The periodontium is a crucial component of the oral cavity, playing a pivotal role in supporting and anchoring the teeth within the jawbone. Comprising various structures and tissues, the periodontium ensures the stability and functionality of the dentition. In this comprehensive article, we will delve into the intricate details of the periodontium, exploring its anatomy, functions, common issues, and preventive measures.
Anatomy of the Periodontium
The periodontium consists of four main components, each with a unique function in maintaining the health and integrity of the teeth.
Gingiva (Gums)
- Free Gingiva
- Attached Gingiva
Free Gingiva
This is the part of the gingiva that is visible and surrounds the teeth. It forms a collar-like band and extends coronally, creating the gumline.
Attached Gingiva
This portion is firmly attached to the underlying bone and the necks of the teeth. The junction between the free and attached gingiva is known as the gingival sulcus.
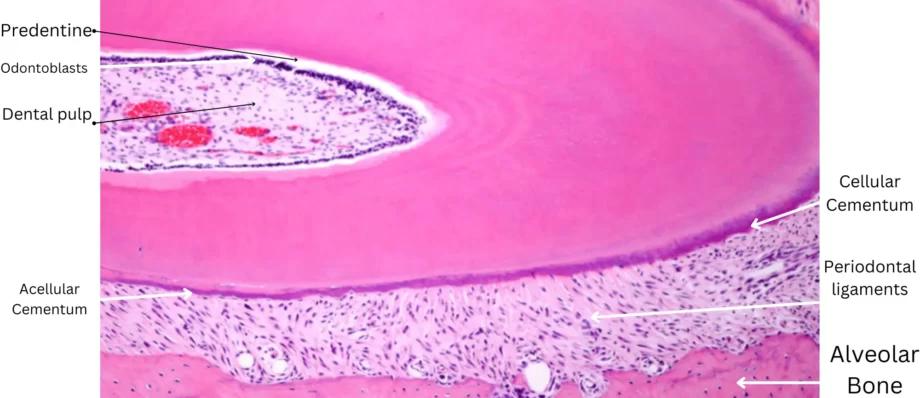
Cementum
Cementum is a calcified tissue covering the roots of the teeth. It is not as hard as enamel but provides essential functions in tooth anchorage.
- Acellular Cementum
- Cellular Cementum
Acellular Cementum
This covers the cervical and middle thirds of the root and does not contain living cells.
Cellular Cementum
Found in the apical third of the root, this type of cementum contains living cells known as cementocytes.
Alveolar Bone
The alveolar bone consists of the facial and lingual plates, which form the sockets (alveoli) that hold the roots of the teeth.
- Alveolar Crest
- Alveolar Socket
- Trabecular Bone
Alveolar Crest
The ridge of bone at the highest point of the alveolar process.
Alveolar Socket
The bony socket that houses the tooth root.
Trabecular Bone
The spongy bone found between the cortical plates, providing structural support.
Periodontal Ligament (PDL)
The periodontal ligament is a fibrous connective tissue that surrounds the roots of the teeth and attaches them to the alveolar bone.
Sharpey’s Fibers
Collagen fibers that insert into the cementum and bone, anchoring the tooth securely.
Functions
The PDL functions in tooth support, shock absorption, and sensory perception. It contains blood vessels and nerve endings.
Blood Supply and Innervation
Blood vessels within the periodontal ligament supply nutrients to the cementum and the adjacent alveolar bone. Nerve fibers in the PDL provide sensory feedback, allowing for the perception of pressure, temperature, and pain. This sensory input is vital for regulating forces during biting and chewing.
Gingival Architecture
The gingiva consists of different layers, including the epithelium and the underlying connective tissue.
Epithelial Layers
The gingival epithelium includes the oral epithelium facing the oral cavity and the sulcular epithelium lining the gingival sulcus.
Connective Tissue
Comprising collagen fibers, blood vessels, and immune cells, the connective tissue provides support and nourishment to the overlying epithelium.
Functions of the Periodontium
- Support and Stability
- Shock Absorption
- Nutrient Supply
- Sensory Function
Support and Stability
The periodontium provides a stable foundation for the teeth, anchoring them securely within the jawbone. This stability is essential for proper oral function, including chewing, speaking, and maintaining facial aesthetics.
Shock Absorption
The periodontal ligament acts as a shock absorber, dissipating the forces generated during biting and chewing. This prevents excessive stress on the teeth and the supporting structures, reducing the risk of damage.
Nutrient Supply
Blood vessels within the periodontal ligament supply nutrients to the cementum and the surrounding bone, contributing to their health and maintenance.
Sensory Function
Nerve fibers in the periodontal ligament contribute to the sensory perception of the oral environment. This sensory input is crucial for regulating the forces applied during biting and chewing.
Common Periodontal Issues
- Gingivitis
- Periodontitis
- Gingival Recession
- Periodontal Abscess
Gingivitis
Gingivitis is the inflammation of the gingival tissue, often caused by the accumulation of dental plaque. Symptoms include redness, swelling, and bleeding of the gums, and it is generally reversible with proper oral hygiene practices.
Periodontitis
If left untreated, gingivitis can progress to periodontitis, a more severe form of gum disease. Periodontitis involves the inflammation of the supporting structures of the teeth, leading to the destruction of the periodontal ligament and alveolar bone. Common signs include gum recession, pocket formation, and tooth mobility.
Gingival Recession
Gingival recession occurs when the margin of the gums pulls away from the teeth, exposing the tooth roots. It can result from various factors, including aggressive tooth brushing, periodontal disease, and anatomical factors.
Periodontal Abscess
A periodontal abscess is a localized collection of pus within the periodontal tissues. It is often associated with advanced periodontitis and may cause pain, swelling, and discomfort.
Conclusion
Understanding the periodontium is essential for maintaining optimal oral health. From the gingiva to the periodontal ligament and alveolar bone, each component plays a vital role in supporting the teeth and ensuring their stability. Regular dental care, effective oral hygiene practices, and lifestyle modifications are key factors in preventing periodontal issues and preserving the integrity of the periodontium. As the gateway to a healthy smile, a comprehensive approach to periodontal care is essential for overall well-being.