Tonsils are small, lymphoid tissues located at the back of the throat. Despite their small size, they play a significant role in the immune system, especially during early childhood. Tonsil removal, or tonsillectomy, is a common procedure, yet it’s essential to understand when this surgery is necessary. This article delves into the anatomy and function of the tonsils, common issues associated with them, and the medical guidelines for their removal.
Table of Contents
ToggleAnatomy and Function of Tonsils
Structure of Tonsils
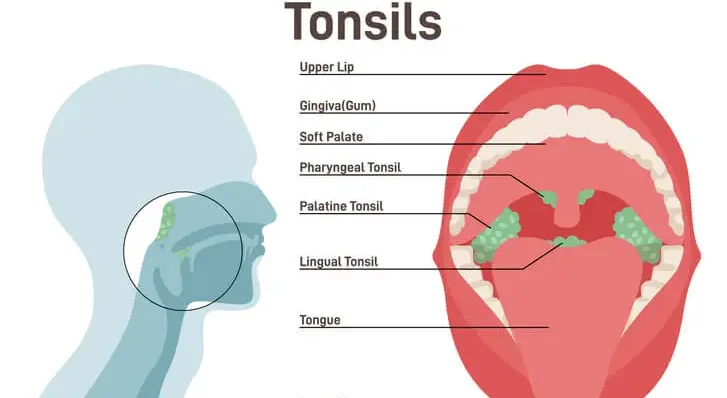
The human body has three sets of tonsils: the palatine, pharyngeal (commonly known as adenoids), and lingual tonsils. The palatine tonsils are the most commonly referred to when discussing tonsil issues and surgeries. These are located on either side of the throat and are visible when the mouth is open wide. The adenoids sit higher in the throat, behind the nose, while the lingual tonsils are found at the base of the tongue.
Function of Tonsils
Tonsils are part of the body’s lymphatic system, which helps fight infections. They act as a first line of defense, trapping pathogens (bacteria and viruses) that enter through the mouth or nose. Tonsils contain cells that produce antibodies to fight off infections, playing a crucial role in the development of the immune system in young children.
Common Tonsil Problems
Despite their protective role, tonsils can become problematic, particularly when they become infected or enlarged.
Tonsillitis
Tonsillitis is an inflammation of the tonsils, typically caused by viral or bacterial infections. Common symptoms include:
- Sore throat
- Difficulty swallowing
- Red and swollen tonsils
- White or yellow coating on the tonsils
- Fever
- Swollen lymph nodes in the neck
Tonsillitis can be acute or chronic. Acute tonsillitis is a short-term condition that often resolves with appropriate treatment. Chronic tonsillitis, however, involves repeated infections and may lead to more severe health issues.
Enlarged Tonsils (Tonsillar Hypertrophy)
Enlarged tonsils, or tonsillar hypertrophy, can occur without infection. This condition is particularly common in children and can lead to obstructive sleep apnea (OSA), a serious disorder characterized by repetitive pauses in breathing during sleep. Symptoms of OSA in children include:
- Loud snoring
- Pauses in breathing
- Restless sleep
- Daytime fatigue or hyperactivity
- Behavioral issues
Peritonsillar Abscess
A peritonsillar abscess is a collection of pus that forms near the tonsils, typically as a complication of tonsillitis. This condition can cause severe throat pain, difficulty swallowing, fever, and swelling that can block the throat, leading to difficulty breathing.
When to Consider Tonsil Removal
Tonsil removal, or tonsillectomy, is considered when tonsil problems become severe and recurrent. The decision to remove the tonsils is based on specific medical guidelines and varies based on individual circumstances.
Recurrent Tonsillitis
One of the primary reasons for tonsillectomy is recurrent tonsillitis. The American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) provides criteria to help determine when a tonsillectomy is appropriate. According to the AAO-HNS, tonsillectomy may be considered if a child has:
- Seven or more episodes of tonsillitis in one year
- Five or more episodes per year for two consecutive years
- Three or more episodes per year for three consecutive years
These episodes should be well-documented, showing specific symptoms such as fever, swollen lymph nodes, and positive cultures for streptococcus (a common cause of bacterial tonsillitis).
