Osteonecrosis of the jaw (ONJ) is a rare but potentially serious condition that affects the jawbone. Also known as jawbone necrosis or jaw osteonecrosis, it occurs when the bone tissue in the jaw fails to heal after minor trauma, leading to the death of bone cells. While ONJ most commonly occurs following dental procedures, it can also be associated with certain medications, particularly those used in cancer treatment. In this article, we will delve into the causes, symptoms, diagnosis, and treatment options for osteonecrosis of the jaw.
Table of Contents
ToggleUnderstanding Osteonecrosis
Osteonecrosis, in general, refers to the death of bone tissue due to a lack of blood supply. Without adequate blood flow, bone cells cannot receive the nutrients and oxygen they need to survive, leading to their death. In the jaw, this condition can be particularly problematic due to its role in supporting the teeth and facilitating various oral functions, including chewing and speaking.
Causes of Osteonecrosis of the Jaw
- Dental Procedures
- Medications
- Radiation Therapy
Dental Procedures
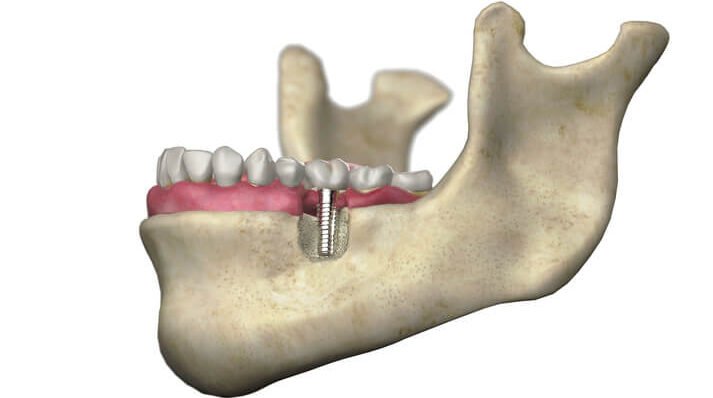
The most common cause of ONJ is dental procedures, particularly invasive ones like tooth extraction or dental implant placement. Trauma to the jawbone during these procedures can disrupt blood flow to the area, predisposing it to osteonecrosis.
Medications
Certain medications have been associated with an increased risk of developing ONJ. Bisphosphonates, which are commonly used to treat osteoporosis and prevent bone complications in cancer patients with bone metastases, are one such class of drugs. Other medications, such as denosumab (a monoclonal antibody), have also been implicated in rare cases of ONJ.
Radiation Therapy
Cancer patients who undergo radiation therapy to the head and neck region may develop osteonecrosis of the jaw as a complication. Radiation can damage blood vessels and impair bone healing, increasing the risk of ONJ, especially in conjunction with dental procedures.
Symptoms of Osteonecrosis of the Jaw
The symptoms of ONJ can vary depending on the severity of the condition. In the early stages, patients may experience no symptoms at all, making it challenging to detect. However, as the condition progresses, the following symptoms may occur:
- Pain or Discomfort
- Swelling or Infection
- Loose Teeth
- Exposed Bone
- Difficulty Healing
Pain or Discomfort
Persistent pain or discomfort in the jaw, gums, or teeth is a common symptom of ONJ. The pain may be dull and aching or sharp and intense, depending on the extent of bone damage.
Swelling or Infection
Swelling of the gums or soft tissues in the mouth can occur, often accompanied by signs of infection such as redness, warmth, or pus drainage.
Loose Teeth
As the bone deteriorates, teeth may become loose or start to shift out of position. This can affect bite alignment and overall oral function.
Exposed Bone
In advanced cases of ONJ, the affected area of the jawbone may become exposed through the gums. Exposed bone is vulnerable to infection and can be painful or sensitive to touch.
Difficulty Healing
Wounds or sores in the mouth may take longer than usual to heal, or they may not heal at all. This is because compromised blood flow impairs the body’s ability to repair damaged tissue.
Diagnosis of Osteonecrosis of the Jaw
Diagnosing ONJ typically involves a combination of clinical evaluation, medical history review, and imaging studies. Dentists, oral surgeons, or maxillofacial specialists are trained to recognize the signs and symptoms of ONJ and may order the following tests:
- X-rays
- CT Scan or MRI
- Biopsy
X-rays
X-ray images of the jaw can reveal changes in bone density or structure that may indicate osteonecrosis.
CT Scan or MRI
More detailed imaging studies like computed tomography (CT) scans or magnetic resonance imaging (MRI) can provide a clearer picture of the extent of bone damage and help guide treatment planning.
Biopsy
In some cases, a small sample of tissue may be taken from the affected area for examination under a microscope to confirm the diagnosis of ONJ and rule out other conditions.
Treatment Options for Osteonecrosis of the Jaw
The management of ONJ depends on several factors, including the underlying cause, the severity of symptoms, and the patient’s overall health. Treatment options may include:
- Medication Management
- Antibiotics
- Pain Management
- Surgical Intervention
- Hyperbaric Oxygen Therapy (HBOT)
Medication Management
In cases where ONJ is associated with bisphosphonate or denosumab therapy, discontinuing the medication or adjusting the dosage may help alleviate symptoms and slow the progression of bone necrosis. However, this decision should be made in consultation with the patient’s healthcare provider, as stopping these medications abruptly can have other implications for bone health.
Antibiotics
If infection is present, antibiotics may be prescribed to help control the spread of bacteria and prevent further complications.
Pain Management
Over-the-counter or prescription pain medications may be recommended to manage discomfort associated with ONJ.
Surgical Intervention
In advanced cases of ONJ where conservative measures have failed, surgical intervention may be necessary to remove necrotic bone tissue, promote healing, and reduce the risk of infection. Surgical procedures may range from debridement (removal of dead tissue) to more extensive jawbone resection or reconstruction.
Hyperbaric Oxygen Therapy (HBOT)
Some healthcare providers may recommend HBOT as an adjunctive therapy for ONJ. HBOT involves breathing pure oxygen in a pressurized chamber, which can help improve blood flow to the affected area and promote tissue healing.
Conclusion
Osteonecrosis of the jaw is a complex condition that requires careful management and coordination between dental and medical professionals. While rare, ONJ can have significant implications for oral health and quality of life, particularly in patients undergoing certain medical treatments. By understanding the causes, symptoms, and treatment options for ONJ, patients and healthcare providers can work together to minimize the risk of complications and optimize outcomes for affected individuals.