Anemia, a condition characterized by a deficiency of red blood cells or hemoglobin, is a common yet often overlooked health issue that can have significant implications in dental care. For dental professionals, understanding the complexities of anemia is crucial for providing comprehensive and safe patient care. This article delves into the various aspects of anemia, its relevance in dentistry, and the best practices for managing anemic patients in a dental setting.
Table of Contents
ToggleUnderstanding Anemia
Anemia can be broadly classified into several types based on the underlying cause:
- Iron Deficiency Anemia (IDA)
- Vitamin Deficiency Anemias
- Hemolytic Anemias
- Aplastic Anemia
- Sickle Cell Anemia
Iron Deficiency Anemia (IDA)
The most common form, resulting from a lack of iron which is essential for hemoglobin production.
Vitamin Deficiency Anemias
These include pernicious anemia caused by a deficiency in vitamin B12, and folate-deficiency anemia.
Hemolytic Anemias
Result from the destruction of red blood cells faster than they can be produced.
Aplastic Anemia
Caused by the inability of the bone marrow to produce sufficient red blood cells.
Sickle Cell Anemia
A hereditary form that results in abnormally shaped red blood cells.
Each type of anemia presents unique challenges in a dental context, necessitating tailored approaches to treatment and patient management.
Anemia Symptoms
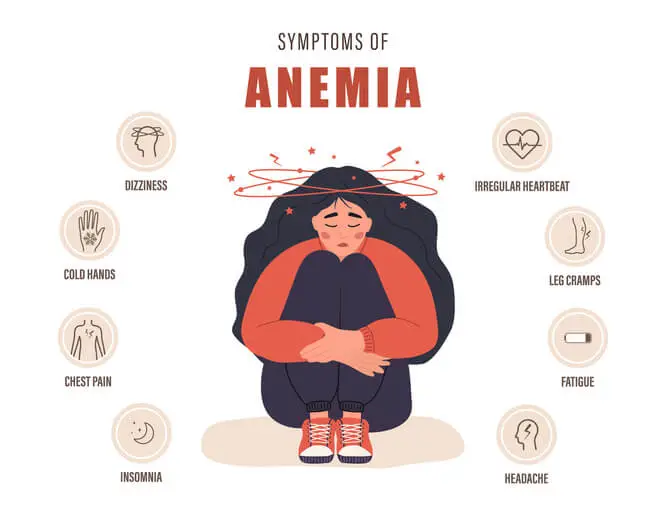
Here are some common symptoms of anemia:
General Symptoms
- Fatigue – Feeling tired or weak is one of the most common symptoms.
- Weakness – Experiencing muscle weakness.
- Pale or Yellowish Skin – Paleness in the face or other areas can indicate anemia.
- Shortness of Breath – Feeling short of breath, especially with physical activity.
- Dizziness or Lightheadedness – Feeling dizzy or lightheaded, especially when standing up.
- Cold Hands and Feet – Experiencing cold extremities.
- Chest Pain – Sometimes anemia can cause chest pain, especially if it is severe.
- Headaches – Frequent headaches can be a symptom.
- Irregular Heartbeats – Also known as arrhythmia or palpitations.
Specific Symptoms Based on Type of Anemia
- Iron-Deficiency Anemia: Craving for non-nutritive substances such as ice, dirt, or starch (a condition known as pica), brittle nails, swelling or soreness of the tongue, cracks in the sides of the mouth, and an enlarged spleen.
- Vitamin B12 Deficiency Anemia: Numbness or tingling in the hands and feet, difficulty walking, memory loss, and a swollen, inflamed tongue.
- Folate-Deficiency Anemia: Irritability, diarrhea, and a smooth tongue.
- Hemolytic Anemia: Symptoms may include dark urine, jaundice (yellow skin and eyes), and pain in the abdomen.
- Aplastic Anemia: Can cause a high risk of infections and unexplained or easy bruising and bleeding.
Severe Anemia Symptoms
- Extreme Fatigue – Feeling exhausted despite rest.
- Fainting – Passing out or feeling like you might pass out.
- Severe Shortness of Breath – Difficulty breathing even while resting.
Oral Manifestations of Anemia
Anemia often manifests in the oral cavity, sometimes serving as an early indicator of the condition. Common oral signs and symptoms include:
- Pallor of the Oral Mucosa
- Atrophic Glossitis
- Angular Cheilitis
- Recurrent Aphthous Stomatitis (RAS)
- Periodontal Disease
Pallor of the Oral Mucosa
Reduced hemoglobin levels lead to a pale appearance of the gums and mucous membranes.
Atrophic Glossitis
Characterized by a smooth, glossy tongue due to the loss of papillae, often seen in iron and vitamin B12 deficiencies.
Angular Cheilitis
Cracks and sores at the corners of the mouth, commonly associated with iron deficiency anemia.
