A loose dental crown is a common dental issue that can cause discomfort and compromise oral health if not addressed promptly. Dental crowns are designed to restore the function and appearance of damaged teeth, but various factors can lead to their loosening over time. Understanding the causes, recognizing the symptoms, and knowing the appropriate steps to take can help manage this situation effectively.
Table of Contents
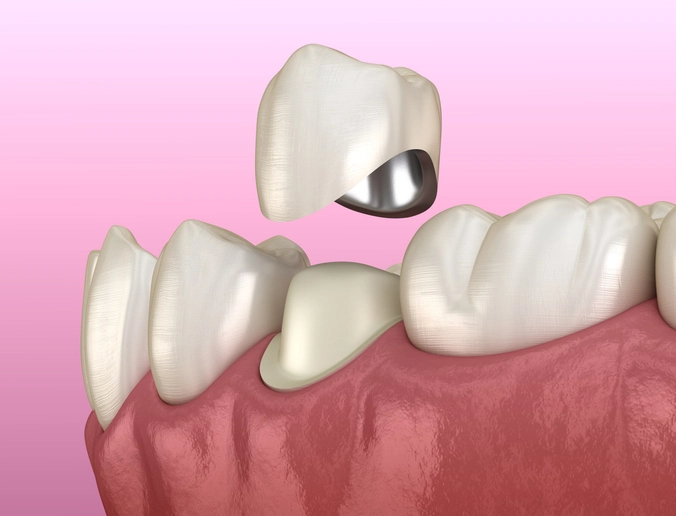
ToggleWhat Is a Dental Crown?
A dental crown is a cap placed over a damaged or decayed tooth to restore its shape, size, strength, and appearance. Crowns are commonly used after procedures like root canals, to cover large fillings, or to protect weak teeth from breaking. They can be made from various materials, including porcelain, ceramic, metal alloys, or a combination of materials.
Causes of a Loose Dental Crown
Dental crowns are designed to be durable and long-lasting, often staying in place for 10 to 15 years or more with proper care. However, they are not indestructible. Several factors can contribute to a crown becoming loose over time. Understanding these causes can help patients take preventive measures and know when to seek dental intervention.
1. Tooth Decay Beneath the Crown
Even though a crown covers the visible part of a tooth, the underlying natural tooth is still vulnerable to decay—especially near the margins where the crown meets the tooth. Plaque and food particles can accumulate around these edges, particularly if oral hygiene is poor. Over time, this can lead to cavities forming beneath the crown. As the decay progresses, it undermines the structural integrity of the tooth, compromising the crown’s foundation and causing it to loosen.
Key risk factors:
- Inadequate brushing and flossing
- High-sugar diets
- Poorly sealed crown margins
- Irregular dental check-ups
2. Degradation or Breakdown of Dental Cement
Dental crowns are typically held in place with a strong dental adhesive or cement. Over time, this material can degrade due to normal wear and tear, chemical exposure (from acidic foods and beverages), or poor initial bonding during placement. When the cement starts to wear away, the crown may begin to shift, wiggle, or fall off entirely.
Common contributors to cement failure:
- Long-term exposure to acidic drinks (like soda, wine, or citrus juice)
- Saliva contamination during crown placement
- Improper curing or insufficient cement application
3. Bruxism (Teeth Grinding and Clenching)
Bruxism refers to the habit of grinding or clenching teeth, often unconsciously during sleep or times of stress. The excessive pressure exerted on teeth during grinding can cause wear and tear not only on natural teeth but also on dental restorations like crowns. Over time, the crown may loosen or even fracture under these forces.
Warning signs of bruxism:
- Jaw pain or soreness, especially in the morning
- Flattened or chipped teeth
- Unexplained headaches
- Noisy grinding sounds during sleep (reported by a partner)
Preventive measure:
Wearing a nightguard (occlusal splint)
4. Trauma or Injury to the Mouth
A direct impact to the mouth—such as from a fall, sports injury, or car accident—can dislodge a crown or cause microfractures in the underlying tooth. Even biting down on something unexpectedly hard, like a popcorn kernel or ice, can cause trauma sufficient to loosen a crown.
