Bone density is a critical factor in various medical fields, especially in dentistry. In dentistry, bone density is one of the key elements that determine the success and longevity of dental treatments, particularly dental implants, periodontal therapies, and restorative procedures. This article delves into the concept of bone density, its role in dental implants, its relevance in periodontology, and its broader importance in general dentistry, while discussing the ways to assess and manage bone density-related challenges in dental practice.
Table of Contents
ToggleUnderstanding Bone Density
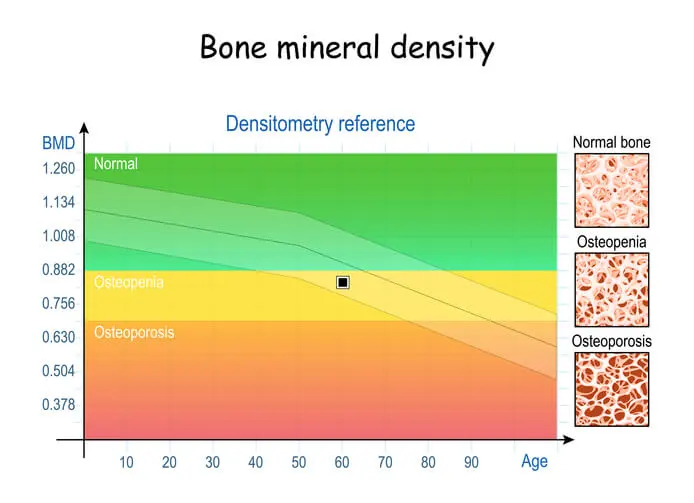
Bone density refers to the amount of bone mineral in bone tissue and is a critical indicator of bone strength. It is measured in terms of grams of mineral per square centimeter of bone and plays a key role in determining the bone’s mechanical properties, including its ability to withstand pressure, stress, and healing potential. Bone density is typically assessed through imaging techniques like dual-energy X-ray absorptiometry (DXA or DEXA scans) and cone-beam computed tomography (CBCT).
Bone density varies throughout the body and between individuals based on factors such as age, gender, genetics, hormonal levels, physical activity, nutrition, and systemic health conditions like osteoporosis or diabetes. In the oral and maxillofacial region, particularly in the alveolar bone (the part of the jawbone that supports teeth), bone density can differ significantly across different areas of the mouth. For example, the posterior maxilla generally has lower bone density compared to the anterior mandible, a factor that can influence the success rate of various dental procedures, particularly dental implants.
Types of Bone Density in the Oral Cavity
Bone in the oral cavity is categorized based on the Lekholm and Zarb classification, which divides bone into four types based on its density:
- Type I – This is dense cortical bone. It is very strong, has high mineral content, and is the most favorable for implant placement. However, it can be relatively less vascular, which may impact healing in some cases.
- Type II – This is a mix of dense cortical bone and a core of less dense trabecular (spongy) bone. It provides good primary stability for dental implants and allows for better healing due to its vascularity.
- Type III – This is a thinner cortical bone with a larger amount of trabecular bone, usually seen in the maxilla. The lower density makes it more challenging for implant placement, but with proper management, it can still yield good results.
- Type IV – This is predominantly trabecular bone with a thin or absent cortical bone. It is the least favorable for dental implant placement due to its low strength and limited ability to provide primary implant stability.
These variations in bone density are crucial for dental professionals to understand and manage because they directly influence the success of procedures like dental implants and periodontal surgeries.
The Role of Bone Density in Dental Implants
- Implant Osseointegration
- Implant Placement and Stability
- Bone Grafting and Bone Augmentation
- Implant Survival Rates
Implant Osseointegration
Dental implants rely heavily on a process called osseointegration, where the implant fuses with the surrounding bone. Successful osseointegration is dependent on the quantity and quality of the bone present, which is directly tied to bone density. High bone density provides the necessary stability and support for implants during both the healing phase and long-term functionality. Implants placed in denser bone (such as Type I and Type II) have a higher chance of achieving primary stability — the initial mechanical engagement between the implant and the bone — which is a key factor in successful osseointegration.
In contrast, low bone density (Types III and IV), such as that found in the posterior maxilla, poses challenges for achieving primary stability. This can lead to micro-movement of the implant during the healing process, which may result in implant failure. To compensate, implantologists may use techniques like undersized drilling (to create a tighter fit for the implant), bone grafting (to augment the available bone), or shorter, wider implants to improve the likelihood of success in areas with lower bone density.
