Gastroesophageal reflux disease (GERD), also known as acid reflux, is a chronic digestive disorder that affects millions of people worldwide. Characterized by the backward flow of stomach acids into the esophagus, GERD can cause symptoms such as heartburn, regurgitation, and difficulty swallowing. While GERD is primarily associated with digestive health, its effects extend beyond the esophagus and stomach. One of the lesser-known yet significant consequences of GERD is its impact on oral health, particularly on the teeth and gums.
The acidic nature of stomach contents that rise into the esophagus can reach the oral cavity, potentially causing dental erosion, gum irritation, and other oral health issues. This article explores the relationship between GERD and oral health, focusing on how acid reflux can damage teeth, affect oral tissues, and contribute to various dental problems. Additionally, it offers insights into preventive measures and treatments to mitigate these effects.
Table of Contents
ToggleUnderstanding GERD: A Brief Overview
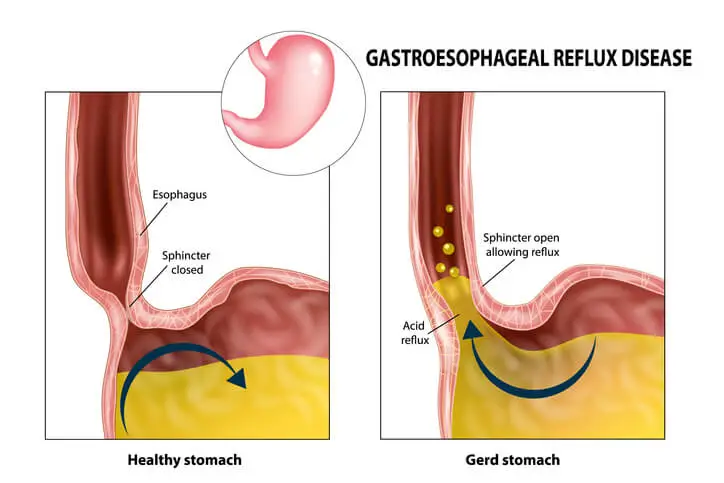
GERD is caused by the dysfunction of the lower esophageal sphincter (LES), a muscular ring that acts as a valve between the esophagus and the stomach. Normally, the LES opens to allow food to enter the stomach and closes to prevent stomach acid from flowing back into the esophagus. In individuals with GERD, the LES fails to close properly or relaxes too frequently, allowing acid and other stomach contents to escape into the esophagus.
Common symptoms of GERD include:
- Heartburn (a burning sensation in the chest or throat)
- Acid regurgitation (sour or bitter-tasting liquid in the mouth)
- Difficulty swallowing (dysphagia)
- Chest pain
- Chronic cough or hoarseness
GERD is a chronic condition, meaning it requires long-term management. While medications and lifestyle changes can help control the symptoms, many people may not be aware of the impact GERD has on their oral health.
Impacts of GERD on Oral Health
Oral cavity is sensitive to changes in pH levels. Under normal circumstances, saliva helps neutralize acids and maintain an environment conducive to healthy teeth and gums. However, the continuous exposure of the oral cavity to stomach acids from GERD can upset this balance, leading to several oral health issues. These include dental erosion, increased risk of tooth decay, gum inflammation, and even complications such as halitosis (bad breath). The following sections explore these effects in detail.
- Dental Erosion
- Increased Risk of Tooth Decay
- Gum Disease and Soft Tissue Irritation
- Halitosis (Bad Breath)
- Dry Mouth (Xerostomia)
Dental Erosion: The Destruction of Tooth Enamel
One of the most significant oral health consequences of GERD is dental erosion. Dental erosion occurs when the enamel—the hard, protective outer layer of the teeth—is worn away by acid exposure. Stomach acids have a very low pH (around 1 to 3), making them highly corrosive to tooth enamel, which begins to demineralize at a pH level of around 5.5.
Stages of Dental Erosion Due to GERD:
- Initial stage: In the early stages, acid exposure can soften the enamel, making the teeth more vulnerable to mechanical wear from brushing or grinding.
- Advanced stage: Over time, repeated acid attacks can thin the enamel, causing teeth to become more sensitive to hot, cold, or sweet foods and drinks.
- Severe stage: In severe cases, the erosion may reach the underlying dentin, the softer layer beneath the enamel, leading to significant tooth sensitivity, discoloration, and an increased risk of cavities.
