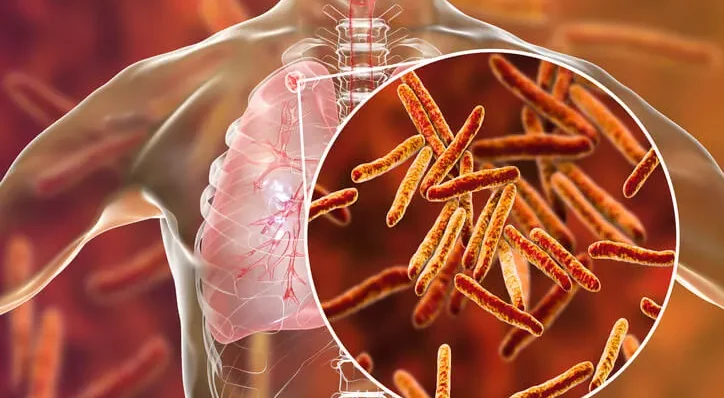
Tuberculosis (TB) is a highly infectious disease caused by the bacterium Mycobacterium tuberculosis. It primarily affects the lungs but can also affect other parts of the body, such as the kidneys, spine, and brain. TB remains a significant global health concern, particularly in developing countries where access to healthcare and proper treatment is limited. In this article, we will explore the various aspects of tuberculosis, its epidemiology, pathophysiology, diagnosis, treatment, and its importance in the field of dentistry.
Table of Contents
ToggleEpidemiology of Tuberculosis
TB is one of the top 10 causes of death worldwide and the leading cause of death from a single infectious agent, ranking above HIV/AIDS. According to the World Health Organization (WHO), an estimated 10 million people fell ill with TB in 2020, with 1.5 million dying from the disease. TB is prevalent in developing countries with overcrowded living conditions, poor sanitation, and limited access to healthcare. However, it also affects developed countries, particularly in urban areas and among marginalized populations such as homeless individuals and those with compromised immune systems.
Pathophysiology of Tuberculosis
Mycobacterium tuberculosis primarily affects the lungs, where it is transmitted through droplets expelled when an infected person coughs or sneezes. Once inhaled, the bacteria infect the alveolar macrophages and replicate within them, leading to the formation of granulomas, which are the hallmark of TB infection. These granulomas can undergo necrosis, leading to the formation of cavities within the lungs, which further aids in the spread of the bacteria.
Symptoms and Diagnosis
The symptoms of TB vary depending on the stage of the disease and the organs involved. The most common symptoms include persistent cough, chest pain, fatigue, weight loss, fever, and night sweats. However, TB can also affect other organs, leading to a wide range of symptoms. Diagnosis often involves a combination of medical history, physical examination, imaging studies (such as chest X-ray), and laboratory tests (such as sputum smear microscopy, culture, and nucleic acid amplification tests).
Treatment of Tuberculosis
TB treatment typically involves a combination of antibiotics taken over a period of 6 to 9 months. The most commonly used antibiotics include isoniazid, rifampicin, ethambutol, and pyrazinamide. It is essential for patients to complete the full course of treatment to prevent the development of drug-resistant strains of TB. However, drug-resistant TB is becoming an increasing concern, particularly multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB), which are more challenging to treat and require second-line antibiotics.
Importance of Tuberculosis in Dentistry
While TB primarily affects the lungs, it can also manifest in the oral cavity and impact dental practice in several ways. Dentists and dental hygienists are at risk of exposure to TB when treating patients with active pulmonary TB or TB lesions in the oral cavity. TB lesions in the oral cavity typically present as ulcerations, nodules, or granulomas, which may be mistaken for other oral lesions if not properly evaluated. Therefore, it is crucial for dental healthcare providers to be aware of the signs and symptoms of TB and to implement appropriate infection control measures to prevent transmission.
Infection Control in Dental Settings
In dental settings, infection control measures are essential to prevent the transmission of TB and other infectious diseases. These measures include proper hand hygiene, wearing personal protective equipment (such as gloves, masks, and eye protection), maintaining a clean and sterile environment, and implementing respiratory hygiene and cough etiquette practices. Additionally, patients with suspected or confirmed TB should be isolated in a well-ventilated room with negative air pressure to minimize the risk of airborne transmission.
Screening and Referral
Dental healthcare providers should also be involved in screening patients for TB risk factors and symptoms during routine dental visits. Patients with a history of TB, respiratory symptoms suggestive of TB, or known exposure to TB should be referred to a medical professional for further evaluation and management. Furthermore, dental healthcare providers should be familiar with the local TB control guidelines and collaborate with public health authorities to ensure timely diagnosis and treatment of TB cases.
Conclusion
In conclusion, tuberculosis remains a significant global health concern with widespread implications for public health and healthcare delivery. While TB primarily affects the lungs, it can also manifest in the oral cavity and impact dental practice. Dental healthcare providers play a crucial role in preventing the transmission of TB by implementing appropriate infection control measures, screening patients for TB risk factors and symptoms, and referring suspected cases for further evaluation and management. By integrating TB control efforts into dental practice, we can contribute to the global efforts to eliminate TB and improve public health outcomes worldwide.