Tips to reduce risk:
- Wear a mouthguard during contact sports
- Avoid chewing ice or hard candies
- Be cautious with unexpected hard textures in food
5. Chewing Hard or Sticky Foods
Certain foods can exert undue force on crowns. Hard items (like nuts, hard candies, and bones) can chip or crack a crown, while sticky foods (like caramel, chewing gum, or dried fruit) can pull the crown away from the tooth. Repeated chewing on these types of foods weakens the bond between the crown and the natural tooth structure.
Problematic foods include:
- Taffy, gummy candies, and licorice
- Hard nuts and seeds
- Popcorn (especially unpopped kernels)
- Jerky or hard crusty bread
6. Improper Crown Fit or Placement
Sometimes, the issue stems from how the crown was initially made or placed. A poorly fitted crown may not fully seal the underlying tooth or might not sit evenly on the tooth surface. This can lead to rocking, shifting, or loosening over time. It can also create small gaps where bacteria can infiltrate and cause decay.
Causes of improper fit:
- Inaccurate tooth impressions
- Manufacturing defects in lab-fabricated crowns
- Errors during crown cementation
7. Natural Tooth Wear or Structural Weakness
Over time, the underlying tooth structure can change. This can happen due to gradual erosion, root resorption, or the weakening of the tooth from previous dental work. When the natural tooth wears down or fractures, it may no longer provide a stable base for the crown, leading to loosening or failure.
Common scenarios:
- Extensive dental restorations weakening the tooth
- Root canal-treated teeth that haven’t been reinforced
- Age-related changes in tooth density
8. Gum Recession or Periodontal Disease
As gums recede due to aging or gum disease, more of the tooth beneath the crown becomes exposed. This can affect how well the crown fits and can make it more prone to catching food or bacteria. Periodontal issues can also weaken the tooth’s support structure, increasing the chance of the crown loosening or falling out.
Symptoms to watch for:
- Bleeding or swollen gums
- Chronic bad breath
- Exposed tooth roots
- Loose teeth or shifting bite
9. Repeated Crown Removal and Recementation
In some cases, a crown may need to be removed and re-cemented multiple times due to various reasons (such as root canal treatment or dental cleaning beneath the crown). Repeated manipulation of the crown weakens its ability to stay tightly sealed to the tooth, increasing the risk of future loosening.
Recognizing a Loose Crown
Early identification of a loose dental crown is crucial for preventing more serious dental complications. Often, people may not immediately notice that a crown is loose, especially if there’s no immediate pain or the movement is subtle. However, certain signs and symptoms can help alert you to a potential problem. Recognizing these indicators early on can save you from infection, further decay, or the need for more invasive dental work later.
Below are the most common and important signs to watch for:
1. Unusual Movement or Wiggling
One of the most obvious signs of a loose crown is that it no longer feels secure. You may notice slight movement when you chew, bite, or touch the crown with your tongue. A well-fitted crown should feel exactly like a natural tooth—firm and immobile.
How to detect it:
- Gently press the crown with your tongue or finger to check for movement.
- Chew on both sides of your mouth and pay attention to any sensation of rocking or shifting.
2. Sensitivity to Hot, Cold, or Sweet Foods
Sensitivity is a red flag that something is wrong beneath or around the crown. If a crown becomes loose, it may expose parts of the underlying tooth or allow fluids and bacteria to seep underneath. This exposure often leads to increased sensitivity to temperature and sugar.
Typical symptoms:
- Sharp or lingering pain when drinking cold water or hot coffee.
- Tingling or mild pain after consuming sugary snacks.
- Pain that persists even after the stimulus is removed, indicating possible decay under the crown.
3. Pain or Discomfort While Chewing
Pain when chewing is another key indicator. This can result from:
- Pressure on exposed areas of the tooth.
- Movement of the crown pinching the gum.
- Loosening of the crown irritating surrounding tissues or nerves.
What to notice:
- Discomfort that worsens when biting down.
- A feeling that the tooth is “off” or not aligned with your bite.
- A clicking sensation when you chew.