Symptoms of Dental Erosion in GERD Patients:
- Teeth become smooth and shiny, especially on the chewing surfaces
- Increased tooth sensitivity, particularly to temperature changes
- Yellowing of the teeth due to exposure of the underlying dentin
- Cracks, chips, or thinning of the teeth
- Flat or worn-down biting edges
Why Enamel Erosion is Dangerous:
Enamel plays a crucial role in protecting the teeth from physical damage and decay. Once enamel is lost, it cannot be regenerated, and the teeth become more susceptible to caries (tooth decay) and other dental problems. In extreme cases, dental erosion can lead to tooth loss.
Increased Risk of Tooth Decay
GERD patients are at a higher risk of developing tooth decay. The acid exposure from GERD weakens tooth enamel, making it more prone to bacterial invasion. In a healthy mouth, bacteria are kept in check by saliva, which helps neutralize acids and wash away food particles. However, the acidic environment created by GERD can upset this balance, allowing harmful bacteria to thrive and cause dental caries.
How GERD Contributes to Tooth Decay:
- Weakened enamel: As enamel erodes, the protective barrier is compromised, making it easier for bacteria to penetrate the tooth structure.
- Lower saliva production: GERD can sometimes lead to dry mouth (xerostomia), reducing saliva flow and its ability to neutralize acids and wash away bacteria.
- Changes in oral pH: The acidic environment in the mouth caused by GERD can promote the growth of acid-producing bacteria, further contributing to tooth decay.
Gum Disease and Soft Tissue Irritation
While the primary focus of GERD’s impact on oral health is often on the teeth, it can also affect the soft tissues of the mouth, including the gums, tongue, and throat. Chronic acid exposure can irritate and inflame these tissues, leading to conditions such as:
- Gingivitis: Inflammation of the gums, which can cause redness, swelling, and bleeding.
- Periodontitis: A more advanced form of gum disease that affects the bone and supporting structures of the teeth, potentially leading to tooth loss.
- Burning mouth syndrome: Some GERD patients experience a burning sensation in the mouth or throat due to acid irritation.
Additionally, stomach acid that enters the mouth can cause soreness or ulceration of the oral mucosa (the lining of the mouth), making it painful to eat or drink. Persistent inflammation of the gums and soft tissues can also contribute to the development of gum disease.
Halitosis (Bad Breath)
Bad breath, or halitosis, is a common complaint among individuals with GERD. The regurgitation of stomach acid and partially digested food into the mouth can leave a sour, unpleasant odor. Additionally, the acidic environment in the mouth promotes the growth of odor-causing bacteria, further contributing to bad breath.
Dry Mouth (Xerostomia)
GERD can sometimes result in dry mouth, a condition characterized by a decrease in saliva production. Saliva is essential for maintaining oral health because it helps neutralize acids, wash away food particles, and prevent bacterial overgrowth. When saliva production is reduced, the risk of tooth decay, gum disease, and other oral health problems increases.
Xerostomia can occur in GERD patients for several reasons:
- Medications: Some medications used to treat GERD, such as proton pump inhibitors (PPIs) and H2 blockers, can cause dry mouth as a side effect.
- Mouth breathing: GERD patients who experience nasal congestion or breathing difficulties may be more likely to breathe through their mouths, which can dry out the oral tissues.
- Dehydration: Frequent regurgitation and vomiting associated with severe GERD can lead to dehydration, reducing saliva flow.
Preventive Measures for Protecting Oral Health in GERD Patients
Given the significant impact GERD can have on oral health, it is crucial for individuals with GERD to take proactive steps to protect their teeth and gums. Here are some practical strategies for minimizing the oral health risks associated with GERD:
- Control Acid Reflux with Medical Management
- Practice Good Oral Hygiene
- Use Enamel-Protecting Products
- Stay Hydrated
- Regular Dental Check-ups
Control Acid Reflux with Medical Management
The first step in preventing GERD-related oral health problems is to manage the underlying condition effectively. This may involve a combination of lifestyle changes, medications, and dietary adjustments to reduce acid reflux and prevent stomach acids from reaching the mouth. Common treatments for GERD include:
- Proton pump inhibitors (PPIs): These medications reduce the production of stomach acid, minimizing the risk of acid reflux.
- H2 blockers: These drugs decrease acid production and are often used in combination with PPIs.
- Antacids: Over-the-counter antacids can neutralize stomach acid and provide temporary relief from heartburn.
- Lifestyle changes: Avoiding trigger foods (such as spicy, fatty, or acidic foods), eating smaller meals, and maintaining a healthy weight can help reduce GERD symptoms.
Practice Good Oral Hygiene
Proper oral hygiene is essential for preventing the oral health complications of GERD. Patients should focus on strengthening and protecting their teeth while maintaining a healthy oral environment. Key oral hygiene practices include:
- Brushing twice a day: Use a soft-bristled toothbrush and fluoride toothpaste to gently clean the teeth without causing further enamel damage. Avoid brushing immediately after a reflux episode to prevent additional erosion. Read more about brushing Techniques.
