Bone Morphogenetic Proteins (BMPs) are a family of growth factors belonging to the transforming growth factor-beta (TGF-β) superfamily. Discovered by Dr. Marshall Urist in the 1960s, BMPs have emerged as critical agents in the regeneration of bone and other tissues. Their ability to induce osteogenesis, the formation of bone from undifferentiated mesenchymal cells, has made them a cornerstone in regenerative medicine. In dentistry and implantology, Bone Morphogenetic Proteins have redefined therapeutic approaches, providing enhanced outcomes in complex cases of bone loss, periodontal disease, and implant integration. This article explores the biology of BMPs, their applications in dentistry, and their transformative potential in implantology.
Table of Contents
ToggleBiology and Mechanism of Action of Bone Morphogenetic Proteins
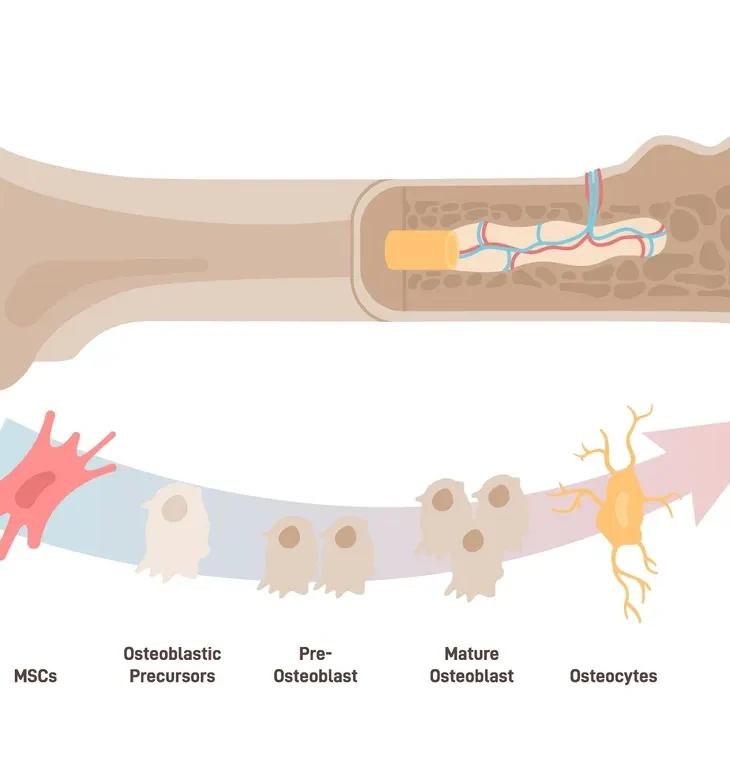
Bone Morphogenetic Proteins are signaling molecules that regulate the differentiation of mesenchymal stem cells into osteoblasts and chondroblasts. Among the 20 identified BMPs, BMP-2, BMP-4, and BMP-7 (also known as osteogenic protein-1, OP-1) have demonstrated the most significant osteoinductive potential.
Mechanism of Action
BMPs initiate bone formation through a multi-step process:
- Binding to Receptors
- Activation of SMAD Pathway
- Gene Expression
- Bone Formation
Binding to Receptors
BMPs bind to specific serine/threonine kinase receptors (BMPR-I and BMPR-II) on target cell membranes.
Activation of SMAD Pathway
The receptor-ligand interaction activates intracellular SMAD proteins, which translocate to the nucleus.
Gene Expression
SMAD complexes modulate the transcription of genes associated with osteoblast differentiation, such as Runx2 and osterix.
Bone Formation
Differentiation of mesenchymal stem cells into osteoblasts leads to matrix production and mineralization.
Clinical Applications of Bone Morphogenetic Proteins in Dentistry
Bone Morphogenetic Proteins have found extensive use in dentistry, particularly in periodontal regeneration, alveolar ridge augmentation, and maxillofacial reconstruction.