4. A Feeling That Something is “Off”
Sometimes, there’s no overt pain or sensitivity—but a crown that doesn’t feel right can still be loose. Patients often describe it as a “foreign feeling” in their mouth, or they instinctively begin avoiding chewing on that side.
Subtle clues:
- Uneven bite or changes in how your teeth meet when you close your mouth.
- A sudden awareness of the crown’s presence after months or years of not noticing it.
- Discomfort when talking or resting your mouth.
5. Visible Gaps Around the Crown
In a healthy situation, a crown fits snugly against the gum line, covering the prepared tooth underneath. If you see a gap between the crown and the gum, that means it’s not seated properly. This visible separation is often a sign that either the cement has failed or the underlying tooth has changed shape due to decay.
What to look for:
- Gaps or shadowing at the base of the crown.
- Dark lines near the gumline that weren’t there before.
- Slight lifting of the crown on one side.
6. A Bad Taste or Odor
An unpleasant taste or smell near a crowned tooth can be caused by bacteria trapped beneath the loose crown. When the seal between the crown and tooth is broken, food debris and bacteria may enter and begin to decay, creating odor and taste issues.
Possible signs:
- A persistent metallic or sour taste.
- Bad breath that doesn’t improve with brushing or mouthwash.
- A foul smell when flossing around the crown.
7. Bleeding or Inflamed Gums Around the Crown
When a crown loosens, it can irritate or injure the surrounding gum tissue. You might notice redness, swelling, or bleeding, especially when brushing or flossing. These symptoms can also mimic or contribute to gum disease.
Symptoms to track:
- Inflamed or puffy gums around the crown.
- Bleeding during routine brushing or flossing.
- Tenderness or itching in the gum area adjacent to the crown.
8. Crown Detachment or Falling Out
In some cases, the crown may not just loosen—it can fall out entirely. This is often preceded by the above signs, but sometimes it happens without much warning. If a crown comes off:
- Store it safely and bring it to your dentist.
- Do not attempt to glue it back yourself with household adhesives.
What to do:
- Avoid chewing on that side.
- Keep the area clean to prevent infection.
- Use dental wax or over-the-counter temporary cement as a short-term fix.
Immediate Steps to Take
If you suspect that a dental crown has become loose, taking quick and appropriate action can prevent further damage to your tooth and protect your overall oral health. While it’s crucial to see a dentist promptly, there are several things you can do in the meantime to minimize discomfort, prevent complications, and protect the tooth from exposure.
Here’s a breakdown of the key steps to follow immediately:
1. Stop Using the Affected Side of Your Mouth
If you notice your crown feels loose or wobbly, avoid chewing food on that side of your mouth. Putting pressure on a loose crown can worsen the situation, causing:
- Further loosening or complete detachment
- Damage to the underlying tooth
- Pain or irritation of the surrounding gum tissue
Tips:
- Shift your chewing to the opposite side.
- Stick to soft foods that don’t require vigorous chewing.
- Avoid biting into food with your front teeth if the crown is on an anterior tooth.
2. Avoid Sticky, Crunchy, or Hard Foods
Hard or sticky foods can pull a loose crown off or push it further out of place. They may also cause cracks or damage to the crown and the tooth beneath it. Until you see your dentist, avoid the following:
- Chewing gum
- Caramel, toffee, and other sticky sweets
- Ice, hard nuts, popcorn kernels
- Raw carrots, crusty bread, and tough meats
Instead, opt for:
- Soft-cooked vegetables
- Mashed potatoes, yogurt, scrambled eggs
- Smoothies and protein shakes
3. Keep the Area Clean
Maintaining good oral hygiene is vital to prevent bacteria from entering the gap between the crown and the tooth. Even though the crown is compromised, cleaning around it gently can prevent infection or decay from worsening.
How to clean safely:
- Brush gently around the loose crown with a soft-bristled toothbrush.
- Use fluoride toothpaste to help protect exposed tooth structure.
- Floss carefully around the crown—slide the floss out rather than snapping it up or down, which could dislodge the crown further.
- Rinse with warm salt water or an antiseptic mouthwash to reduce bacteria and soothe irritated gums.
