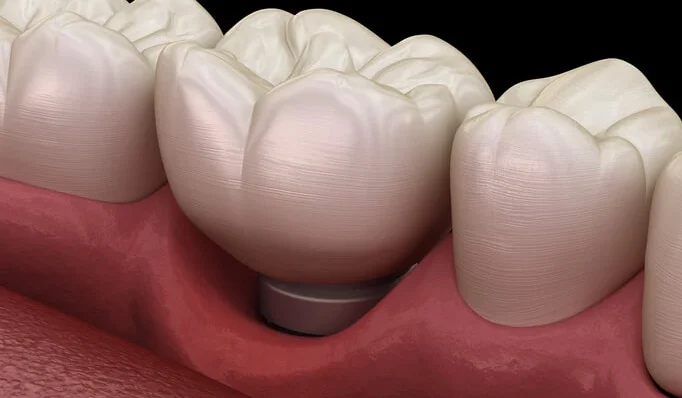
Dental implants have revolutionized the field of dentistry by providing a durable and aesthetically pleasing solution for replacing missing teeth. However, the success of dental implants relies not only on osseointegration, the process by which the implant fuses with the jawbone, but also on the health and stability of the soft tissues surrounding the implant. Soft tissue management plays a crucial role in ensuring the long-term success of dental implants, as it helps to prevent complications such as peri-implant mucositis, peri-implantitis, and soft tissue recession. In this article, we will explore the importance of soft tissue management around dental implants and discuss key strategies for achieving optimal outcomes.
Table of Contents
ToggleImportance of Soft Tissue Management
Soft tissue management is essential for maintaining the health and stability of the peri-implant tissues, including the gingiva and the mucosa. Healthy soft tissues provide a protective barrier around the implant, helping to prevent bacterial infiltration and inflammation. Proper soft tissue management also contributes to the maintenance of peri-implant esthetics, ensuring that the gums appear natural and symmetrical around the implant restoration.
One of the primary goals of soft tissue management is to establish a stable and functional peri-implant soft tissue seal. This seal helps to prevent the migration of bacteria and debris into the peri-implant sulcus, reducing the risk of inflammation and infection. Additionally, a well-maintained soft tissue seal contributes to the stability of the implant restoration and helps to preserve the underlying bone structure.
Key Strategies for Soft Tissue Management
- Preoperative Evaluation and Treatment Planning
- Implant Placement Technique
- Soft Tissue Augmentation
- Prosthetic Design and Material Selection
- Maintenance and Follow-Up
- Management of Peri-Implant Complications
Preoperative Evaluation and Treatment Planning
A thorough preoperative evaluation is essential for assessing the condition of the soft tissues and identifying any potential risk factors for complications. This may include evaluating the quality and quantity of the peri-implant mucosa, assessing the presence of any underlying soft tissue deficiencies or abnormalities, and identifying any systemic factors that may impact soft tissue healing. Based on this evaluation, a comprehensive treatment plan can be developed to address any soft tissue deficiencies and optimize the peri-implant environment.
Implant Placement Technique
The surgical technique used for implant placement can have a significant impact on the health and stability of the peri-implant soft tissues. Careful attention should be paid to achieving proper implant positioning and orientation to ensure optimal soft tissue contours and emergence profile. Minimally invasive surgical techniques, such as flapless or guided surgery, may help to preserve the soft tissue architecture and promote faster healing.
Soft Tissue Augmentation
In cases where the peri-implant soft tissues are deficient or inadequate, soft tissue augmentation procedures may be necessary to enhance the soft tissue contours and improve esthetic outcomes. Soft tissue grafting techniques, such as connective tissue grafts or free gingival grafts, can be used to increase the volume and thickness of the peri-implant mucosa and create a more natural-looking soft tissue profile.
Prosthetic Design and Material Selection
The design and materials used for the implant restoration can also influence the health and stability of the peri-implant soft tissues. Prosthetic components should be carefully selected to minimize tissue irritation and promote soft tissue adaptation. Additionally, the use of biocompatible materials that mimic the natural properties of the peri-implant tissues can help to minimize inflammation and promote soft tissue integration.
Maintenance and Follow-Up
Regular maintenance and follow-up care are essential for monitoring the health of the peri-implant soft tissues and preventing complications. Patients should be instructed on proper oral hygiene practices, including effective plaque control around the implant restoration. Regular professional cleanings and examinations allow for early detection and treatment of any signs of peri-implant inflammation or infection.
Management of Peri-Implant Complications
Despite meticulous soft tissue management, complications such as peri-implant mucositis and peri-implantitis may still occur. Prompt diagnosis and management of these complications are critical for preventing further soft tissue and bone loss. Treatment may involve nonsurgical interventions such as antimicrobial therapy and mechanical debridement, or surgical interventions such as flap surgery and bone grafting.
Conclusion
Soft tissue management plays a crucial role in the long-term success of dental implants by promoting the health and stability of the peri-implant tissues. By employing a combination of preoperative evaluation, surgical techniques, soft tissue augmentation, prosthetic design, and maintenance protocols, dental professionals can optimize the peri-implant environment and minimize the risk of complications. By prioritizing soft tissue management, clinicians can ensure that their patients achieve durable and esthetically pleasing outcomes following implant treatment.