Menstruation, a natural biological process marking the reproductive cycle in females, is accompanied by complex hormonal fluctuations. The menstrual cycle, typically lasting between 21 and 35 days, involves a series of hormonal changes that regulate the monthly preparation of the body for pregnancy. These changes, especially the fluctuations in estrogen and progesterone, have profound effects not only on the reproductive system but also on other areas of the body, including oral and dental health.
In recent years, growing research has highlighted the connection between menstruation and oral health, particularly gum and dental treatments. The interaction between hormonal changes during different phases of the menstrual cycle and oral health can result in noticeable changes in the gums, teeth, and overall dental well-being. Understanding these connections can help both patients and dental professionals provide better care and prevent potential oral health problems. This article aims to provide a comprehensive review of how menstruation and the menstrual cycle affect oral health and the implications for dental treatments.
Table of Contents
ToggleMenstrual Cycle: An Overview
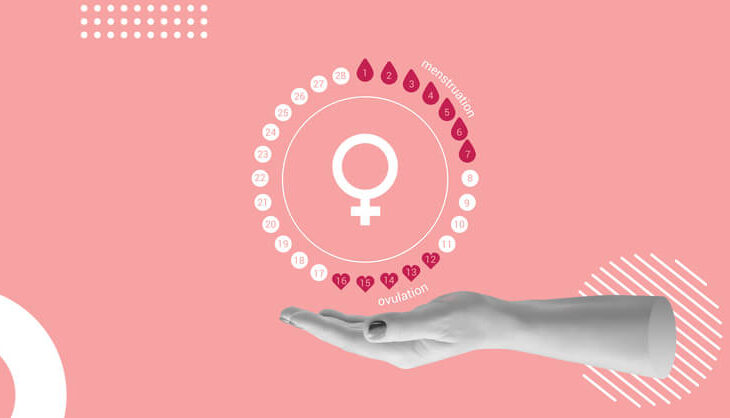
To understand how menstruation affects oral health, it’s essential first to understand the menstrual cycle. The menstrual cycle is typically divided into four main phases:
- Menstrual Phase (Day 1 to 5): This is the first stage of the cycle when menstruation occurs. The body sheds the uterine lining, and hormone levels, particularly estrogen and progesterone, are at their lowest.
- Follicular Phase (Day 6 to 14): This phase begins immediately after menstruation and is marked by an increase in estrogen levels as the body prepares for ovulation. The rise in estrogen helps thicken the uterine lining, preparing the body for potential pregnancy.
- Ovulation (Day 14): Midway through the cycle, a mature egg is released from the ovary. Estrogen levels peak, and progesterone levels begin to rise.
- Luteal Phase (Day 15 to 28): After ovulation, progesterone levels continue to rise to maintain the uterine lining. If fertilization does not occur, both estrogen and progesterone levels drop, leading to the start of menstruation and the beginning of a new cycle.
These hormonal changes during each phase of the menstrual cycle influence various systems in the body, including the cardiovascular, skeletal, and oral systems. For many women, fluctuations in hormone levels can lead to changes in mood, skin, and oral health.
Impact of Hormonal Changes on Oral Health
The gums, teeth, and other soft tissues in the mouth are highly sensitive to changes in hormone levels. The fluctuations in estrogen and progesterone during the menstrual cycle can cause several oral health issues, most notably:
- Gingival Inflammation (Menstrual Gingivitis)
- Changes in Saliva Composition
- Increased Sensitivity to Dental Treatments
- Oral Ulcers and Sores
- Temporomandibular Joint (TMJ) Pain
Gingival Inflammation (Menstrual Gingivitis)
One of the most common oral health concerns associated with menstruation is menstrual gingivitis. This condition involves inflammation of the gums, which may occur just before menstruation and resolve once menstruation begins. Symptoms include swollen, red, or bleeding gums, particularly around the molars. The increased blood flow to the gums during the luteal phase (due to rising progesterone levels) is believed to make the gums more sensitive to plaque and bacteria, leading to increased inflammation.
Changes in Saliva Composition
Hormonal changes during the menstrual cycle also affect the composition and flow of saliva. Saliva plays a crucial role in maintaining oral health by neutralizing acids, washing away food particles, and providing protective enzymes. During certain phases of the menstrual cycle, particularly around ovulation, changes in saliva composition may increase the risk of tooth decay and gum disease.
Increased Sensitivity to Dental Treatments
Some women report increased sensitivity to dental treatments, such as cleanings or fillings, during certain phases of their menstrual cycle. The increased inflammation in the gums and soft tissues during the luteal phase can make dental procedures more uncomfortable.
Oral Ulcers and Sores
Some women may experience an increase in oral ulcers or sores during menstruation. These can occur as a result of the hormonal fluctuations or due to immune changes that make the body more susceptible to infections or irritation.
Temporomandibular Joint (TMJ) Pain
For some women, hormonal changes during the menstrual cycle can exacerbate conditions such as temporomandibular joint disorder (TMD). TMD is a condition that affects the jaw joint and surrounding muscles, causing pain and discomfort. Estrogen receptors in the temporomandibular joint may make this area more sensitive to hormonal fluctuations, leading to increased jaw pain or discomfort around menstruation.