4. Inspect the Crown (But Do Not Force It)
If the crown feels extremely loose or has partially come off, try to examine it carefully. However, do not attempt to remove it forcefully, as this could damage the underlying tooth or cause pain. If it does come off:
- Rinse it with water to remove debris.
- Store it in a clean, dry container or plastic bag.
- Bring it with you to your dental appointment—it may be reusable if intact.
Warning signs that removal may be necessary:
- Pain or swelling around the crown
- The crown moves significantly or falls off on its own
- Sharp edges of the tooth or crown are causing irritation
5. Use Temporary Dental Cement (If Necessary)
Over-the-counter dental cement (available at most pharmacies) can be a useful short-term solution if the crown has fallen off but is otherwise undamaged. It can help protect the exposed tooth and prevent further discomfort until you get to your dentist.
Steps for temporary reattachment:
- Clean the crown and your tooth with warm water (no soap or chemicals).
- Dry both surfaces thoroughly.
- Apply a small amount of dental cement inside the crown.
- Gently place it back onto the tooth and bite down lightly to ensure it seats correctly.
- Wipe away excess cement.
- Avoid chewing with the crown until your dentist confirms it is secure.
Cautions:
- Do not use super glue or household adhesives.
- This is a temporary measure, not a substitute for professional care.
6. Manage Discomfort or Pain
If you’re experiencing soreness or sensitivity, managing the pain until your appointment can make a significant difference. You may try:
- Over-the-counter pain relievers (ibuprofen or acetaminophen)
- Salt water rinses to reduce inflammation
- Avoiding hot, cold, or sweet foods and beverages
- Applying a cold compress to the outside of the mouth for swelling
If the pain becomes severe or is accompanied by fever or swelling, contact your dentist or seek emergency dental care—this could indicate an infection or abscess.
7. Protect Sharp Edges (If the Crown Falls Off)
If your crown has come off and the exposed tooth feels rough or sharp, it can injure your tongue, lips, or cheek. Use a piece of dental wax (available at pharmacies or in orthodontic kits) to cover sharp areas temporarily until you see the dentist.
8. Call Your Dentist Promptly
Even if you’re not experiencing major discomfort, a loose crown should be treated by a professional as soon as possible. Leaving it untreated increases the risk of:
- Decay under the crown
- Tooth fracture
- Infection or inflammation of surrounding tissues
- Complete crown loss, requiring a new crown or even root canal therapy
When calling your dentist:
- Explain when the crown became loose and any symptoms you’re experiencing.
- Mention if you used temporary cement or if the crown has come off completely.
- Request an urgent appointment if there is pain, bleeding, or the crown is completely detached.
9. Document the Issue (Optional but Useful)
If the crown is visibly shifting or causing discomfort, taking photos can be helpful. These can be shown to your dentist if you’re unable to get in quickly. It can also serve as documentation if dental insurance becomes involved.
Tips:
- Take clear, close-up photos under good lighting.
- Include both the crown and surrounding gum tissue.
- Note the timeline of when symptoms began and any home remedies used.
Summary: Immediate Do’s and Don’ts
✅ DO:
- Avoid chewing on the affected side.
- Keep the area clean with gentle brushing and rinsing.
- Use over-the-counter dental cement if the crown falls out.
- Contact your dentist promptly.
❌ DON’T:
- Ignore the issue or delay treatment.
- Chew hard or sticky foods.
- Try to force the crown off or reattach it with non-dental glue.
- Leave sharp or exposed edges unprotected.
Potential Complications
A loose dental crown may seem like a minor annoyance at first, especially if it’s not causing immediate pain. However, if left unaddressed, it can lead to a cascade of serious dental issues. Crowns are designed not only for cosmetic reasons but also to protect the underlying tooth from further damage and decay. Once the seal between the crown and tooth is compromised, your tooth becomes vulnerable.
Below are the major complications that can arise from ignoring a loose crown:
1. Tooth Decay and Cavities Beneath the Crown
When a crown becomes loose, the protective barrier between your natural tooth and the oral environment breaks down. This allows bacteria, food particles, and plaque to infiltrate the space between the crown and tooth, especially near the gum line. Since this area is hard to clean effectively, it creates the perfect environment for decay to develop under the crown—often undetected until it’s too late.