Obstructive Sleep Apnea (OSA)
Tonsillectomy is often recommended for children with enlarged tonsils causing obstructive sleep apnea. The decision is typically based on a combination of symptoms and sleep studies that confirm the diagnosis of OSA. Tonsillectomy can significantly improve sleep quality and overall health in these cases.
Peritonsillar Abscess
In cases of peritonsillar abscess, a tonsillectomy might be recommended to prevent recurrent abscesses. This decision is often made after an initial abscess has been treated and the risk of recurrence is deemed high.
Other Indications
Other indications for tonsillectomy include:
- Chronic tonsillitis that does not respond to treatment
- Significant difficulty swallowing or breathing due to enlarged tonsils
- Suspicion of malignancy (cancer) in the tonsils, though this is rare
The Tonsillectomy Procedure
Preoperative Considerations
Before undergoing a tonsillectomy, a thorough medical evaluation is necessary. This includes a detailed medical history, physical examination, and sometimes blood tests or imaging studies. The surgeon will explain the risks and benefits of the procedure and provide instructions on how to prepare for surgery, such as fasting requirements and medication adjustments.
The Surgery
Tonsillectomy is typically performed under general anesthesia. The procedure involves the surgical removal of the tonsils through the mouth, with no external incisions. There are several techniques for tonsil removal, including:
- Cold knife (steel) dissection
- Electrocautery (using electric current)
- Coblation (using radiofrequency energy)
- Harmonic scalpel (using ultrasonic energy)
The choice of technique depends on the surgeon’s preference and the specific case. The surgery usually takes about 30 to 60 minutes.
Postoperative Care
Recovery from tonsillectomy can be uncomfortable and requires careful postoperative care. Common postoperative symptoms include:
- Throat pain
- Difficulty swallowing
- Ear pain (referred pain)
- Mild fever
- Bad breath
Pain management is crucial, and doctors typically prescribe pain relievers. Hydration is essential, and patients are encouraged to drink plenty of fluids. Soft, cool foods such as ice cream, yogurt, and applesauce can help soothe the throat. It is also important to avoid rough or acidic foods that can irritate the surgical site.
Potential Complications
Like any surgery, tonsillectomy carries risks. Potential complications include:
- Bleeding: Postoperative bleeding is a significant risk, especially within the first 24 hours and about 7 to 10 days after surgery when scabs begin to fall off.
- Infection: Although rare, infections can occur at the surgical site.
- Dehydration: Pain and difficulty swallowing can lead to reduced fluid intake and dehydration.
- Adverse reactions to anesthesia: These can include nausea, vomiting, and, in rare cases, more serious reactions.
Most complications can be managed with appropriate medical care, but it is important to follow postoperative instructions carefully and seek medical attention if any concerning symptoms arise.
Frequently Asked Questions (FAQs)
What is the reason for getting tonsils?
Tonsils are a crucial part of the immune system, acting as a defense mechanism against bacteria, viruses, and other harmful pathogens. They are located at the back of the throat and help to filter out germs before they can enter the respiratory or digestive systems. Tonsils also produce white blood cells and antibodies to fight infections, particularly during childhood when the immune system is still developing.
Should tonsils be removed?
Tonsil removal, or tonsillectomy, is generally only recommended in cases of recurring tonsillitis, frequent throat infections, obstructive sleep apnea, or difficulty breathing due to enlarged tonsils. In some cases, persistent bad breath (halitosis) caused by tonsil stones (tonsilloliths) may also be a reason for removal. However, unless there is a medical necessity, most doctors prefer to leave the tonsils intact because they play a role in the body’s immune response.
How do you know you’ve got tonsillitis?
Tonsillitis is characterized by a sore throat, difficulty swallowing, and swollen, inflamed tonsils. Other common symptoms include fever, headache, swollen lymph nodes in the neck, bad breath, and white or yellow patches on the tonsils. In some cases, tonsillitis may also cause ear pain, fatigue, and a muffled voice. If symptoms persist for more than a few days, a doctor should be consulted for diagnosis and treatment.