- Periodontal Regeneration
- Alveolar Ridge Augmentation
- Sinus Floor Elevation
- Maxillofacial Reconstruction
Periodontal Regeneration
Periodontal disease results in the loss of alveolar bone, periodontal ligament, and cementum. Traditional treatments, such as guided tissue regeneration (GTR), have limitations in predictability. BMPs offer a more reliable alternative due to their osteoinductive properties.
- BMP-2 and BMP-7 – These proteins stimulate periodontal ligament fibroblasts and osteoblasts, promoting bone and cementum regeneration.
- Clinical Outcomes – Studies have demonstrated superior attachment gain and bone fill when BMPs are used in conjunction with collagen membranes or scaffolds.
Alveolar Ridge Augmentation
Alveolar ridge resorption, a common consequence of tooth loss, poses a significant challenge for implant placement. BMPs facilitate ridge augmentation by promoting new bone formation.
- BMP-2 for Ridge Augmentation – BMP-2 is often delivered via an absorbable collagen sponge (ACS) or synthetic scaffolds to induce vertical and horizontal bone growth.
- Efficacy – Clinical trials have shown predictable outcomes in restoring ridge dimensions, enabling successful implant placement.
Sinus Floor Elevation
In cases of posterior maxilla atrophy, sinus augmentation is required for implant placement. Bone Morphogenetic Proteins, particularly BMP-2, are used as an alternative to autogenous bone grafts.
- Advantages – BMPs eliminate the need for secondary surgical sites, reducing morbidity and patient discomfort.
- Clinical Success – Studies report comparable or superior bone volume gain and implant survival rates with BMP-based sinus lifts.
Maxillofacial Reconstruction
Large defects resulting from trauma, tumors, or congenital anomalies necessitate advanced regenerative approaches. Bone Morphogenetic Proteins are employed in conjunction with custom scaffolds and osteoconductive materials for effective defect reconstruction.
- Case Studies – BMP-7 has been successfully used for mandibular reconstruction in patients with extensive bone loss.
Role of Bone Morphogenetic Proteins in Dental Implantology
The integration of Bone Morphogenetic Proteins into implantology has revolutionized treatment strategies, particularly in challenging cases of insufficient bone volume and compromised healing.
- Enhancing Osseointegration
- Applications in Peri-Implant Defects
- Immediate Implant Placement
- All-on-4 and Full-Arch Reconstructions
Enhancing Osseointegration
Osseointegration, the direct structural and functional connection between bone and a dental implant, is critical for implant success. BMPs accelerate this process by:
- Stimulating osteoblast differentiation around the implant.
- Enhancing the deposition of bone matrix at the implant surface.
Applications in Peri-Implant Defects
Bone Morphogenetic Proteins are particularly valuable in managing peri-implant defects, which can arise due to infection, mechanical stress, or insufficient bone at the time of placement.
- BMP-2 for Peri-Implantitis – Studies have shown that BMP-2 promotes regeneration of peri-implant bone, reversing the effects of peri-implantitis.
Immediate Implant Placement
In cases of immediate implant placement post-extraction, BMPs enhance socket healing and minimize resorption.
- Clinical Benefits – Faster osseointegration and higher implant stability are observed when BMPs are applied in conjunction with implants.
All-on-4 and Full-Arch Reconstructions
Patients requiring full-arch reconstructions often present with severe bone atrophy. Bone Morphogenetic Proteins enable bone augmentation procedures that support complex implant restorations like All-on-4 systems.
- BMP-7 in Full-Arch Cases – BMP-7 combined with titanium mesh scaffolds has demonstrated success in creating sufficient bone volume for full-arch prostheses.
Delivery Systems for BMPs
The effectiveness of Bone Morphogenetic Proteins depends on their delivery system, which ensures sustained release, optimal localization, and biological activity.
- Collagen-Based Carriers
- Synthetic Scaffolds
- Injectable Hydrogels
- 3D-Printed Scaffolds
Collagen-Based Carriers
Absorbable collagen sponges (ACS) are the most commonly used carriers for BMP delivery. They provide a scaffold for cell attachment and maintain Bone Morphogenetic Proteins bioactivity.