What can happen:
- Progressive decay may erode the tooth underneath, weakening its structure.
- The tooth may eventually require a new crown or additional dental work such as a filling or root canal.
- If decay goes unchecked, it may result in the total loss of the tooth.
2. Infection or Abscess Formation
One of the most dangerous complications of a loose crown is the potential for infection. As bacteria enter the compromised seal, they can reach the dental pulp—the soft inner tissue of the tooth containing nerves and blood vessels. If this occurs, a painful infection or abscess (a pocket of pus) may develop.
Signs of a possible infection:
- Persistent toothache or throbbing pain
- Sensitivity to pressure or temperature
- Swelling in the gums or face
- Bad breath or a foul taste in the mouth
- Fever or swollen lymph nodes (in severe cases)
Outcome:
- You may require a root canal to remove the infected pulp.
- In more severe situations, the tooth may need to be extracted.
3. Damage to the Underlying Tooth
Crowns are meant to protect structurally compromised teeth—teeth that may have had large fillings, cracks, or root canal therapy. Once a crown becomes loose, that protection is diminished. Normal chewing forces or even accidental biting on hard foods can fracture the exposed tooth, especially if it’s already weakened.
Consequences:
- The tooth may fracture vertically or horizontally.
- Damage could extend below the gum line, making the tooth non-restorable.
- Extraction followed by a dental implant or bridge may be necessary.
4. Gum Irritation and Periodontal Disease
Loose crowns can irritate the surrounding gum tissue, especially if they shift when chewing or if food gets trapped around them. This irritation can lead to inflammation, recession of the gum line, and the beginning stages of periodontal (gum) disease.
Symptoms of gum complications:
- Red, swollen, or bleeding gums near the affected crown
- Tenderness or pain around the tooth
- Receding gum line that exposes more of the tooth root
- Formation of pockets between the gum and tooth where bacteria accumulate
If untreated:
- Gingivitis can progress to periodontitis, a more serious form of gum disease.
- Bone loss around the tooth can occur, eventually leading to tooth mobility and loss.
5. Crown Displacement or Loss
A loose crown is at constant risk of falling off completely, often at inconvenient times—like during meals, at night, or while traveling. When a crown detaches unexpectedly:
- You may accidentally swallow or aspirate it.
- The exposed tooth may become extremely sensitive and painful.
- The aesthetics of your smile may be affected, especially if it’s a front tooth.
Recovery may require:
- Emergency dental visits
- Use of temporary crowns
- Full crown replacement (if damaged or swallowed)
6. Changes in Bite and Jaw Pain
A loose or shifting crown can subtly alter how your upper and lower teeth meet—your bite alignment. This imbalance can put undue pressure on your jaw joints (temporomandibular joints or TMJs), leading to discomfort and long-term complications.
Signs of bite-related issues:
- Clicking or popping in the jaw
- Pain in the jaw, neck, or ears
- Difficulty opening or closing the mouth
- Increased tooth wear from uneven pressure
Over time:
- Bite misalignment can lead to bruxism (grinding), worsening the damage to other teeth and restorations.
- TMJ disorders may develop, requiring additional therapy or intervention.
7. Aesthetic and Functional Issues
Dental crowns also serve cosmetic and functional roles—especially for visible front teeth or molars critical for chewing. A loose or fallen crown can affect your appearance, speech, and confidence, as well as make it difficult to eat certain foods.
You may experience:
- Difficulty chewing effectively
- Pronunciation issues due to gaps in teeth
- Self-consciousness about your smile
8. Increased Treatment Complexity and Cost
Delaying treatment for a loose crown can turn a simple, inexpensive fix into a complex—and costly—procedure. For example:
- A re-cementation that might have cost under $200 could become a root canal and crown replacement costing over $2,000.
- Ignoring the issue may necessitate full tooth replacement via implant or bridge.
Other considerations:
- Insurance may not fully cover replacements if the damage was due to neglect.
- Dental emergencies may disrupt work, travel, or other responsibilities.
