Dental implant surgery has become one of the most reliable methods to replace missing teeth, offering both aesthetic and functional benefits. However, one of the key prerequisites for successful dental implant placement is the presence of adequate bone volume in the jaw to support the implant. In cases where there is insufficient bone, bone grafting becomes an essential preparatory procedure. This article explores the various bone grafting techniques used in dental implant surgery and other oral surgeries, detailing their processes, advantages, and potential limitations.
Table of Contents
ToggleImportance of Bone Grafting in Dentistry
Bone grafting is a surgical procedure that aims to rebuild or replace lost bone in areas where it is deficient. Bone loss can occur due to several factors, including periodontal disease, trauma, infection, or prolonged tooth loss, which leads to bone resorption. Adequate bone volume is essential not only for implant stability but also for achieving proper aesthetics and long-term implant success.
Without sufficient bone, dental implants may fail due to lack of support, leading to poor functional outcomes and unsatisfactory aesthetics. Bone grafting provides a solution to these issues, allowing clinicians to rebuild lost bone and create a stable foundation for implants.
Types of Bone Grafting Techniques
Bone grafting techniques vary depending on the extent of bone loss, the location of the defect, and the type of surgery planned. Below are the most commonly used techniques:
- Socket Preservation (Alveolar Ridge Preservation)
- Onlay Grafting
- Sinus Lift (Sinus Augmentation)
- Ridge Expansion (Ridge Splitting)
- Guided Bone Regeneration (GBR)
- Autogenous Block Grafting
- All-on-4 and Zygomatic Implants with Minimal Grafting
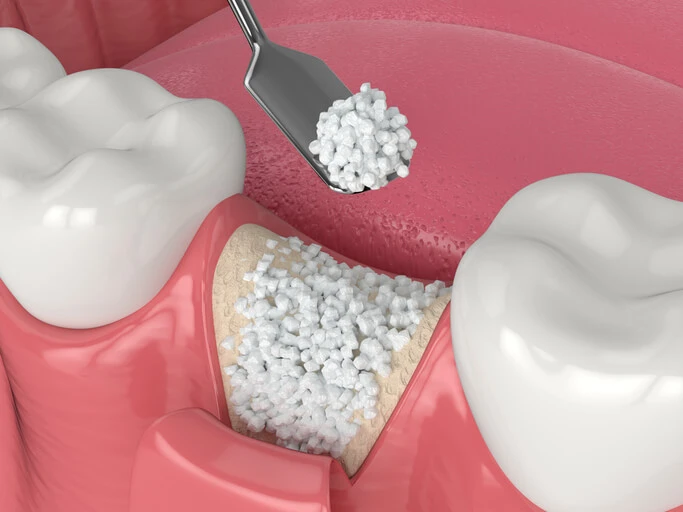
Socket Preservation (Alveolar Ridge Preservation)
Socket preservation is performed immediately after a tooth extraction to prevent bone loss in the extraction site. Once the tooth is removed, a bone graft material is placed into the empty socket to maintain the bone height and width. The graft material acts as a scaffold, promoting new bone growth and preventing the alveolar ridge from collapsing.
Materials Used:
- Autografts (bone harvested from the patient, typically from the chin or ramus)
- Allografts (bone sourced from a human donor)
- Xenografts (bone from an animal source, often bovine)
- Synthetic bone substitutes (e.g., bioactive ceramics, hydroxyapatite)
Pros:
- Prevents significant bone resorption after tooth extraction.
- Reduces the need for more extensive grafting procedures in the future.
- Supports soft tissue healing and maintains the alveolar ridge contour.
- Enhances aesthetic outcomes, especially in the anterior region.
Cons:
- Limited to localized bone loss around the extraction site.
- Healing time can vary based on the material used, typically taking 3-6 months.
- May increase treatment cost.
Onlay Grafting
Onlay grafting is used to rebuild large horizontal or vertical bone deficiencies. Bone graft material, often in the form of a block, is placed on top of the deficient area and secured with screws to increase bone height or width. This technique is common in cases where there has been severe bone loss due to long-term tooth absence or trauma.
Materials Used:
- Autografts, particularly from intraoral sites such as the mandibular ramus or chin.
- Allografts or xenografts for patients who prefer not to undergo bone harvesting.
Procedure:
- The recipient site is prepared by decorticating the bone to enhance vascularization and integration.
