Gingivectomy is a surgical procedure involving the removal of gum tissue (gingiva). It is primarily performed to treat gum disease or to remove overgrown gum tissue that may be caused by various factors, including certain medications, systemic diseases, or poor oral hygiene. This article delves into the purpose, procedure, recovery, and benefits of gingivectomy, alongside considerations and potential complications.
Table of Contents
TogglePurpose of Gingivectomy
Gingivectomy is performed for both therapeutic and cosmetic reasons. The primary purposes include:
- Treatment of Gum Disease
- Gingival Hyperplasia Management
- Cosmetic Improvement
Treatment of Gum Disease
Gingivectomy is often used to treat periodontal disease, a severe form of gum disease that can lead to tooth loss if not properly managed. By removing diseased gum tissue, the procedure helps reduce the depth of periodontal pockets, making it easier to maintain oral hygiene and prevent further infection.
Gingival Hyperplasia Management
Gingival hyperplasia, or gum overgrowth, can be caused by certain medications such as anticonvulsants, immunosuppressants, and calcium channel blockers. Overgrown gums can cover teeth partially or entirely, creating a breeding ground for bacteria and making oral hygiene challenging. Gingivectomy removes the excess tissue, improving both oral health and aesthetics.
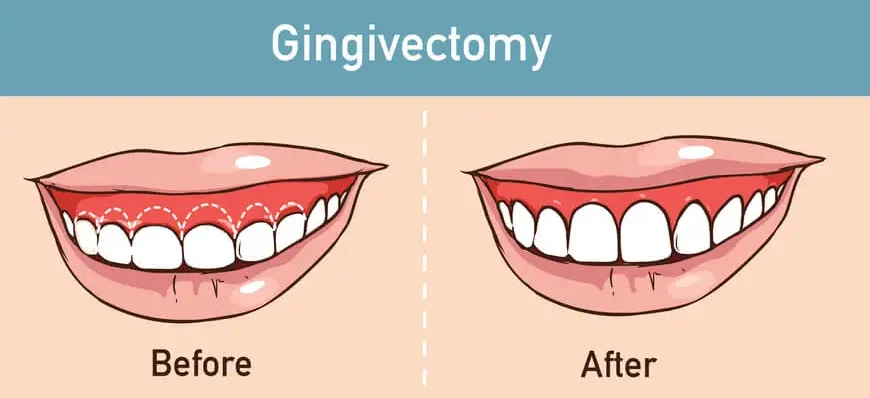
Cosmetic Improvement
In cases where excessive gum tissue affects the appearance of a smile, a gingivectomy can be performed to sculpt and contour the gum line, resulting in a more attractive and proportionate smile.
Indications for Gingivectomy
Gingivectomy is indicated in various scenarios, including:
- Chronic Periodontitis
- Drug-Induced Gingival Overgrowth
- Hereditary Gingival Fibromatosis
- Aesthetic Concerns
Chronic Periodontitis
When nonsurgical treatments such as scaling and root planing fail to control periodontal pockets, gingivectomy becomes necessary.
Drug-Induced Gingival Overgrowth
Medications like phenytoin, cyclosporine, and nifedipine can cause significant gum overgrowth that may require surgical intervention.
Hereditary Gingival Fibromatosis
A rare condition characterized by the excessive growth of gingival tissues, often necessitating surgical removal for functional and aesthetic reasons.
Aesthetic Concerns
Individuals seeking to improve the appearance of their gums for a more balanced smile.
Gingivectomy Procedure
Gingivectomy procedure can be performed using different techniques, including traditional surgical methods with a scalpel, electrosurgery, or laser surgery. Here’s a step-by-step overview of the traditional gingivectomy process:
Pre-Operative Preparation
- Clinical Assessment
- Informed Consent
- Oral Hygiene Instructions
Clinical Assessment
A thorough oral examination and medical history review are essential to determine the suitability of the patient for the procedure. Diagnostic tools such as dental X-rays and periodontal charting are used to assess the extent of the gum disease or overgrowth.
Informed Consent
Patients are informed about the procedure, its benefits, risks, and post-operative care. Obtaining informed consent is a crucial step in the pre-operative process.
Oral Hygiene Instructions
Patients are often advised to maintain optimal oral hygiene before the procedure to reduce the risk of post-operative infections.
Anesthesia
Local anesthesia is administered to numb the area where the gingivectomy will be performed. In some cases, sedation may be used for patients with dental anxiety or for extensive procedures.
Surgical Procedure
- Incision and Tissue Removal
- Reshaping and Contouring
- Hemostasis
- Application of Surgical Dressing
Incision and Tissue Removal
The surgeon makes incisions in the gum tissue to remove the diseased or excess tissue. The incisions are typically made using a scalpel, although lasers or electrosurgical units may also be employed for precision and reduced bleeding.
Reshaping and Contouring
After the removal of the targeted gum tissue, the remaining gingiva is reshaped and contoured to ensure a natural and aesthetically pleasing appearance.
Hemostasis
Bleeding is controlled using various methods such as pressure, sutures, or electrocautery. Hemostasis is crucial to ensure a clean surgical field and promote healing.
Application of Surgical Dressing
A periodontal dressing may be applied to protect the surgical site and aid in healing. This dressing also helps to minimize discomfort and control bleeding.