Summary: Why You Should Never Ignore a Loose Crown
| Complication | Possible Outcome |
|---|---|
| Tooth Decay | Cavity beneath crown, need for new crown or filling |
| Infection | Root canal, abscess, or extraction |
| Tooth Fracture | Irreparable damage requiring extraction |
| Gum Irritation | Periodontal disease and gum recession |
| Crown Loss | Emergency visit, loss of aesthetics/function |
| Bite Issues | TMJ disorders and chronic jaw pain |
| Increased Cost | More extensive and expensive treatment required |
Treatment Options
Once a dental crown becomes loose, it’s essential to seek professional treatment to prevent further complications and to restore the integrity and function of your tooth. The treatment your dentist recommends will depend on several factors, including the condition of the crown, the state of the underlying tooth, the presence of any decay or infection, and whether the crown can be reused.
Below is a comprehensive overview of the most common and effective treatment options available:
1. Re-cementing the Existing Crown
If the crown has simply become dislodged due to worn-out dental cement but is otherwise in good condition—and the underlying tooth is healthy—your dentist may be able to re-cement it.
Procedure:
- The dentist will clean both the inside of the crown and the surface of the tooth.
- Any remaining old cement is removed.
- A fresh bonding agent or dental cement is applied.
- The crown is repositioned and securely bonded back in place.
When it’s viable:
- No decay or damage to the tooth or crown
- Crown fits well and hasn’t changed shape
- Crown and tooth alignment remains proper
Benefits:
- Cost-effective
- Quick procedure—often done in a single visit
- Preserves the original crown
2. Replacing the Crown with a New One
If the crown is damaged, has a poor fit, or if it no longer seals the tooth properly due to changes in the tooth structure, your dentist may recommend replacing it with a new crown.
Reasons for replacement:
- Cracked, chipped, or worn-out crown
- Recurrent decay under the crown
- Crown no longer fits due to gum recession or tooth movement
- Cosmetic concerns with older or discolored crowns
Procedure:
- The old crown is removed.
- The underlying tooth is cleaned and, if necessary, reshaped.
- New impressions are taken or a digital scan is done.
- A temporary crown is placed.
- Once the permanent crown is fabricated (typically 1–2 weeks later), it is bonded securely.
Materials for new crowns may include:
- Porcelain or ceramic (aesthetic, tooth-colored)
- Porcelain-fused-to-metal (strength and aesthetics)
- Gold alloy (durability, often used for molars)
- Zirconia (very strong and aesthetic)
3. Repairing the Crown or Underlying Tooth
Sometimes, both the crown and the tooth may have minor damage that doesn’t require a full replacement. Your dentist may be able to make repairs, particularly if the issue is minor and isolated.
For the crown:
- Small chips in porcelain can be smoothed or filled with composite material.
- Hairline cracks may be sealed if the crown is still functional.
For the tooth:
- Decay beneath the crown can sometimes be treated without full crown replacement.
- Minor fractures can be restored with dental bonding.
Limitations:
- Repairs are typically temporary.
- Most repairs are not suitable for major cracks or recurrent decay.
4. Root Canal Therapy (If the Pulp is Infected or Exposed)
If decay beneath the crown has reached the pulp of the tooth or if an infection has developed, root canal treatment may be required before a new crown can be placed.
Signs that a root canal may be needed:
- Severe or persistent pain
- Swelling or abscess near the affected tooth
- Sensitivity to hot or cold that lingers
- Darkening of the tooth underneath the crown
Procedure:
- The dentist removes the infected pulp tissue.
- The canal is cleaned, shaped, and sealed.
- A post may be placed for added support.
- The tooth is then covered with a new crown.
5. Post and Core Build-Up
If a significant portion of the natural tooth is missing or damaged, your dentist may need to build up the tooth structure before reattaching or replacing a crown. This is especially common for teeth that have had root canals.
What it involves:
- A post is inserted into the root canal for structural support.
- A core material (often composite or dental buildup resin) is placed around the post to recreate the shape of the original tooth.
- The crown is then fitted over this new foundation.