Hormonal Influences on Gum Health
The gums, or gingiva, are particularly sensitive to hormonal changes, and these changes can have a significant impact on gum health. There are several key ways in which hormonal fluctuations during the menstrual cycle influence the gums:
- Estrogen and Gum Health
- Progesterone and Inflammation
- Menstrual Gingivitis
- Periodontal Disease and Hormonal Changes
Estrogen and Gum Health
Estrogen plays a vital role in maintaining the structural integrity of gum tissues. It helps regulate collagen production, which is essential for the strength and resilience of the gums. However, during menstruation, the decrease in estrogen levels can lead to a breakdown in gum tissue, making them more susceptible to irritation and inflammation.
Progesterone and Inflammation
Progesterone is known to increase the permeability of blood vessels in the gums, leading to increased blood flow and a heightened inflammatory response. This is why many women experience increased gum sensitivity and inflammation during the luteal phase of the menstrual cycle, when progesterone levels are at their highest.
Menstrual Gingivitis
Menstrual gingivitis is characterized by an exaggerated inflammatory response in the gums just before menstruation. The gums may appear red, swollen, and prone to bleeding, particularly in response to plaque accumulation. This condition usually resolves once menstruation begins and hormone levels stabilize. Maintaining good oral hygiene during this time is crucial to prevent further irritation and inflammation.
Periodontal Disease and Hormonal Changes
Chronic hormonal imbalances can contribute to more severe gum disease, such as periodontitis. Women with hormonal imbalances, such as those caused by polycystic ovary syndrome (PCOS), are at a higher risk of developing periodontal disease. In these cases, the gums may become infected, leading to the destruction of the supporting bone structure around the teeth if left untreated.
Oral Health and Menstrual Disorders
Certain menstrual disorders, such as polycystic ovary syndrome (PCOS) and premenstrual syndrome (PMS), can exacerbate oral health issues. For example:
- Polycystic Ovary Syndrome (PCOS)
- Premenstrual Syndrome (PMS)
Polycystic Ovary Syndrome (PCOS)
PCOS is a common hormonal disorder that affects many women of reproductive age. It is characterized by elevated levels of androgens (male hormones), which can disrupt the balance of estrogen and progesterone. Women with PCOS are more prone to developing periodontal disease due to the chronic inflammation caused by hormonal imbalances. Additionally, insulin resistance, commonly associated with PCOS, can increase the risk of gum disease and tooth decay.
Premenstrual Syndrome (PMS)
PMS is a condition that affects many women in the days leading up to menstruation. It is characterized by a range of physical and emotional symptoms, including bloating, mood swings, and fatigue. The hormonal changes associated with PMS can also affect oral health, leading to increased gum sensitivity, dry mouth, and a higher risk of developing gingivitis or periodontal disease.
Implications for Dental Treatments
Given the impact of hormonal changes on oral health, it’s important for both patients and dental professionals to be aware of how the menstrual cycle may affect dental treatments. Here are some considerations for managing oral health and planning dental treatments during menstruation:
- Timing of Dental Appointments
- Managing Gingivitis and Gum Sensitivity
- Addressing Dry Mouth
- Pain Management During Dental Procedures
- Hormonal Contraceptives and Oral Health
Timing of Dental Appointments
For women who experience significant oral health changes during their menstrual cycle, timing dental appointments carefully can help improve comfort and outcomes. Scheduling treatments during the follicular phase, when estrogen levels are rising and progesterone levels are lower, may reduce gum sensitivity and inflammation.
Managing Gingivitis and Gum Sensitivity
Women who experience menstrual gingivitis should be diligent about maintaining good oral hygiene throughout their menstrual cycle. This includes brushing and flossing regularly, using an antibacterial mouthwash, and visiting the dentist for regular cleanings. In some cases, a dental professional may recommend scaling and root planing to remove plaque and tartar buildup below the gumline.
Addressing Dry Mouth
Hormonal changes during menstruation can sometimes lead to dry mouth, which increases the risk of tooth decay and gum disease. Drinking plenty of water, using sugar-free gum or lozenges to stimulate saliva production, and using an alcohol-free mouthwash can help alleviate dry mouth symptoms.
Pain Management During Dental Procedures
Women who experience increased sensitivity during menstruation may require additional pain management during dental treatments. This may include the use of topical anesthetics, local anesthesia, or anti-inflammatory medications to reduce discomfort during cleanings, fillings, or other dental procedures.
Hormonal Contraceptives and Oral Health
Hormonal contraceptives, such as birth control pills, can also affect oral health by altering the balance of estrogen and progesterone in the body. Women taking hormonal contraceptives may be at a higher risk of developing gum inflammation and should take extra care to maintain good oral hygiene. Dental professionals should be aware of a patient’s contraceptive use when planning treatments, as it may affect the healing process after procedures such as tooth extractions or periodontal surgery.
Frequently Asked Questions (FAQ)
What Are The Oral Changes During Menstruation?
