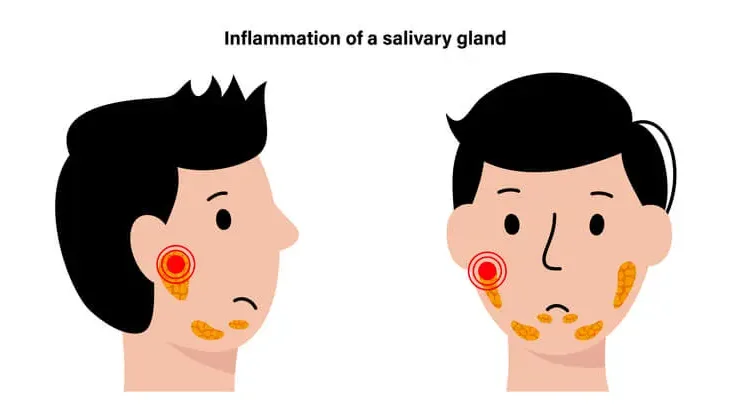
Sialadenitis is a medical condition characterized by the inflammation of the salivary glands. This condition can affect any of the major salivary glands, including the parotid, submandibular, and sublingual glands, as well as minor salivary glands scattered throughout the oral cavity. Sialadenitis can occur due to various factors, including infections, blockages, autoimmune disorders, or systemic diseases. Understanding this condition is crucial for early diagnosis, effective treatment, and prevention of complications. This article explores the etiology, clinical presentation, diagnostic approaches, and treatment options for sialadenitis.
Table of Contents
ToggleAnatomy and Function of Salivary Glands
The salivary glands play an essential role in the oral and digestive systems. They secrete saliva, which aids in digestion, lubricates the oral cavity, protects teeth from decay, and provides antimicrobial action. There are three pairs of major salivary glands:
- Parotid glands: Located near the cheeks and in front of the ears, these are the largest salivary glands.
- Submandibular glands: Found beneath the jaw, these glands produce a mix of serous and mucous saliva.
- Sublingual glands: Located under the tongue, these glands primarily produce mucous saliva.
Minor salivary glands are distributed throughout the mucosa of the oral cavity, contributing to a small but important amount of saliva.
Etiology of Sialadenitis
Sialadenitis can result from various causes:
- Infections
- Obstruction
- Autoimmune Conditions
- Radiation Therapy
- Trauma
- Other Causes
Infections
- Bacterial infections: Acute bacterial sialadenitis often occurs due to bacterial invasion, most commonly by Staphylococcus aureus. Other pathogens include Streptococcus species and Haemophilus influenzae.
- Viral infections: Viral causes include mumps, a viral infection of the parotid gland caused by the paramyxovirus. Other viral agents include cytomegalovirus (CMV) and Epstein-Barr virus (EBV).
Obstruction
- Sialolithiasis: Salivary duct stones can block the flow of saliva, leading to secondary infection and inflammation.
- Strictures: Narrowing of the salivary ducts due to chronic inflammation or trauma can impede saliva flow.
Autoimmune Conditions
- Sjögren’s syndrome: Sjogren’s syndrome A chronic autoimmune disease that causes lymphocytic infiltration of salivary and lacrimal glands, leading to dry mouth (xerostomia) and dry eyes (keratoconjunctivitis sicca).
- Other autoimmune disorders: Conditions such as systemic lupus erythematosus (SLE) and rheumatoid arthritis can also involve the salivary glands.
Radiation Therapy
Radiation therapy for head and neck cancers can damage salivary glands, causing inflammation, fibrosis, and reduced saliva production.
Trauma
Physical trauma or surgical interventions near the salivary glands can trigger sialadenitis.
Other Causes
Dehydration, malnutrition, or systemic illnesses can predispose individuals to sialadenitis by reducing saliva production or altering its composition.
Clinical Presentation
The symptoms of sialadenitis vary depending on the cause and severity of the condition. Common symptoms include:
- Pain and Swelling: Pain and swelling are the hallmark symptoms, often localized to the affected gland. Swelling may worsen during meals due to increased saliva production.
- Erythema and Tenderness: The overlying skin may appear red and feel warm to the touch. The gland is tender on palpation.
- Fever and Malaise: Systemic signs such as fever, chills, and fatigue are common in acute bacterial sialadenitis.
- Xerostomia: Dry mouth may occur due to reduced saliva production.
- Purulent Discharge: In bacterial infections, pus may drain from the duct opening into the oral cavity.
- Difficulty Eating and Speaking: Swelling and pain can interfere with mastication and articulation.
- Recurrent Symptoms: Chronic sialadenitis may present with recurrent episodes of pain and swelling.
Diagnosis
The diagnosis of sialadenitis involves a combination of clinical evaluation, imaging, and laboratory studies.