Post-Operative Care and Recovery
Proper post-operative care is vital for a successful recovery following a gingivectomy. Patients are typically provided with detailed instructions, which may include:
- Pain Management
- Oral Hygiene
- Diet
- Activity Restrictions
- Follow-Up Appointments
Pain Management
Over-the-counter pain relievers such as ibuprofen or acetaminophen are often recommended to manage post-operative pain. In some cases, prescription medications may be necessary.
Oral Hygiene
Patients are advised to follow a gentle oral hygiene routine to prevent infection and promote healing. This may involve the use of antimicrobial mouth rinses and soft-bristled toothbrushes.
Diet
A soft diet is recommended for the first few days post-surgery to avoid irritation of the surgical site. Patients should avoid hot, spicy, or hard foods that could disrupt the healing process.
Activity Restrictions
Strenuous activities and heavy lifting should be avoided for a few days to reduce the risk of bleeding and swelling.
Follow-Up Appointments
Regular follow-up visits are scheduled to monitor the healing process and address any concerns or complications that may arise.
Benefits of Gingivectomy
Gingivectomy offers numerous benefits, both functional and aesthetic:
- Improved Oral Health
- Enhanced Aesthetics
- Better Functionality
- Reduced Risk of Complications
Improved Oral Health
By removing diseased or overgrown gum tissue, gingivectomy helps reduce periodontal pocket depths, making it easier to clean teeth and gums, thereby preventing further disease progression.
Enhanced Aesthetics
The procedure can significantly improve the appearance of the gums and smile, boosting the patient’s confidence and self-esteem.
Better Functionality
Removing excess gum tissue can enhance the functionality of the teeth and gums, making it easier to chew and speak.
Reduced Risk of Complications
Addressing gum disease and overgrowth early on can prevent more severe complications such as tooth loss and bone loss.
Potential Complications and Risks
While gingivectomy is generally considered a safe procedure, it is not without potential risks and complications, including:
- Infection
- Bleeding
- Pain and Discomfort
- Swelling
- Recurrence of Gum Disease or Overgrowth
- Aesthetic Concerns
Infection
Despite precautions, there is always a risk of infection following any surgical procedure. Proper oral hygiene and post-operative care are crucial to minimizing this risk.
Bleeding
Some bleeding is expected after a gingivectomy, but excessive or prolonged bleeding can be a concern. Patients should follow their surgeon’s instructions carefully to manage bleeding.
Pain and Discomfort
Pain and discomfort are common in the immediate post-operative period. Adequate pain management strategies should be employed to ensure patient comfort.
Swelling
Swelling of the gums and surrounding tissues is a normal response to surgery. Applying ice packs and following post-operative care instructions can help manage swelling.
Recurrence of Gum Disease or Overgrowth
Without proper oral hygiene and regular dental check-ups, there is a risk of recurrence of gum disease or gingival overgrowth.
Aesthetic Concerns
In some cases, the reshaped gum line may not meet the patient’s aesthetic expectations, necessitating further adjustments or procedures.
Frequently Asked Questions (FAQs)
How painful is gingivectomy?
Gingivectomy is typically performed under local anesthesia, so patients usually experience little to no pain during the procedure. After the anesthesia wears off, mild to moderate discomfort and sensitivity may occur, which can be managed with pain relievers and proper post-operative care.
Do gums grow back after gingivectomy?
No, gums do not fully grow back after a gingivectomy since the procedure involves the removal of excess gum tissue. However, the remaining gum tissue can heal and reshape over time, adapting to the new gum line.
How much will a gingivectomy cost?
The cost of a gingivectomy varies depending on factors like the extent of the procedure, the number of teeth involved, and the provider’s location. On average, it can range from $200 to $400 per tooth, but full-mouth procedures can cost significantly more.
What is the disadvantage of gingivectomy?
While gingivectomy can improve gum health and aesthetics, some potential disadvantages include post-operative discomfort, temporary sensitivity, risk of infection, and, in some cases, excessive gum removal leading to increased tooth sensitivity or aesthetic concerns.
How long does it take to heal from a gingivectomy?
Initial healing typically takes about one to two weeks, but complete recovery can take four to six weeks, depending on the extent of the procedure and individual healing rates. Proper oral hygiene and following post-operative instructions can aid the healing process.
Does insurance cover gingivectomy?
Insurance coverage for gingivectomy depends on whether it is deemed medically necessary. If the procedure is performed for gum disease treatment, it is often covered by dental insurance. However, if it is done for cosmetic purposes, insurance may not cover the costs. It’s best to check with your provider for specific coverage details.
Conclusion
Gingivectomy is a valuable procedure in the realm of periodontal therapy and cosmetic dentistry. It plays a crucial role in managing gum disease, addressing gingival overgrowth, and enhancing the overall appearance of the smile. While the procedure is generally safe and effective, proper patient selection, thorough pre-operative assessment, meticulous surgical technique, and diligent post-operative care are essential for achieving optimal outcomes.
Patients considering gingivectomy should consult with a qualified dental professional to discuss their specific needs and expectations. By understanding the purpose, procedure, benefits, and potential risks associated with gingivectomy, patients can make informed decisions and take proactive steps toward achieving and maintaining optimal oral health.