemia) can produce a range of symptoms, including:
- Fatigue and weakness
- Nausea and vomiting
- Constipation
- Frequent urination and dehydration
- Confusion or difficulty thinking clearly
- Muscle cramps or twitches
- Abdominal pain or discomfort
- Headaches or dizziness
In more serious cases, very high calcium levels can cause irregular heartbeats or even coma. These symptoms often improve quickly once calcium levels return to normal.
What personality changes occur with hyperparathyroidism?
Many patients report emotional and cognitive changes such as:
- Increased irritability or impatience
- Episodes of depression or anxiety
- Mood swings that seem disproportionate
- Loss of interest in activities or social withdrawal
- Forgetfulness or mental fog
These changes can be subtle or quite profound. They’re often misdiagnosed as depression, anxiety disorders, or even early dementia until calcium and parathyroid hormone levels are tested.
What triggers hyperparathyroidism?
The causes differ by type:
- Primary hyperparathyroidism is usually caused by a benign adenoma (tumor) on one of the four parathyroid glands. Less commonly, it’s due to gland hyperplasia (enlargement) or cancer.
- Secondary hyperparathyroidism is most often caused by chronic kidney disease, which disrupts calcium and phosphorus balance, or vitamin D deficiency.
- Tertiary hyperparathyroidism can occur after long-standing secondary hyperparathyroidism when the glands become permanently overactive.
Some genetic disorders, radiation exposure, and certain medications can also contribute.
Should I take vitamin D if I have parathyroid disease?
Vitamin D levels must be carefully managed in people with parathyroid disease. In many cases of primary hyperparathyroidism, vitamin D is low, and replacing it (cautiously) can help normalize parathyroid hormone levels and reduce bone loss. However, too much vitamin D can raise calcium levels, potentially worsening symptoms or causing complications.
Never self-prescribe vitamin D—always follow your healthcare provider’s guidance on whether supplementation is appropriate for your specific case.
Does parathyroid disease affect your eyes?
Yes, indirectly. Chronically elevated calcium levels can lead to calcification in the eyes, most commonly seen as band keratopathy (calcium deposits on the cornea). Other potential effects include:
- Blurry vision
- Dry or irritated eyes
- Cataracts (clouding of the lens, sometimes linked to long-term calcium imbalance)
While eye symptoms are less common, they can be a part of the overall picture in longstanding, untreated hyperparathyroidism.