Indications:
- Insufficient natural tooth remains to hold a crown securely
- Tooth weakened from large fillings, decay, or previous restorations
6. Tooth Extraction (When the Tooth is Beyond Repair)
In rare but serious cases, the underlying tooth may be too damaged or decayed to be saved. If the crown comes loose and reveals a severely fractured, abscessed, or decayed tooth that can’t support a new crown or post, extraction may be the only viable option.
Reasons for extraction:
- Vertical root fracture
- Advanced periodontal disease with bone loss
- Non-restorable decay
- Repeated failed root canals
Follow-up options:
- Dental implant with a crown
- Dental bridge
- Partial denture
7. Temporary Crown Placement
If the permanent crown cannot be re-cemented immediately—whether due to lab time, treatment of underlying issues, or healing time needed—your dentist may place a temporary crown to protect the tooth.
Benefits:
- Preserves aesthetics and function
- Shields the tooth from sensitivity and damage
- Allows time for fabrication of a custom permanent crown
8. Orthodontic or Surgical Adjustment (Rare Cases)
In uncommon situations, the underlying issue may be due to changes in your bite, misalignment, or tooth positioning. A loose crown could be a symptom of an occlusal (bite) problem that requires more complex intervention.
Potential solutions:
- Occlusal adjustment (shaving down opposing teeth)
- Orthodontic treatment to realign teeth
- Crown lengthening surgery to expose more of the tooth for better crown retention
These treatments are typically used only after repeated crown failures or if bite issues are causing stress to multiple crowns or restorations.
Summary: Matching Treatment to the Problem
| Problem | Treatment Option |
|---|---|
| Intact crown, healthy tooth | Re-cementation |
| Damaged or worn crown | Replacement with new crown |
| Tooth decay under crown | Decay removal + new crown or root canal |
| Fractured tooth under crown | Post and core build-up or extraction |
| Pain or infection | Root canal therapy |
| Crown fell off completely | Temporary crown, then permanent restoration |
| Bite-related crown failure | Occlusal adjustment or orthodontics |
Preventing Future Issues
Dental crowns are designed to be strong, durable, and long-lasting—but like any dental restoration, their longevity depends heavily on how well they are cared for. With proper maintenance and attention to oral health habits, you can significantly reduce the risk of your crown becoming loose, damaged, or failing prematurely.
Below are the key strategies for preventing future crown problems:
1. Practice Excellent Oral Hygiene
Although a dental crown itself cannot decay, the tooth underneath it can. Maintaining proper oral hygiene is essential to prevent decay at the margin where the crown meets the natural tooth, as well as to preserve the health of your gums.
Daily habits to follow:
- Brush at least twice a day with fluoride toothpaste, paying extra attention to the gumline around the crown.
- Floss daily to remove plaque and food particles between the crown and neighboring teeth. Be gentle when flossing around the crown—slide the floss out rather than pulling upward to avoid loosening the crown.
- Use an antiseptic mouthwash once a day to help kill bacteria that brushing and flossing may miss.
2. Visit Your Dentist Regularly
Routine dental check-ups are one of the most effective ways to catch and correct problems before they escalate. During a dental visit, your dentist will:
- Examine the integrity of your crown and the underlying tooth
- Check for signs of decay, gum disease, or improper bite
- Professionally clean areas that are hard to reach at home
- Take X-rays (if necessary) to detect hidden problems beneath the crown
Recommendation:
Schedule professional cleanings and exams every 6 months (or more frequently if recommended).
3. Avoid Hard, Sticky, or Crunchy Foods
One of the most common causes of crown failure is physical stress from the foods we eat. Crowns, especially porcelain ones, can crack or become loose when exposed to hard biting forces.
Foods to avoid or be cautious with:
- Ice cubes (never chew them)
- Popcorn kernels
- Hard candy and nuts
- Sticky candies like caramel, taffy, or gummy bears
- Chewy breads or jerky
Tip: If you must eat such foods, chew on the opposite side of your mouth (away from the crown) and avoid biting directly into them with front crowns.