- Example – INFUSE Bone Graft (Medtronic), which combines BMP-2 with an ACS carrier.
Synthetic Scaffolds
Hydroxyapatite, beta-tricalcium phosphate (β-TCP), and polycaprolactone (PCL) are synthetic materials used to deliver BMPs in bone defects.
- Advantages – Controlled degradation and osteoconductive properties.
Injectable Hydrogels
Hydrogels loaded with Bone Morphogenetic Proteins offer a minimally invasive option for periodontal and peri-implant regeneration.
- Future Prospects – Smart hydrogels with controlled release mechanisms are under development.
3D-Printed Scaffolds
Advances in 3D printing have enabled the fabrication of patient-specific scaffolds loaded with BMPs for defect reconstruction.
- Example – 3D-printed titanium or polymer scaffolds infused with BMP-2.
Challenges and Limitations
Despite their promise, Bone Morphogenetic Proteins face several challenges in clinical application:
- High Cost – The production and delivery of recombinant BMPs are expensive, limiting their widespread use.
- Overdose Complications – Excessive Bone Morphogenetic Proteins doses can lead to ectopic bone formation, inflammation, and other complications.
- Regulatory Approvals – Strict regulatory requirements and limited indications restrict BMP use in certain regions.
- Host Response Variability – Patient-specific factors, such as age, systemic health, and smoking, can influence Bone Morphogenetic Proteins efficacy.
Future Directions and Research
- Genetic Engineering
- Nanotechnology
- Combinatorial Therapies
- Tissue Engineering
Genetic Engineering
Advances in gene therapy aim to enhance Bone Morphogenetic Proteins production within target tissues by transfecting cells with BMP-encoding genes. This approach offers sustained BMP availability without exogenous delivery.
Nanotechnology
Nanoparticles are being explored as carriers for BMP delivery, allowing controlled release and increased bioavailability.
- Example – BMP-loaded silica nanoparticles for localized bone regeneration.
Combinatorial Therapies
Combining Bone Morphogenetic Proteins with other growth factors, such as vascular endothelial growth factor (VEGF), may enhance angiogenesis and bone healing.
- Clinical Potential – Synergistic effects between BMPs and VEGF could improve outcomes in large defects.
Tissue Engineering
The integration of Bone Morphogenetic Proteins with stem cells and biomimetic scaffolds represents a promising avenue for customized tissue engineering solutions.
- Example – Autologous mesenchymal stem cells seeded on BMP-loaded scaffolds for complex bone defects.
Frequently Asked Questions (FAQs)
What are Bone Morphogenetic Proteins (BMPs)?
BMPs are a group of growth factors that belong to the transforming growth factor-beta (TGF-β) superfamily. They play a crucial role in bone formation, regeneration, and repair by stimulating the differentiation of mesenchymal stem cells into osteoblasts, the cells responsible for bone production.
How are BMPs used in dentistry?
BMPs are primarily used in dentistry for:
- Periodontal regeneration to restore lost bone and support structures of teeth.
- Alveolar ridge augmentation to increase bone volume for dental implants.
- Sinus floor elevation in cases of maxillary atrophy.
- Management of peri-implant bone defects.
- Maxillofacial reconstruction after trauma, tumor removal, or congenital defects.
What are the most commonly used BMPs in dental applications?
The most commonly used BMPs in dental and implant applications are:
- BMP-2: Strongly osteoinductive and widely used for bone regeneration.
- BMP-7 (Osteogenic Protein-1, OP-1): Used in bone grafting and maxillofacial reconstruction.
How do BMPs enhance dental implant success?
BMPs improve dental implant outcomes by:
- Promoting faster and stronger osseointegration.
- Enhancing bone regeneration in deficient areas before or during implant placement.
- Reducing the need for autogenous bone grafts, which require secondary donor sites.