Implant Placement and Stability
The success of dental implants is heavily dependent on the stability achieved at the time of placement, referred to as primary stability. Bone density is one of the most critical factors that affect primary stability. Denser bone offers more resistance to implant placement, providing a more stable foundation. On the other hand, softer, less dense bone may result in inadequate stability and increase the risk of micromovement, which can hinder osseointegration and lead to implant failure.
Primary stability is particularly crucial during the early healing phase, as the implant relies on mechanical stability before biological osseointegration occurs. Implants in denser bone tend to integrate more rapidly and predictably, reducing the risk of early failure.
Bone Grafting and Bone Augmentation
In cases where bone density is insufficient to support an implant, bone grafting or bone augmentation may be necessary to build up the bone volume and improve density. This is often required in areas like the posterior maxilla, where bone tends to be thinner and less dense due to natural resorption after tooth loss or as a result of chronic periodontal disease.
Bone grafting involves the placement of bone graft materials — either autografts (bone from the patient), allografts (bone from a donor), or synthetic bone substitutes — to augment the existing bone and encourage the formation of new, dense bone. Over time, the graft material is resorbed and replaced by the patient’s natural bone, providing a stronger foundation for implant placement.
In the context of bone density, the success of bone grafting procedures depends on several factors, including the quality of the surrounding bone, the blood supply to the area, and the patient’s overall health. Successful bone grafting can significantly improve bone density, making previously unsuitable areas viable for implant placement.
Implant Survival Rates
Multiple studies have shown that implant survival rates are closely linked to bone density. Implants placed in higher-density bone have significantly higher long-term survival rates compared to those placed in low-density bone. This is particularly true in the posterior maxilla, where bone density is naturally lower. In these cases, implant failure rates are higher, particularly if additional measures like bone grafting or sinus lifting are not performed.
Factors like the quality of the bone at the implant site, the type of implant used, the surgical technique, and the patient’s overall health all play a role in the long-term success of dental implants. However, bone density remains one of the most important determinants of implant success, highlighting the need for careful preoperative planning and evaluation.
The Role of Bone Density in Periodontology
- Bone Loss and Periodontal Disease
- Bone Regeneration in Periodontal Therapy
Bone Loss and Periodontal Disease
Periodontal disease, particularly in its advanced stages, leads to the destruction of both soft and hard tissues, including the alveolar bone that supports the teeth. As periodontitis progresses, bone resorption occurs, reducing bone density and eventually leading to tooth mobility and tooth loss if left untreated. The relationship between periodontal disease and bone density is complex, as systemic factors like osteoporosis and diabetes can exacerbate the condition.
In patients with low bone density due to systemic diseases or age-related bone loss, periodontal disease can progress more rapidly and may be more difficult to manage. In such cases, regenerative procedures like bone grafting, guided tissue regeneration (GTR), and the use of growth factors may be employed to restore lost bone and improve density.
Bone Regeneration in Periodontal Therapy
Bone density is a critical consideration in periodontal regeneration, where the goal is to rebuild the bone that has been lost due to disease. Procedures such as bone grafting, guided tissue regeneration (GTR), and the use of biologic agents (e.g., enamel matrix derivatives or platelet-rich plasma) are used to encourage bone growth and increase bone density around affected teeth.
In cases of severe bone loss, bone grafting can help regenerate the lost bone and restore both function and aesthetics. The success of these procedures, however, depends on several factors, including the patient’s bone density, the health of the surrounding tissues, and the presence of adequate blood supply. Improving bone density through these regenerative procedures can significantly improve the prognosis for teeth affected by periodontal disease.
Assessing Bone Density in Dentistry
Accurate assessment of bone density is essential for successful treatment planning in implant dentistry and periodontal therapy.
Imaging Techniques
Several imaging techniques are available to evaluate bone density in the oral cavity:
- Cone-Beam Computed Tomography (CBCT)
- DEXA Scan
- Panoramic Radiographs
Cone-Beam Computed Tomography (CBCT)
CBCT is a three-dimensional imaging technique that provides detailed information about the bone’s structure, including its density and volume. This is the most commonly used imaging modality in implant dentistry and periodontology for assessing bone quality and determining the best course of treatment.
DEXA Scan
While DEXA scans are more commonly used in medical settings to diagnose conditions like osteoporosis, they can also provide valuable information about systemic bone density, which can impact oral bone health.
Panoramic Radiographs
Panoramic X-rays can provide a broad view of the maxilla and mandible but are less detailed than CBCT. They are often used as an initial diagnostic tool, particularly for evaluating bone levels in periodontal disease.