What is the purpose of your tonsils?
Tonsils act as the body’s first line of defense against infections that enter through the mouth and nose. They help detect and trap harmful bacteria and viruses before they can spread further into the body. Tonsils are particularly important in children, as their immune systems are still developing. Over time, the immune function of the tonsils decreases as the body develops other means of defense, which is why adults can often have them removed with minimal long-term effects.
Why do doctors not want to remove tonsils?
Doctors generally avoid removing tonsils unless necessary because they play an important role in the immune system, particularly during childhood. Tonsil removal can lead to risks such as bleeding, infection, and discomfort during recovery. Additionally, some studies suggest that tonsil removal may slightly increase susceptibility to respiratory infections, allergies, or other illnesses, though the overall impact is usually minimal.
What is the best age to get your tonsils removed?
Tonsillectomy is most commonly performed on children between the ages of 3 and 7, as this is when enlarged or frequently infected tonsils are most problematic. However, the procedure can be performed at any age if medically necessary. In adults, recovery may take longer and be more painful compared to children. Doctors will typically assess the severity of symptoms before recommending surgery.
What is the disadvantage of removing tonsils?
The disadvantages of tonsil removal include potential post-surgical complications such as bleeding, infection, and pain. Recovery can be uncomfortable, with a sore throat lasting up to two weeks. Some research suggests that removing tonsils may slightly reduce the body’s ability to fight upper respiratory infections. Additionally, in rare cases, patients may experience changes in their voice due to the removal of tissue that affects resonance.
Does tonsil removal change your voice?
Tonsil removal can slightly alter voice resonance, particularly in individuals with very large tonsils before surgery. The procedure may change how sound vibrates in the throat, leading to a slight difference in voice tone. However, for most people, any change is subtle and barely noticeable. Professional singers or speakers may detect a minor change, but it is usually not significant enough to affect performance.
Do people without tonsils get sick more?
Most people do not experience an increase in illness after having their tonsils removed. While the tonsils play a role in immune defense, the body has other mechanisms to fight infections, such as lymph nodes and other immune tissues. However, some individuals may experience slightly more upper respiratory infections in the first few months after surgery as the body adjusts.
Do tonsils grow back?
In rare cases, tonsil tissue can regrow if some tissue is left behind during surgery. This is more likely to happen in young children who undergo a partial tonsillectomy. However, even if regrowth occurs, the new tissue is usually much smaller and does not cause the same problems that led to the initial surgery.
How to naturally shrink tonsils?
To naturally reduce the size of swollen tonsils, consider the following remedies:
- Saltwater gargles: Gargling with warm salt water can help reduce inflammation and kill bacteria.
- Staying hydrated: Drinking plenty of fluids, especially warm teas and broths, helps soothe the throat.
- Honey and warm tea: Honey has antibacterial properties and can help reduce swelling and irritation.
- Avoiding irritants: Limiting exposure to smoke, pollution, and allergens can help prevent tonsil inflammation.
- Turmeric and ginger: These natural anti-inflammatory agents can be added to warm drinks to help reduce swelling.
- Humidifiers: Using a humidifier can keep the air moist and reduce throat dryness, which may help shrink swollen tonsils over time. If tonsil swelling is persistent or severe, it is important to consult a doctor for proper diagnosis and treatment.
Conclusion
Tonsils play an important role in the immune system, particularly in children, by helping to protect against infections. However, when tonsils become problematic due to recurrent infections, significant enlargement, or complications like peritonsillar abscesses, a tonsillectomy may be necessary. Understanding the indications for tonsil removal, the procedure itself, and postoperative care can help patients and their families make informed decisions about this common surgery.
Tonsillectomy has been performed for many decades and continues to be a safe and effective solution for various tonsil-related issues. With advancements in surgical techniques and postoperative care, patients can expect a smooth recovery and significant improvement in their quality of life. As always, it is crucial to consult with a healthcare professional to determine the best course of action based on individual medical needs.