- The graft material is shaped and secured with fixation screws.
- A barrier membrane may be used to protect the graft and promote bone regeneration.
- The site is closed, and the healing process begins, typically requiring 4-9 months.
Pros:
- Effective for significant bone augmentation, addressing both height and width deficiencies.
- Can provide sufficient bone volume for implant placement, even in severe cases.
- High success rate when combined with proper surgical techniques and postoperative care.
Cons:
- Requires a longer healing period compared to other techniques.
- Potential for partial graft resorption.
- More invasive, especially when harvesting autografts, increasing patient morbidity.
- Risk of complications, such as infection, donor site pain, or graft failure.
Sinus Lift (Sinus Augmentation)
A sinus lift is a procedure designed to increase bone height in the posterior maxilla, where the maxillary sinus floor often limits implant placement. This technique is particularly valuable for patients with severe bone loss in the upper jaw. By lifting the sinus membrane and placing bone graft material in the sinus cavity, clinicians can create the necessary volume for implants.
Techniques:
- Lateral Window Approach: A small bony window is created on the lateral sinus wall to access and lift the membrane. Bone graft material is then placed into the sinus cavity.
- Transalveolar Approach: Less invasive, this method involves accessing the sinus through the implant site and lifting the membrane with specialized instruments.
Materials Used:
Autografts, allografts, xenografts, or synthetic substitutes.
Pros:
- Specifically addresses bone deficiencies in the posterior maxilla.
- Enables implant placement in areas previously deemed unsuitable.
- High success rates when performed by experienced clinicians.
Cons:
- Risk of sinus membrane perforation, which may lead to graft failure.
- Postoperative complications, such as sinus infections, swelling, or discomfort.
- Longer healing time, ranging from 4-9 months before implants can be placed.
- Requires specialized surgical expertise and meticulous technique.
Ridge Expansion (Ridge Splitting)
Ridge expansion is a technique used to widen a narrow alveolar ridge to accommodate implants. This method is ideal for patients with adequate bone height but insufficient ridge width. The alveolar ridge is carefully split longitudinally, and graft material is often placed between the separated segments to enhance bone regeneration.
Procedure:
- The ridge is carefully scored and split using chisels or piezoelectric surgical tools.
- Bone graft material may be placed within the split to promote new bone formation.
- In some cases, implants can be placed simultaneously.
Pros:
- Minimally invasive compared to block grafting.
- Allows for simultaneous implant placement in suitable cases.
- Reduces the need for secondary surgeries, saving time and cost.
Cons:
- Not suitable for extremely thin ridges or severe bone deficiencies.
- Risk of ridge fracture during the splitting process.
- May require additional healing time if implants are not placed immediately.
Guided Bone Regeneration (GBR)
Guided Bone Regeneration (GBR) involves using a barrier membrane to protect the bone graft material and create a space for new bone growth. This technique is particularly effective for localized defects, such as small dehiscences or fenestrations around implants.
Materials Used:
- Bone graft material (autograft, allograft, xenograft, or synthetic).
- Barrier membranes, which can be resorbable (e.g., collagen) or non-resorbable (e.g., titanium-reinforced PTFE).
Procedure:
- The defect area is debrided and prepared for the graft.
- Bone graft material is placed into the defect.
- A barrier membrane is positioned over the graft to prevent soft tissue invasion.
- The site is sutured, and healing begins.
Pros:
- Highly predictable results when performed correctly.
- Promotes both bone and soft tissue regeneration.
- Can address a wide range of localized bone defects.
Cons:
- Requires precise surgical technique to avoid membrane exposure.
- Healing period is longer, often 6-9 months.
- Non-resorbable membranes may require a second surgery for removal.
Autogenous Block Grafting
This technique involves harvesting a block of bone from the patient’s own body (typically the chin, ramus, or iliac crest) and securing it to the recipient site with screws. Autogenous block grafting is often used for severe bone deficiencies requiring significant augmentation.
Pros:
- Autogenous grafts are considered the gold standard due to their osteogenic, osteoinductive, and osteoconductive properties.
- High success rates when properly executed.
- Ideal for addressing large bone defects where other techniques may fall short.
Cons:
- Requires a secondary surgical site, increasing patient morbidity and recovery time.
- More invasive compared to other grafting methods.
- Risk of donor site complications, such as pain, nerve injury, or infection.