- Flossing daily: Flossing helps remove food particles and plaque from between the teeth, reducing the risk of gum disease and tooth decay.
- Rinsing with water or a fluoride mouthwash: After an acid reflux episode, rinsing the mouth with water can help neutralize acids. Using a fluoride mouthwash can also strengthen enamel and protect against decay.
- Chewing sugar-free gum: Chewing gum stimulates saliva production, which can help neutralize acid and protect the teeth.
Use Enamel-Protecting Products
GERD patients may benefit from using oral care products specifically designed to protect and strengthen enamel. These products include:
- Fluoride toothpaste: Fluoride helps remineralize and strengthen enamel, making it more resistant to acid attacks.
- Enamel-repair toothpaste: Some toothpaste formulations contain ingredients like calcium phosphate or hydroxyapatite, which can help repair and protect weakened enamel.
- Prescription fluoride treatments: In cases of severe enamel erosion, a dentist may recommend prescription-strength fluoride treatments to provide additional protection.
Stay Hydrated
Maintaining proper hydration is crucial for preventing dry mouth and promoting saliva production. GERD patients should drink plenty of water throughout the day to keep their mouths moist and help neutralize acids.
Regular Dental Check-ups
GERD patients should visit their dentist regularly for check-ups and cleanings. A dentist can monitor the condition of the teeth and gums, identify early signs of dental erosion or decay, and recommend appropriate treatments to protect oral health. In some cases, a dentist may apply dental sealants or fluoride varnishes to provide additional protection against acid damage.
Frequently Asked Questions (FAQs)
What are 4 symptoms of GERD?
- Heartburn (burning sensation in the chest)
- Acid reflux or regurgitation
- Difficulty swallowing (dysphagia)
- Chronic cough or sore throat
Does GERD go away?
GERD is a chronic condition that typically does not go away on its own. However, symptoms can be managed with lifestyle changes, medications, and in some cases, medical procedures.
What does living with GERD feel like?
Living with GERD can mean experiencing frequent heartburn, discomfort after eating, a sour taste in the mouth, and sometimes trouble sleeping due to acid reflux. Some people may also feel chest pain, bloating, or excessive burping.
How long does it take for GERD to turn into Barrett’s esophagus?
There is no set timeline, but chronic GERD over many years (often 5–10 years or more) increases the risk of developing Barrett’s esophagus. Regular monitoring by a doctor is essential if GERD symptoms persist.
What does Barrett’s esophagus feel like?
Barrett’s esophagus itself does not cause symptoms, but since it develops due to long-term GERD, people with this condition often experience persistent acid reflux, heartburn, and difficulty swallowing.
Can you eat bananas if you have Barrett’s esophagus?
Yes, bananas are generally safe for Barrett’s esophagus as they are low in acid and can help soothe the digestive tract. However, personal tolerance may vary.
What is the best way to reverse Barrett’s esophagus?
While Barrett’s esophagus cannot always be reversed, treatment focuses on preventing progression. This includes:
- Managing acid reflux with medications (PPIs, H2 blockers)
- Avoiding trigger foods
- Maintaining a healthy weight
- In severe cases, medical procedures like radiofrequency ablation (RFA)
What are the signs of a damaged esophagus?
- Difficulty swallowing (dysphagia)
- Painful swallowing
- Chest pain
- Chronic sore throat or hoarseness
- Bleeding (vomiting blood or black stools in severe cases)
What are the worst foods for Barrett’s esophagus?
- Spicy foods
- Citrus fruits and juices
- Tomatoes and tomato-based products
- Coffee and caffeine-containing beverages
- Alcohol
- Fatty, fried, and processed foods
- Chocolate and peppermint
Conclusion
Gastroesophageal reflux disease (GERD) is a chronic condition that affects not only the digestive system but also oral health. The frequent exposure of the teeth and gums to stomach acids can lead to dental erosion, increased risk of tooth decay, gum disease, and other oral health issues. Understanding the connection between GERD and oral health is essential for both patients and healthcare providers to implement effective preventive measures.
By managing acid reflux through medications, lifestyle changes, and proper oral hygiene, individuals with GERD can minimize the damage to their teeth and gums and maintain optimal oral health. Regular dental check-ups, the use of enamel-strengthening products, and staying hydrated are all important strategies for protecting the teeth and preventing the long-term consequences of acid reflux on oral health.
While GERD can present significant challenges, a proactive approach to both digestive and oral health can help individuals with this condition lead healthier, more comfortable lives.

Ankara Avukat
15 October 2024Thank you for this insightful post! I really appreciate the effort you put into creating such valuable content.