1. History and Physical Examination
- A detailed history of symptoms, medical conditions, and risk factors is essential.
- Physical examination includes palpation of the salivary glands and inspection of the duct openings for discharge or blockage.
2. Imaging Studies
- Ultrasound: A non-invasive modality to assess glandular swelling, ductal dilatation, or stones.
- CT Scan: Useful for detecting abscesses, stones, or tumors.
- MRI: Provides detailed imaging of soft tissues and is helpful in assessing chronic or complex cases.
- Sialography: Involves injecting contrast into the ductal system to evaluate blockages or strictures.
3. Laboratory Tests
- Microbiological cultures: Analysis of pus or saliva can identify causative pathogens.
- Autoimmune markers: Tests for antibodies such as anti-SSA/Ro and anti-SSB/La in suspected Sjögren’s syndrome.
- Complete blood count (CBC): May reveal leukocytosis in bacterial infections.
4. Biopsy
In chronic or unclear cases, a biopsy of the gland may be performed to rule out neoplasms or confirm autoimmune diseases.
Treatment of Sialadenitis
The treatment of sialadenitis depends on the underlying cause and severity of the condition.
1. Medical Management
Bacterial Infections:
- Empiric antibiotic therapy targeting common pathogens, such as amoxicillin-clavulanate or clindamycin.
- Adjust antibiotics based on culture and sensitivity results.
Viral Infections:
- Supportive care, including hydration, analgesics, and antipyretics, as antibiotics are ineffective against viruses.
Autoimmune Conditions:
- Immunosuppressive medications such as corticosteroids or disease modifying antirheumatic drugs (DMARDs) in autoimmune sialadenitis.
- Artificial saliva and pilocarpine may alleviate xerostomia.
2. Surgical Intervention
Drainage of Abscesses:
Incision and drainage are necessary for abscess formation.
Advertisements
Removal of Stones or Tumors:
- Sialolithiasis may require endoscopic or surgical removal of stones.
- Tumors necessitate excision, often with gland removal.
Ductal Repair:
For strictures or trauma-induced blockages, ductal repair or dilation may restore salivary flow.
3. Supportive Measures
- Hydration to maintain salivary flow.
- Warm compresses and gentle massage of the gland to promote drainage.
- Sialogogues (substances that stimulate saliva production), such as lemon drops or chewing gum.
4. Management of Chronic Sialadenitis
Recurrent or chronic sialadenitis may require long-term management, including addressing underlying causes, regular monitoring, and surgical intervention when necessary.
Complications
If untreated, sialadenitis can lead to:
- Abscess Formation: Localized pus accumulation requiring surgical drainage.
- Chronic Sialadenitis: Persistent inflammation can result in fibrosis and gland dysfunction.
- Spread of Infection: Untreated bacterial sialadenitis may progress to cellulitis or sepsis.
- Salivary Gland Dysfunction: Chronic inflammation or obstruction can permanently impair saliva production.
- Neoplasms: Persistent swelling and pain should raise suspicion of salivary gland tumors.
Prevention
Preventing sialadenitis involves addressing risk factors and maintaining good oral and systemic health:
- Hydration: Adequate fluid intake prevents dehydration and ensures normal salivary flow.
- Oral Hygiene: Regular brushing, flossing, and dental check-ups reduce the risk of infections.
- Avoidance of Irritants: Limiting alcohol and tobacco use can reduce gland irritation.
- Early Treatment of Obstructions: Prompt management of sialolithiasis or ductal strictures prevents secondary infections.
- Monitoring Autoimmune Conditions: Regular follow-ups for individuals with Sjögren’s syndrome or other autoimmune diseases.
Frequently Asked Questions
1. Is sialadenitis contagious?
Bacterial sialadenitis is not contagious, but viral infections like mumps can be spread through respiratory droplets.
2. Can sialadenitis go away on its own?
Mild cases may resolve with hydration and supportive care, but bacterial infections often require antibiotics.
3. How can I prevent sialadenitis?
Maintaining good oral hygiene, staying hydrated, and treating any underlying conditions can help prevent sialadenitis.
4. When should I see a doctor for sialadenitis?
Seek medical attention if symptoms persist for more than a few days, worsen, or include fever and pus discharge.
5. Can sialadenitis recur?
Yes, especially in cases of chronic conditions or unresolved obstructions.
Conclusion
Sialadenitis is a potentially debilitating condition that can significantly affect the quality of life if left untreated. A comprehensive understanding of its causes, symptoms, and treatment options is essential for effective management. Advances in diagnostic tools and minimally invasive treatments have greatly improved outcomes for patients with sialadenitis. Early diagnosis and prompt intervention, combined with preventive measures, can help mitigate complications and ensure better long-term health for affected individuals.