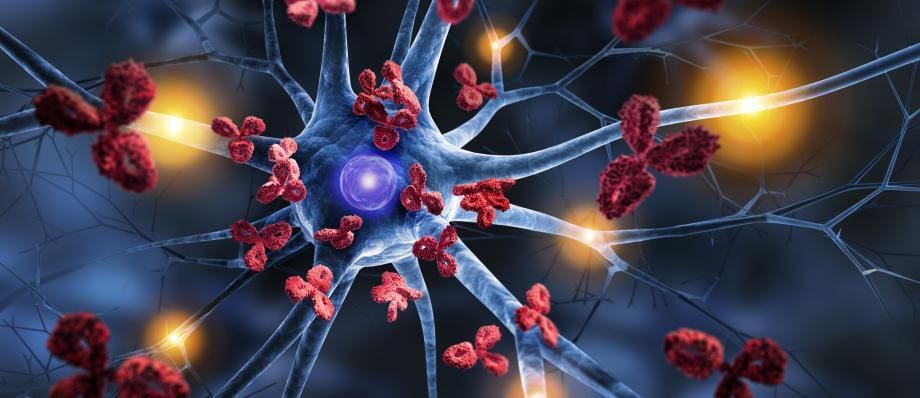
Autoimmune diseases are a diverse group of disorders characterized by an immune system that mistakenly attacks the body’s own cells and tissues. These conditions can affect various parts of the body, including the oral cavity and surrounding structures. In dentistry, understanding autoimmune diseases and their implications is essential for providing comprehensive care to affected individuals. This article delves into the relationship between autoimmune diseases and dentistry, highlighting key autoimmune conditions and their dental manifestations, the challenges faced in dental treatment, and strategies for managing oral health in individuals with autoimmune diseases.
Table of Contents
ToggleWhat are Autoimmune Diseases?
Autoimmune diseases result from a malfunction of the immune system, which mistakenly targets healthy cells and tissues, leading to inflammation, pain, and damage. The causes of autoimmune diseases are multifaceted, involving a complex interplay of genetic, environmental, and immunological factors. Some common autoimmune diseases include rheumatoid arthritis, lupus erythematosus, Sjögren’s syndrome, Crohn’s disease, and multiple sclerosis.
The manifestations of autoimmune diseases can vary widely, affecting virtually any part of the body, including joints, skin, organs, and mucous membranes. In dentistry, the focus is primarily on how autoimmune diseases impact oral health and the delivery of dental care.
Autoimmune Diseases and Their Dental Manifestations
- Sjögren’s Syndrome
- Rheumatoid Arthritis
- Systemic Lupus Erythematosus (SLE)
- Inflammatory Bowel Disease (IBD)
Sjögren’s Syndrome
Sjögren’s syndrome is an autoimmune disorder characterized by dryness of the mouth and eyes due to the immune system attacking the body’s moisture-producing glands. In dentistry, patients with Sjögren’s syndrome often present with xerostomia (dry mouth), which can result in increased susceptibility to dental caries, periodontal disease, and oral fungal infections. Dentists must address these issues by recommending frequent sips of water, sugar-free gum, and specialized oral hygiene products to mitigate the effects of dry mouth.
Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune disorder that primarily affects the joints, causing pain, inflammation, and stiffness. The temporomandibular joint (TMJ) can be impacted, leading to difficulty in chewing, jaw pain, and limited mouth opening. Dentists need to consider these challenges during dental treatments and may need to modify procedures or recommend exercises to improve jaw mobility and reduce discomfort for affected individuals.
Systemic Lupus Erythematosus (SLE)
Systemic lupus erythematosus is a systemic autoimmune disease that affects various organs, including the skin, joints, and kidneys. Oral manifestations can include ulcers, lesions, and tissue swelling. Moreover, medications used to manage SLE, such as corticosteroids and immunosuppressants, can impact oral health by increasing the risk of oral infections and delayed wound healing. Dental professionals need to work closely with rheumatologists to coordinate care and ensure appropriate management of these oral complications.
Inflammatory Bowel Disease (IBD)
Inflammatory bowel disease encompasses conditions like Crohn’s disease and ulcerative colitis, where the gastrointestinal tract is primarily affected. Patients with IBD may experience oral manifestations such as aphthous ulcers, gingivitis, and periodontitis. Dentists should collaborate with gastroenterologists to manage oral symptoms while considering the overall health and medication regimen of the patient.
Challenges in Dental Treatment of Patients with Autoimmune Diseases
Providing dental care to individuals with autoimmune diseases poses unique challenges. These challenges arise from the systemic nature of autoimmune conditions and the potential impact of medications used to manage them. Some common challenges include:
- Compromised Immune Function
- Medication Interactions
- Sensitivity to Pain and Stress
Compromised Immune Function
Many autoimmune diseases and their treatments compromise the immune system, making patients more susceptible to infections. Dentists must take extra precautions to prevent infections during dental procedures, ensuring a sterile environment and following appropriate infection control measures.
Medication Interactions
Patients with autoimmune diseases often take multiple medications to manage their condition. Some medications can have implications for dental treatment, such as increased bleeding tendencies or interactions with local anesthetics. Dentists need to be aware of the patient’s medication list and adjust treatment plans accordingly.
Sensitivity to Pain and Stress
Patients with autoimmune diseases may have heightened sensitivity to pain and stress due to their condition. Dentists should adopt strategies to minimize discomfort during dental procedures, such as utilizing gentle techniques, managing anxiety, and considering pain management options.
Strategies for Managing Oral Health in Individuals with Autoimmune Diseases
To address the unique needs of patients with autoimmune diseases, dental professionals can implement the following strategies:
- Comprehensive Health History and Consultation
- Individualized Treatment Plans
- Collaborative Care
- Patient Education
Comprehensive Health History and Consultation
Thoroughly reviewing the patient’s medical history and consulting with their healthcare team can provide valuable insights into their condition, medication regimen, and any specific considerations for dental treatment.
Individualized Treatment Plans
Tailoring dental treatment plans to accommodate the patient’s autoimmune condition, medication side effects, and overall health status is crucial. This may involve shorter treatment sessions, premedication protocols, and close monitoring during and after procedures.
Collaborative Care
Collaborating with other healthcare providers, such as rheumatologists, gastroenterologists, and immunologists, ensures a multidisciplinary approach to the patient’s care. Effective communication and information sharing facilitate coordinated treatment that considers both systemic health and oral health needs.
Patient Education
Educating patients about the potential oral manifestations of their autoimmune disease, the importance of good oral hygiene, and the necessity of regular dental check-ups empowers them to take an active role in managing their oral health.
Conclusion
Autoimmune diseases present unique challenges in the field of dentistry, affecting the oral health and treatment of affected individuals. Dental professionals must possess a comprehensive understanding of autoimmune conditions and their manifestations to provide effective care. By tailoring treatment plans, collaborating with other healthcare providers, and prioritizing patient education, dental teams can optimize oral health outcomes for individuals with autoimmune diseases.