4. Wear a Nightguard if You Grind Your Teeth (Bruxism)
Bruxism (grinding or clenching your teeth, often during sleep) can exert significant pressure on your crowns and natural teeth. Over time, this can lead to micro-movements that loosen the crown, crack the porcelain, or cause damage to the underlying tooth.
What to do:
- Ask your dentist to evaluate you for signs of bruxism.
- If diagnosed, use a custom nightguard to protect your teeth while you sleep.
- Stress-reducing techniques (like meditation or biofeedback) may also help reduce grinding.
5. Avoid Using Teeth as Tools
Using your teeth to open packages, rip tape, hold items, or bite nails is extremely damaging—not just to crowns but to all your teeth. This habit can cause a crown to chip, crack, or become dislodged unexpectedly.
Safe alternatives:
- Use scissors or proper tools instead of your teeth.
- Keep a nail clipper or package opener handy to avoid temptation.
6. Be Mindful of Changes in Your Bite
If your bite feels “off” after dental work, or if you suddenly notice a clicking, shifting, or uncomfortable bite pattern, don’t ignore it. A misaligned bite can lead to uneven forces being applied to your crown and surrounding teeth, increasing the risk of loosening.
What to watch for:
- New or increased tooth sensitivity
- Difficulty chewing on one side
- Feeling that upper and lower teeth don’t align properly
- Jaw soreness or headaches in the morning
Action step:
Schedule a bite evaluation with your dentist if any changes occur.
7. Consider Crown Material Selection Carefully
The type of crown material used can affect how long it lasts and how well it withstands the forces in your mouth. Understanding the differences and making the right choice can prevent complications down the line.
Types of crowns and considerations:
- Porcelain or ceramic: Excellent aesthetics, best for front teeth, but may be more prone to chipping.
- Porcelain-fused-to-metal (PFM): Stronger than porcelain alone but may show a dark line at the gum line over time.
- Zirconia: Highly durable and fracture-resistant, suitable for molars or people with bruxism.
- Gold or metal alloy: Very durable, best for out-of-sight molars, and causes minimal wear to opposing teeth.
Talk to your dentist about the best material based on the location of the crown, your bite strength, and your aesthetic preferences.
8. Don’t Ignore Gum Health
The health of your gums directly affects the fit and longevity of your crown. Receding gums or periodontal disease can expose the crown’s margin and increase the risk of it becoming loose or of decay setting in underneath.
How to protect your gums:
- Floss daily and clean between your teeth.
- Use an electric toothbrush for more thorough cleaning along the gumline.
- Avoid tobacco products, which are a leading cause of gum disease.
- Eat a balanced diet rich in vitamin C, calcium, and antioxidants.
9. Address Dental Issues Promptly
Whether it’s minor discomfort, slight movement of a crown, or bleeding gums—act early. Prompt attention to emerging issues helps prevent complex and expensive treatments in the future.
Why early action matters:
- You may only need a quick adjustment or minor repair.
- Delayed care increases the risk of infection, fracture, and full crown failure.
- Dental insurance may cover repairs but not full replacements if due to neglect.
10. Educate Yourself and Stay Informed
Understanding the role your crown plays in your dental health helps you make informed choices about its care. Don’t hesitate to ask your dentist questions like:
- “What signs should I watch for?”
- “How long should my crown last?”
- “What foods or habits should I avoid for my specific crown material?”
The more proactive and knowledgeable you are, the better you can maintain your dental restorations for the long haul.
Summary: Prevention is Better (and Cheaper) Than Repair
| Preventive Habit | Benefit |
|---|---|
| Daily brushing and flossing | Prevents decay under the crown |
| Regular dental check-ups | Early detection of issues |
| Nightguard for bruxism | Protects crown from excessive pressure |
| Avoid hard/sticky foods | Reduces risk of dislodgement or breakage |
| Monitor bite changes | Prevents jaw issues and crown stress |
| Keep gums healthy | Maintains proper crown fit and support |
Conclusion
A loose dental crown is a manageable issue when addressed promptly. Recognizing the signs, taking immediate precautions, and seeking professional dental care can prevent complications and ensure the longevity of your dental restorations. Maintaining good oral hygiene and regular dental visits are key to preventing future problems with crowns and overall dental health.