Clinical Evaluation
In addition to imaging, a thorough clinical evaluation is necessary to assess bone density in dental patients. Dentists may palpate the area to evaluate bone thickness, check for signs of bone loss or infection, and assess the patient’s medical history for factors that could impact bone density, such as osteoporosis, medications (e.g., bisphosphonates), or previous trauma.
Bone Density and General Dentistry
In broader dentistry, bone density is relevant in procedures that involve the jawbone’s response to stress and healing. These include:
Orthodontics
Bone density affects tooth movement. Softer, less dense bone allows for quicker movement of teeth, while denser bone may resist movement. For patients with low bone density, orthodontists may need to adjust treatment plans to account for slower tooth movement or increased susceptibility to bone resorption during treatment.
Prosthetics
Bone density also plays a significant role in the placement and success of dental prosthetics, such as bridges or dentures. When teeth are lost, the surrounding bone can atrophy due to lack of stimulation, reducing the bone density in that area. This can make it challenging to fit traditional prosthetics like dentures, which rely on a stable bone foundation for retention and comfort. In cases where bone density is low, dental implants may be preferred to provide a more stable base for prosthetic teeth.
Tooth Extractions
Bone density impacts the healing process after tooth extractions. Patients with higher bone density typically experience faster and more predictable healing, while those with lower bone density may require additional procedures, such as socket preservation techniques, to maintain bone volume for future restorative options like implants.
Factors Influencing Bone Density in Dentistry
Bone density in the jaw can be influenced by various factors, including:
- Age
- Systemic Diseases
- Medications
- Smoking
- Nutrition
- Physical Activity
Age
Bone density naturally decreases with age, which can complicate dental procedures, especially in elderly patients. Post-menopausal women, in particular, experience a significant decline in bone density due to hormonal changes, which can affect both systemic and oral bone health.
Systemic Diseases
Conditions like osteoporosis, diabetes, and rheumatoid arthritis can negatively impact bone density in the jaw. Osteoporosis, for example, leads to decreased bone mineral content, which can complicate implant placement and increase the risk of periodontal disease. Diabetes, especially when poorly controlled, can lead to impaired bone metabolism and healing, making bone density management more challenging in these patients.
Medications
Certain medications, particularly bisphosphonates used to treat osteoporosis, can affect bone turnover and healing. Patients on long-term bisphosphonate therapy are at risk for a condition called bisphosphonate-related osteonecrosis of the jaw (BRONJ), where bone fails to heal properly after invasive dental procedures. This highlights the importance of evaluating bone density and understanding a patient’s medical history before any surgical interventions in dentistry.
Smoking
Smoking is a well-known risk factor for bone loss and reduced bone density. Nicotine and other chemicals in tobacco can impair blood flow, bone metabolism, and healing, leading to lower bone density in the jaw. Smokers are at a higher risk of periodontal disease and implant failure, underscoring the importance of counseling patients about smoking cessation before undergoing dental procedures.
Nutrition
Adequate calcium and vitamin D intake are essential for maintaining healthy bone density. Nutritional deficiencies can lead to reduced bone mineral content, making dental treatments more complicated. Patients with poor nutrition may require dietary counseling or supplementation to improve bone health and optimize treatment outcomes in dentistry.
Physical Activity
Weight-bearing exercises are known to stimulate bone formation and increase bone density. For patients undergoing long-term dental treatments like implants or periodontal therapy, maintaining a healthy lifestyle that includes regular physical activity can positively impact bone health in the oral cavity.
Management of Bone Density in Dental Practice
Given the importance of bone density in the success of dental treatments, managing bone health is a critical component of dental care. Dental professionals must assess bone density in their patients and consider strategies to enhance or preserve bone when necessary.
Preoperative Planning
Preoperative planning is essential to ensure the success of dental treatments in patients with low bone density. In cases where bone quality is questionable, additional diagnostic tools, such as CBCT, may be employed to get a detailed view of the bone structure. Surgeons must carefully evaluate the patient’s overall health, history of systemic conditions, and medications to develop a personalized treatment plan.
Bone Grafting and Augmentation
For patients with insufficient bone density, bone grafting and augmentation procedures are often required before implant placement. Grafting materials can stimulate new bone growth, enhancing the density and quality of the bone at the implant site. These procedures may also be necessary in periodontal treatments where significant bone loss has occurred due to disease.