- Improving implant stability in compromised bone conditions.
Are BMPs safe for use in dentistry?
Yes, BMPs have been extensively studied and are approved by regulatory agencies such as the U.S. Food and Drug Administration (FDA) for specific dental and orthopedic applications. However, their use should be carefully controlled to avoid potential complications such as ectopic bone formation, excessive inflammation, and unpredictable host responses.
What are the potential side effects of BMP use in dental procedures?
While BMPs are highly effective, they may lead to:
- Inflammation and swelling at the application site.
- Ectopic bone formation if the BMP diffuses beyond the targeted area.
- High costs, making treatment less accessible to some patients.
- Overstimulation of bone growth, which can cause irregular bone formations if not properly controlled.
How are BMPs delivered to the surgical site?
BMPs require a suitable carrier for effective application. The most common delivery systems include:
- Absorbable collagen sponges (ACS) – Used as a scaffold for BMP delivery.
- Synthetic scaffolds (hydroxyapatite, β-tricalcium phosphate) – Provide osteoconductive support.
- Injectable hydrogels – Allow for minimally invasive applications.
- 3D-printed scaffolds – Custom-designed scaffolds infused with BMPs for complex bone defects.
Are BMPs a substitute for traditional bone grafts?
In many cases, BMPs can serve as an alternative to autogenous bone grafts, reducing the need for secondary surgical sites and minimizing donor site morbidity. However, in large bone defects, BMPs are often used in combination with bone grafts for enhanced outcomes.
How long does it take for BMP-induced bone formation?
The timeline for BMP-induced bone formation varies but generally takes:
- 4-6 weeks for initial bone formation.
- 3-6 months for sufficient bone maturation before dental implant placement.
Can BMPs be used in patients with severe bone loss?
Yes, BMPs are particularly useful for patients with severe bone loss due to periodontal disease, trauma, or atrophy. They can stimulate new bone formation, making implant placement feasible even in challenging cases.
Are BMPs suitable for everyone?
BMPs are generally safe but may not be suitable for:
- Patients with a history of cancer, as BMPs can stimulate cellular activity.
- Individuals with autoimmune diseases or severe systemic conditions that impair healing.
- Cases where excessive bone growth could pose a risk, such as in certain craniofacial syndromes.
How do BMPs compare to platelet-rich plasma (PRP) in bone regeneration?
BMPs are more potent than PRP in bone induction. PRP enhances healing by providing growth factors derived from the patient’s own blood, but it does not directly stimulate new bone formation as BMPs do.
What is the cost of BMP treatment in dentistry?
The cost varies depending on the procedure, BMP dosage, and carrier material. BMP-based treatments are generally more expensive than traditional grafting methods due to the high cost of recombinant proteins.
Can BMPs be used in peri-implantitis treatment?
Yes, BMPs, particularly BMP-2, are used in peri-implantitis cases to regenerate lost bone around failing implants. They help restore bone density and improve implant stability.
What is the future of BMPs in dentistry?
The future of BMPs in dentistry includes:
- Genetic engineering for in-situ BMP production.
- Nanotechnology-based carriers for controlled BMP release.
- Combination therapies with other growth factors (e.g., VEGF) for enhanced regeneration.
- Tissue engineering using stem cells and BMPs for complete dental and craniofacial reconstruction.
Conclusion
Bone Morphogenetic Proteins have transformed the landscape of dentistry and implantology by offering predictable, biologically-driven solutions for bone regeneration and implant integration. From periodontal regeneration to complex maxillofacial reconstructions, BMPs have demonstrated their efficacy and versatility. However, challenges such as cost, regulatory hurdles, and dose related complications highlight the need for ongoing research. Future advancements in delivery systems, genetic engineering, and tissue engineering hold the potential to overcome these barriers, ensuring broader access to BMP-based therapies. As the field evolves, BMPs are poised to remain at the forefront of regenerative dentistry, offering hope and improved quality of life for patients with challenging oral conditions.