Hormonal changes during menstruation can cause several oral health issues, including:
- Menstrual Gingivitis: Swollen, red, and bleeding gums due to increased blood flow and inflammation.
- Increased Gum Sensitivity: Heightened reaction to plaque, making gums more prone to irritation.
- Dry Mouth (Xerostomia): Reduced saliva production, increasing the risk of cavities and bad breath.
- Oral Ulcers and Sores: Some women experience more frequent mouth ulcers during menstruation.
- Metallic or Bitter Taste: Hormonal fluctuations can alter taste perception.
- Bad Breath: Changes in saliva composition and bacterial activity can lead to bad breath.
How Do You Treat Menstrual Gingivitis?
To manage menstrual gingivitis:
- Maintain Good Oral Hygiene – Brush twice daily with fluoride toothpaste and floss regularly.
- Use an Antibacterial Mouthwash – Helps reduce bacterial buildup in the gums.
- Stay Hydrated – Drinking water helps with saliva production and reduces dryness.
- Eat a Balanced Diet – Avoid sugary foods that can worsen inflammation.
- Visit a Dentist Regularly – Professional cleanings help control plaque buildup and inflammation.
- Use a Soft-Bristled Toothbrush – This prevents additional irritation to sensitive gums.
What Happens if I Get Period Blood in My Mouth?
If period blood enters the mouth, it is not harmful in most cases, as menstrual blood is similar to regular blood. However, proper oral hygiene should be maintained to prevent any bacterial infections. Rinse your mouth with water or mouthwash if necessary.
What Is the Effect of the Menstrual Cycle on Periodontal Health?
Clinical and microbiological studies have shown that hormonal fluctuations during the menstrual cycle influence periodontal health by:
- Increasing gum inflammation (gingivitis) during the luteal phase.
- Altering the oral microbiome, leading to an increased risk of periodontal disease.
- Reducing the effectiveness of the immune response, making gums more susceptible to bacterial infections.
Regular dental checkups and good oral hygiene practices can help mitigate these effects.
Can Your Period Affect Your Teeth?
Yes, hormonal changes during menstruation can:
- Increase tooth sensitivity due to gum inflammation.
- Lead to dry mouth, increasing the risk of cavities.
- Cause a metallic taste or temporary changes in taste perception.
- Worsen symptoms of pre-existing gum disease.
Women should maintain good oral hygiene and stay hydrated to counteract these effects.
Why Does My Mouth Feel Weird on My Period?
During menstruation, hormonal changes can lead to:
- Dry Mouth – Reduced saliva production may make the mouth feel dry or sticky.
- Taste Changes – A metallic or bitter taste can develop due to hormone fluctuations.
- Gum Sensitivity – Swelling or tenderness in the gums can cause discomfort.
These changes are temporary and typically resolve after menstruation ends.
Why Do I Have Bad Breath on My Period?
Bad breath during menstruation can be caused by:
- Hormonal Changes – Alterations in saliva production can lead to increased bacterial activity.
- Dry Mouth – Reduced saliva flow makes it easier for odor-causing bacteria to thrive.
- Increased Plaque and Tartar – Gums may become more sensitive to bacterial buildup.
To prevent bad breath, maintain good oral hygiene, drink plenty of water, and use an antibacterial mouthwash.
Can Low Estrogen Affect Your Teeth?
Yes, low estrogen levels can negatively impact oral health by:
- Reducing Bone Density – Increasing the risk of tooth loss and osteoporosis-related issues.
- Decreasing Saliva Production – Leading to dry mouth, which promotes tooth decay.
- Weakening Gum Tissue – Making gums more susceptible to infections and periodontal disease.
Women with hormonal imbalances should monitor their oral health closely and consult their dentist for preventive care.
What Is Period Dental Disease?
“Period dental disease” is a term sometimes used to describe gum inflammation and other oral health issues related to hormonal changes during menstruation. It includes conditions like:
- Menstrual Gingivitis – Temporary gum inflammation before and during menstruation.
- Hormonal Periodontitis – Chronic gum disease worsened by hormonal fluctuations.
- Increased Risk of Cavities – Due to dry mouth and changes in saliva composition.
Regular dental visits, good oral hygiene, and proper hydration can help manage these symptoms.
Conclusion
Menstruation and the menstrual cycle have a significant impact on oral and dental health, largely due to the fluctuations in estrogen and progesterone levels. These hormonal changes can lead to a variety of oral health issues, including gingivitis, dry mouth, increased sensitivity to dental treatments, and a higher risk of gum disease. Women with menstrual disorders, such as PCOS and PMS, may be at an even higher risk of developing oral health problems.
For dental professionals, understanding the connection between the menstrual cycle and oral health is crucial for providing personalized care to female patients. By taking into account the timing of the menstrual cycle, dental professionals can better manage gum sensitivity and inflammation, improve the comfort of dental procedures, and reduce the risk of complications. Additionally, women should be proactive about maintaining good oral hygiene throughout their menstrual cycle to prevent gum disease and other oral health issues.
Incorporating an understanding of hormonal influences on oral health into dental care practices can lead to better outcomes for women and help prevent long-term oral health problems associated with hormonal changes.