Bone grafts can be classified into several categories:
- Autografts
- Allografts
- Xenografts
- Alloplasts
Autografts
These involve taking bone from the patient’s own body, often from areas like the chin or the posterior region of the jaw. Autografts are the gold standard due to their biocompatibility and ability to stimulate new bone formation.
Allografts
These are harvested from a donor, typically cadaveric bone, and processed to ensure safety and compatibility. Allografts are commonly used in cases where autografts are not feasible or the patient prefers a less invasive approach.
Xenografts
These involve bone materials from other species, most commonly bovine bone. Xenografts act as a scaffold for new bone formation and are resorbed over time as the patient’s natural bone replaces the graft.
Alloplasts
These are synthetic bone graft materials made from bioactive substances like calcium phosphate or hydroxyapatite. Alloplasts are useful in patients who prefer not to use animal or donor-derived grafts.
Improving Bone Density Through Lifestyle Modifications
For patients with systemic conditions affecting bone density, lifestyle modifications can improve oral and overall bone health. Encouraging patients to adopt a diet rich in calcium and vitamin D, engage in regular exercise, and avoid harmful habits like smoking can significantly impact the outcome of dental treatments.
Immediate vs. Delayed Implant Placement
In cases where bone density is insufficient, clinicians may opt for delayed implant placement following a bone grafting procedure to allow time for the bone to mature and increase in density. This approach can improve the long-term prognosis of the implant. However, in cases where bone density is adequate, immediate implant placement following tooth extraction may be viable, reducing overall treatment time.
Use of Modern Technology and Techniques
Advances in technology, such as computer-guided implant surgery, have improved the precision of dental procedures in patients with compromised bone density. Using detailed 3D imaging, clinicians can plan the ideal implant placement angle, depth, and orientation, minimizing the risk of complications in low-density bone areas.
In addition, innovations like short and wide-diameter implants, which provide increased surface area for osseointegration, have expanded treatment options for patients with reduced bone density.
Use of Biologic Agents
In recent years, the use of biologic agents, such as platelet-rich plasma (PRP) and enamel matrix derivatives (EMD), has gained popularity in dental treatments aimed at enhancing bone density and promoting tissue regeneration. These agents can accelerate healing, stimulate bone growth, and improve the outcome of procedures like bone grafting and implant placement.
Frequently Asked Questions (FAQs)
What is the role of bone density in dental implants?
Bone density is crucial because it provides the necessary support for dental implants. High-quality, dense bone promotes effective osseointegration—the process by which the implant fuses with the bone—ensuring stability and long-term success.
What happens if you don’t have enough bone for dental implants?
Insufficient bone can compromise implant stability and integration. When the bone volume or density is low, additional procedures like bone grafting or sinus lifts may be recommended to rebuild the bone before implant placement.
How much bone density is needed for dental implants?
The specific amount of bone density required varies based on the implant’s location and individual patient factors. Dentists use imaging techniques (such as CT scans or CBCT) to assess bone quality and quantity, ensuring there’s enough healthy bone to support the implant securely.
Does the implant affect bone density?
Yes, a well-integrated implant can help maintain or even improve local bone density. By transmitting normal chewing forces, the implant stimulates the bone, which can help preserve its structure. However, if the implant does not integrate properly, it may lead to bone loss.
How do they check bone density for dental implants?
Bone density is typically evaluated using imaging methods like Cone Beam Computed Tomography (CBCT), which offers a detailed three-dimensional view of the jawbone. In some cases, other imaging modalities or bone density tests may be used to ensure accurate assessment for implant planning.
What is the connection between bone and implant?
The success of a dental implant relies on osseointegration—the process where the bone grows around and bonds with the implant surface. This strong connection stabilizes the implant, ensuring that it functions effectively as a replacement for a natural tooth.
Conclusion
Bone density is a critical factor that influences the success of a wide range of dental treatments, including dental implants, periodontal therapy, and prosthetic rehabilitation. Understanding the role of bone density in the oral cavity and its impact on treatment outcomes allows dental professionals to plan effectively and manage potential challenges. By utilizing advanced diagnostic tools, modern surgical techniques, and biologic materials, dentists can improve bone health, optimize treatment success, and enhance patient outcomes.
Ultimately, bone density must be carefully evaluated and managed throughout dental treatment planning to ensure that patients receive the best possible care and long-term results. As research in bone biology and regenerative dentistry continues to evolve, clinicians will have more tools and strategies to address bone density challenges and provide better outcomes for their patients.