The oral cavity is a dynamic and diverse environment that houses a vast array of bacteria. These bacteria colonize various surfaces within the mouth, including the teeth, gums, tongue, and oral mucosa. While some bacteria are beneficial and contribute to oral health, others can be pathogenic and lead to oral infections and diseases. The balance between beneficial and pathogenic bacteria is crucial for maintaining oral health. Beneficial bacteria help in digestion, produce antimicrobial substances, and contribute to the overall microbial ecosystem. On the other hand, pathogenic bacteria can cause tooth decay, gum disease, and other oral infections. Understanding the complex interactions between bacteria in the mouth is essential for promoting oral health and preventing oral diseases. Regular oral hygiene practices and professional dental care play vital roles in maintaining a healthy balance of bacteria in the oral cavity.
Beneficial Bacteria in the Mouth
Beneficial bacteria refer to certain types of bacteria that contribute to oral health and play a positive role in maintaining the balance of the oral microbiome. Here’s an explanation of beneficial bacteria in the mouth:
- Streptococcus salivarius
- Streptococcus sanguinis
- Streptococcus mitis
- Lactobacillus species
- Actinomyces species
- Veillonella species
Streptococcus salivarius
Streptococcus salivarius is a beneficial bacteria commonly found in the mouth. It is a part of the normal oral microbiota and contributes to oral health by inhibiting the growth of harmful bacteria. S. salivarius produces bacteriocins, antimicrobial substances that can help control the population of pathogenic bacteria in the oral cavity.
Streptococcus sanguinis
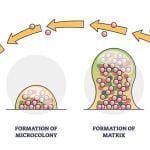
Streptococcus sanguinis is another beneficial bacteria found in the mouth. It plays a crucial role in maintaining oral health by forming biofilms on the tooth surface and preventing the colonization of harmful bacteria. S. sanguinis also produces hydrogen peroxide, which has antimicrobial properties and can help control the growth of pathogens.
Streptococcus mitis
Streptococcus mitis is a commensal bacteria found in the oral cavity that contributes to oral health. It competes with harmful bacteria for nutrients and adhesion sites, limiting their colonization and reducing the risk of dental caries and periodontal diseases.
Lactobacillus species
Lactobacillus species are beneficial bacteria that can be found in the mouth. They are lactic acid-producing bacteria that help maintain the pH balance in the oral cavity. By producing lactic acid, they create an acidic environment that inhibits the growth of acid-loving bacteria, such as Streptococcus mutans, which is associated with tooth decay.
Actinomyces species
Actinomyces species are beneficial bacteria that contribute to oral health. They play a role in the formation of dental plaque and biofilms, which help protect the teeth and gums from harmful bacteria. Actinomyces species also assist in breaking down complex carbohydrates and producing beneficial byproducts.
Veillonella species
Veillonella species are commensal bacteria found in the mouth that have been associated with oral health. They metabolize lactic acid produced by other bacteria, helping to maintain a balanced pH in the oral cavity. Veillonella species are also involved in the breakdown of certain compounds, such as lactate, and contribute to the overall microbial ecosystem in the mouth.
Harmful bacteria in mouth
In the oral cavity, pathogenic or harmful bacteria refer to certain types of bacteria that can cause oral infections and contribute to the development of oral diseases. Here’s an explanation of some common harmful or pathogenic bacteria in the mouth:
- Streptococcus mutans
- Porphyromonas gingivalis
- Aggregatibacter actinomycetemcomitan
- Tannerella forsythia
- Treponema denticola
- Prevotella intermedia
- Fusobacterium nucleatum
Streptococcus mutans
Streptococcus mutans is one of the most well-known pathogenic bacteria in the oral cavity. It is associated with dental caries, commonly known as tooth decay. S. mutans thrives in the presence of sugars and produces acids that can erode tooth enamel, leading to the formation of cavities.
Porphyromonas gingivalis
Porphyromonas gingivalis is a key pathogenic bacterium involved in the development of periodontal diseases, including gingivitis and periodontitis. It forms biofilms along the gum line and releases toxins that cause inflammation and destruction of the gum tissues and supporting structures of the teeth.
Aggregatibacter actinomycetemcomitan
Aggregatibacter actinomycetemcomitans is another pathogenic bacterium associated with periodontal diseases. It can invade gum tissues, leading to the destruction of connective tissues and bone loss. A. actinomycetemcomitans is commonly found in individuals with aggressive forms of periodontitis.
Tannerella forsythia
Tannerella forsythia is a pathogenic bacterium implicated in periodontal diseases. It is known to produce enzymes that can break down proteins in gum tissues, contributing to tissue damage and inflammation.
Treponema denticola
Treponema denticola is a pathogenic bacterium found in the oral cavity, particularly in cases of periodontitis. It is capable of penetrating gum tissues and produces toxins that contribute to tissue destruction and inflammation.
Prevotella intermedia
Prevotella intermedia is a pathogenic bacterium associated with periodontal diseases. It thrives in the presence of an anaerobic environment and contributes to the production of inflammatory substances that can damage gum tissues and promote disease progression.
Fusobacterium nucleatum
Fusobacterium nucleatum is a pathogenic bacterium commonly found in the oral cavity. It can adhere to oral surfaces and facilitate the attachment of other pathogenic bacteria, promoting the formation of complex biofilms and increasing the risk of periodontal diseases.
Conclusion
Oral microbiome is complex, consisting of numerous bacterial species, and the interactions between these bacteria and the host are still being researched. While these bacteria are generally considered beneficial, the overall balance and diversity of the oral microbiome are critical for oral health.
It’s important to note that the presence of these pathogenic bacteria alone is not sufficient to cause oral diseases. Various factors, including poor oral hygiene, a compromised immune system, genetic predisposition, and lifestyle factors, play a role in the development and progression of oral diseases. Maintaining good oral hygiene practices, such as regular brushing, flossing, and visiting the dentist, is crucial for preventing the overgrowth of pathogenic bacteria and maintaining oral health.