Recurrent Aphthous Stomatitis (RAS)
Frequent, painful mouth ulcers that can be linked to nutritional deficiencies.
Periodontal Disease
Anemia can exacerbate conditions like gingivitis and periodontitis due to impaired immune response and reduced oxygen supply to the tissues.
Understanding these manifestations helps in the early detection and management of anemia in dental patients.
Considerations for Dental Management of Anemic Patients
- Pre-Treatment Assessment
- Hemostasis and Bleeding Risk
- Infection Control
- Pain Management
- Nutritional Counseling
- Oral Hygiene and Preventive Care
Pre-Treatment Assessment
Before initiating dental treatment, a thorough medical history and assessment are imperative. This includes:
- Medical History Review
- Blood Tests
- Consultation with Physician
Medical History Review
Identifying underlying causes of anemia, current medications, and any history of blood transfusions.
Blood Tests
Hemoglobin levels, complete blood count (CBC), and iron studies to gauge the severity and type of anemia.
Consultation with Physician
For patients with severe anemia or complex medical histories, liaising with their primary care physician or hematologist is crucial.
Hemostasis and Bleeding Risk
Patients with anemia, particularly those with hemolytic or aplastic types, may have compromised hemostasis. Dental procedures, especially those involving surgery or extractions, require careful planning:
- Preoperative Hemoglobin Levels
- Local Hemostatic Measures
- Minimally Invasive Techniques
Preoperative Hemoglobin Levels
Ensuring hemoglobin levels are stable and within a safe range before invasive procedures.
Local Hemostatic Measures
Use of local anesthesia with vasoconstrictors, hemostatic agents like gelatin sponges, and sutures to control bleeding.
Minimally Invasive Techniques
Opting for less invasive procedures when possible to reduce bleeding risk.
Infection Control
Anemic patients, especially those with severe forms like aplastic anemia, are at increased risk of infections due to compromised immune function:
- Antibiotic Prophylaxis
- Strict Aseptic Techniques
Antibiotic Prophylaxis
May be required for invasive procedures in immunocompromised patients.
Strict Aseptic Techniques
Ensuring a sterile environment and proper aseptic protocols during procedures.
Pain Management
Effective pain management is crucial, but it must be balanced with the patient’s overall health status:
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
- Acetaminophen
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Caution is advised as they can exacerbate gastrointestinal bleeding, especially in iron deficiency anemia.
Acetaminophen
Often preferred for pain relief due to its minimal impact on bleeding.
Nutritional Counseling
For anemic patients, especially those with nutritional deficiencies, dental professionals can play a role in dietary counseling:
- Iron-Rich Foods
- Vitamin B12 and Folate
Iron-Rich Foods
Encouraging consumption of iron-rich foods such as red meat, leafy greens, and fortified cereals.
Vitamin B12 and Folate
Emphasizing the importance of dairy products, eggs, and green vegetables.
Oral Hygiene and Preventive Care
Maintaining optimal oral hygiene is critical for anemic patients to prevent infections and complications:
- Regular Dental Visits
- Home Care Regimen
Regular Dental Visits
Ensuring frequent check-ups and cleanings to monitor oral health.
Home Care Regimen
Reinforcing the importance of brushing, flossing, and possibly the use of antimicrobial mouth rinses.
Special Considerations for Specific Types of Anemia
Iron Deficiency Anemia
Patients with IDA often present with glossitis, angular cheilitis, and pallor. Management includes:
- Iron Supplementation
- Avoiding Trauma
Iron Supplementation
Advising on iron supplements if prescribed by their physician.
Avoiding Trauma
Gentle handling during dental procedures to avoid exacerbating mucosal lesions.
Vitamin B12 and Folate Deficiency Anemia
These patients may present with glossitis and recurrent ulcers. Dental care includes:
- Monitoring Oral Health
- Coordination with Medical Care
Monitoring Oral Health
Frequent checks for signs of glossitis and ulcers.
Coordination with Medical Care
Ensuring they are receiving appropriate vitamin supplementation.
Sickle Cell Anemia
Patients with sickle cell anemia require special attention due to the risk of vaso-occlusive crises and infections:
- Stress Management
- Hydration
- Avoiding Hypoxia
Stress Management
Minimizing stress and ensuring a pain-free experience to avoid triggering a crisis.
Hydration
Encouraging adequate hydration before and after dental procedures.
Avoiding Hypoxia
Using pulse oximetry to monitor oxygen saturation during procedures.
Hemolytic and Aplastic Anemia
Patients with these types of anemia are prone to infections and bleeding complications:
- Strict Infection Control
- Hemostatic Precautions
Strict Infection Control
Using prophylactic antibiotics if necessary.
Hemostatic Precautions
Employing meticulous hemostatic techniques and close monitoring post-procedure.