All-on-4 and Zygomatic Implants with Minimal Grafting
In cases of severe bone loss, advanced techniques such as All-on-4 implants (four implants supporting a full-arch prosthesis) or zygomatic implants (anchored into the cheekbone) can minimize or eliminate the need for bone grafting.
Pros:
- Reduces treatment time compared to traditional grafting and implant placement.
- Allows immediate loading of prosthetics in many cases, restoring function and aesthetics quickly.
- Suitable for patients with severe maxillary bone resorption.
Cons:
- Requires highly skilled surgeons and advanced planning.
- Limited applicability to certain cases where alternative solutions may be more appropriate.
- More complex and expensive than traditional methods.
Key Considerations in Bone Grafting
Material Selection
The choice of bone graft material significantly influences the outcome. The four primary types of bone graft materials are:
- Autografts: The patient’s own bone offers the best results due to its osteogenic, osteoinductive, and osteoconductive properties.
- Allografts: Donor bone is osteoconductive and avoids the need for a secondary surgical site, though it lacks osteogenic properties.
- Xenografts: Animal-derived bone (commonly bovine) is biocompatible, osteoconductive, and widely available.
- Synthetic: Materials such as calcium phosphate and bioactive ceramics are cost-effective and reduce the risk of disease transmission but lack osteogenic capabilities.
Healing Time
Bone grafts require sufficient time to integrate with the native bone. Healing times vary based on the technique, material used, and patient specific factors but generally range from 3 to 9 months. Factors such as smoking, systemic health, and oral hygiene can impact healing.
Complications
While bone grafting is highly successful, potential complications include:
- Infection or inflammation of the surgical site.
- Partial or total graft resorption.
- Donor site morbidity (in autografts), such as prolonged pain or nerve damage.
- Delayed healing in smokers or patients with systemic conditions like diabetes.
- Graft exposure due to inadequate soft tissue closure.
Frequently Asked Questions (FAQs)
1. How long does bone grafting take to heal?
The healing time for bone grafts varies depending on the technique used and the patient’s overall health. Generally, it takes between 3 to 9 months for complete bone integration.
2. Is bone grafting painful?
Bone grafting is performed under local anesthesia or sedation, so patients do not feel pain during the procedure. Some discomfort and swelling are expected during recovery, but this can be managed with prescribed pain medications.
3. What is the success rate of bone grafting?
The success rate of bone grafting is high, typically ranging between 85% and 95%, depending on factors such as the technique used, patient health, and postoperative care.
4. Can I get a dental implant immediately after bone grafting?
In some cases, implants can be placed immediately after bone grafting, but most patients require a healing period of several months before the implant is placed.
5. Are there any risks or complications associated with bone grafting?
While bone grafting is a safe procedure, potential risks include infection, graft failure, swelling, and minor discomfort. In rare cases, additional surgeries may be required if the graft does not integrate properly.
6. What type of bone graft material is best?
The best bone graft material depends on the individual case. Autografts are considered the gold standard, but allografts, xenografts, and synthetic materials are also effective and commonly used.
7. Can smokers undergo bone grafting?
Smoking can negatively affect bone healing and increase the risk of graft failure. Patients are strongly advised to quit smoking before undergoing bone grafting and implant placement.
8. How do I know if I need a bone graft before dental implants?
Your dentist or oral surgeon will evaluate your bone density using imaging techniques such as X-rays or CBCT scans. If there is insufficient bone to support an implant, a bone graft will likely be recommended.
9. What should I avoid after bone grafting surgery?
Patients should avoid smoking, strenuous activities, hard or crunchy foods, and touching the surgical site. Following post-operative care instructions, such as taking prescribed medications and maintaining oral hygiene, is essential for proper healing.
10. How much does bone grafting cost?
The cost of bone grafting varies based on the complexity of the procedure, the type of graft material used, and geographic location. Generally, prices range from a few hundred to several thousand dollars.
Conclusion
Bone grafting is an integral part of modern dental implantology and oral surgery, providing solutions for patients with insufficient bone volume. Techniques such as socket preservation, onlay grafting, sinus lifts, and guided bone regeneration enable clinicians to address diverse clinical scenarios. While each technique has its own set of advantages and limitations, advancements in materials and surgical methods continue to improve outcomes. The choice of technique should be tailored to the individual patient’s needs, ensuring optimal results and long-term success of the dental implant or oral surgery.