Emergency Management
Dental emergencies in anemic patients require prompt and careful handling:
- Bleeding: Immediate use of local hemostatic agents and possibly systemic medications.
- Infection: Rapid administration of appropriate antibiotics.
- Pain: Judicious use of analgesics, avoiding those that exacerbate bleeding.
Frequently Asked Questions (FAQs)
What are safety considerations for anemia?
Individuals with anemia should be cautious of dizziness, fatigue, shortness of breath, and an increased risk of fainting. Since anemia can lead to reduced oxygen transport throughout the body, those affected should avoid strenuous activities that may worsen their symptoms. It is essential to stay hydrated, eat a balanced diet rich in iron, vitamin B12, and folate, and follow any prescribed treatment plan. In cases of severe anemia, individuals should be cautious when standing up quickly to avoid dizziness and potential falls.
Can you go to the dentist with anemia?
Yes, anemic individuals can visit the dentist, but it is important to inform the dental professional about the condition beforehand. Depending on the severity of anemia, special precautions may be needed. For example, patients with significant anemia may require supplemental oxygen during treatment or a modified treatment plan to reduce excessive blood loss. If undergoing a procedure that involves bleeding, such as extractions or gum surgery, the dentist may monitor clotting ability and recommend iron supplements or other interventions to ensure safe healing.
What are the dental considerations for aplastic anemia?
Aplastic anemia is a serious condition in which the bone marrow fails to produce sufficient blood cells, leading to a weakened immune system and increased bleeding risk. In dental care, this means that patients may be more prone to infections, have delayed healing after procedures, and experience excessive bleeding. Dentists may need to take extra precautions, such as using antimicrobial mouth rinses to prevent infections, prescribing prophylactic antibiotics, and avoiding invasive procedures unless absolutely necessary. Close coordination with the patient’s physician is often required to ensure safe dental care.
What are oral implications of anemia?
Anemia can manifest in several ways in the oral cavity. Common symptoms include pale gums and mucosa due to reduced red blood cell levels, glossitis (inflammation of the tongue) causing discomfort and a smooth, swollen appearance, and atrophic changes in oral tissues leading to increased sensitivity. Individuals with anemia may also experience frequent mouth ulcers, delayed wound healing, and an increased risk of oral infections due to weakened immunity. Additionally, a burning sensation in the mouth, particularly in the tongue, is commonly reported in anemic individuals.
What is the dental consideration of iron deficiency anemia?
Iron deficiency anemia can present with multiple oral symptoms, including atrophic glossitis (a smooth, swollen tongue), angular cheilitis (cracking at the corners of the mouth), and increased oral ulceration. Patients may also complain of a burning sensation in the tongue and increased susceptibility to oral candidiasis (fungal infections). Dentists should be aware of these symptoms and encourage patients to follow a well-balanced diet with iron-rich foods or supplements as prescribed by their physician. If oral manifestations are severe, dentists may refer patients to a medical provider for further evaluation of potential underlying causes.
What should anemic people avoid doing?
Anemic individuals should avoid activities that could lead to excessive fatigue or exacerbate their symptoms, such as high-intensity workouts or prolonged standing without support. Sudden changes in position should be avoided to prevent dizziness and fainting. Additionally, they should limit their intake of tea, coffee, and calcium-rich foods during meals, as these can inhibit iron absorption. Alcohol and smoking should also be minimized as they can contribute to further health complications. Seeking medical attention when experiencing symptoms such as extreme fatigue, rapid heartbeat, or shortness of breath is essential.
Can dental disease cause anemia?
Yes, dental disease can contribute to anemia in certain cases. Chronic periodontal disease, oral infections, and untreated dental issues can lead to prolonged inflammation and slow but persistent blood loss, potentially resulting in iron deficiency anemia. Additionally, individuals with severe gum disease may have difficulty eating nutritious foods, leading to deficiencies that worsen anemia. Proper oral hygiene, regular dental check-ups, and timely treatment of dental infections can help prevent this risk.
Do gums bleed with anemia?
Yes, anemia can cause gum bleeding, particularly due to weakened blood vessels and reduced platelet function, which are essential for blood clotting. Individuals with anemia may notice that their gums bleed more easily when brushing or flossing, even if they do not have gum disease. If bleeding gums persist, it is essential to consult a dentist to rule out underlying periodontal disease and a physician to assess anemia severity and treatment options.
Conclusion
Anemia presents a myriad of challenges in dental care, from managing bleeding risks to preventing infections and ensuring adequate pain control. A comprehensive understanding of the various types of anemia and their oral manifestations is essential for dental professionals. By conducting thorough assessments, liaising with medical colleagues, and employing meticulous clinical practices, dental professionals can provide safe and effective care for anemic patients. This holistic approach not only addresses the immediate dental concerns but also contributes to the overall well-being of the patient.