Rheumatoid arthritis (RA) is a chronic systemic inflammatory disease primarily affecting the synovial joints, leading to pain, swelling, stiffness, and progressive joint destruction. It is an autoimmune disorder that disproportionately affects women and typically presents between the ages of 30 and 50. While RA is commonly known for its impact on joints, particularly the hands and feet, it can also have significant effects on the oral and maxillofacial regions, leading to challenges in dental care.
The relationship between rheumatoid arthritis and oral health is complex, involving both direct effects on the temporomandibular joint (TMJ) and indirect effects on oral hygiene and susceptibility to periodontal disease. Furthermore, the medications used to manage RA may introduce complications for dental treatments. This article aims to explore the multifaceted relationship between rheumatoid arthritis and dentistry, including the clinical implications, management strategies, and best practices for dental professionals when treating patients with RA.
Table of Contents
ToggleRheumatoid Arthritis: Pathophysiology and Systemic Impact
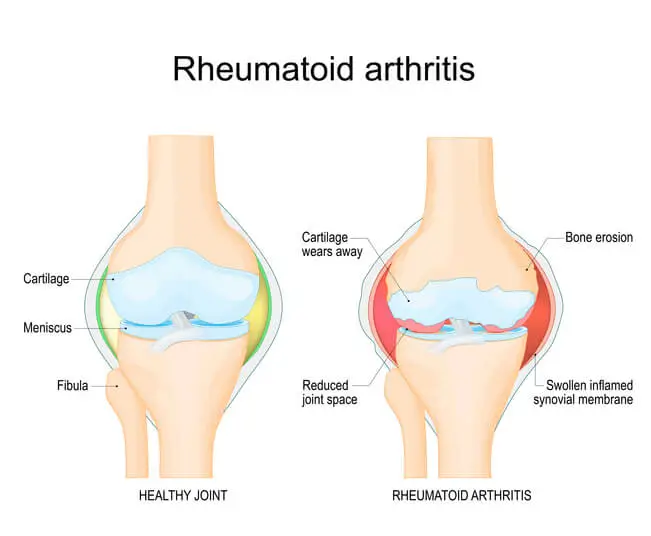
Rheumatoid arthritis is characterized by an autoimmune attack on the synovial membrane, leading to chronic inflammation and joint destruction. The exact cause remains unknown, but genetic, environmental, and hormonal factors are thought to contribute. Autoimmune dysregulation triggers the production of cytokines like tumor necrosis factor-alpha (TNF-α), interleukins, and other inflammatory mediators, which promote tissue damage and erosion of cartilage and bone.
While RA predominantly affects synovial joints, its systemic nature means that various organs and systems, including the oral cavity, can be impacted. Patients with RA often suffer from comorbidities like cardiovascular disease, lung disease, and osteoporosis, which can complicate medical and dental treatment.
Oral Manifestations of Rheumatoid Arthritis
RA can directly and indirectly affect oral health. The following are the primary oral manifestations seen in RA patients:
- Temporomandibular Joint (TMJ) Involvement
- Salivary Gland Dysfunction and Xerostomia
- Periodontal Disease
- Impact of RA Medications on Dental Care
Temporomandibular Joint (TMJ) Involvement
The TMJ is one of the many joints affected by RA. Between 17% and 86% of patients with RA experience TMJ involvement, although the severity varies. The TMJ, a complex joint that allows jaw movement, consists of the mandibular condyle, glenoid fossa, and articular disc. In RA, the inflammatory process in the synovium leads to degeneration of the cartilage and bone, causing pain, limited jaw function, and potential deformities.
Clinical Features of TMJ Involvement in RA are:
- Pain and Tenderness
- Limited Range of Motion
- Crepitus and Clicking Sounds
- Occlusal Changes
- Ankylosis
Pain and Tenderness
Patients often present with chronic pain in the jaw area, which may radiate to the ear and neck. TMJ pain can worsen with chewing or talking.
Limited Range of Motion
RA-induced destruction of the TMJ may cause trismus, a condition where mouth opening is restricted.
Crepitus and Clicking Sounds
As the joint surfaces erode, patients may experience clicking or popping sounds during jaw movement.
Occlusal Changes
Deformities in the TMJ may lead to altered bite patterns, dental malocclusion, and wear on teeth surfaces.
Ankylosis
In severe cases, the joint may become ankylosed, leading to complete immobility of the jaw.
Salivary Gland Dysfunction and Xerostomia
Many RA patients experience xerostomia (dry mouth), either due to RA itself or as a side effect of medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and disease-modifying antirheumatic drugs (DMARDs). Additionally, RA is closely associated with secondary Sjogren’s syndrome, an autoimmune disorder that affects the salivary and lacrimal glands, leading to dry mouth and eyes.
Clinical Implications of Xerostomia are:
- Increased Risk of Dental Caries
- Oral Infections
- Difficulty with Denture Retention
- Altered Taste Sensation
Increased Risk of Dental Caries
Saliva plays a crucial role in buffering acids, clearing food debris, and preventing the growth of harmful bacteria. In xerostomic patients, reduced salivary flow increases the risk of dental caries.
Oral Infections
Dry mouth can lead to oral infections, including candidiasis, due to reduced antimicrobial properties of saliva.
Difficulty with Denture Retention
Denture-wearing RA patients may experience problems with retention and comfort due to dry oral tissues.
Altered Taste Sensation
Xerostomia can also impair the sense of taste, which may affect the patient’s quality of life.
Periodontal Disease
There is a well-established bidirectional relationship between rheumatoid arthritis and periodontal disease. Both conditions share common inflammatory pathways, and periodontal disease is more prevalent and severe in RA patients. Periodontitis is a chronic inflammatory disease of the gums and supporting structures of the teeth, characterized by the destruction of the periodontal ligament and alveolar bone.
Mechanism Linking RA and Periodontal Disease:
Both RA and periodontal disease involve increased levels of inflammatory cytokines like TNF-α, interleukin-6 (IL-6), and prostaglandin E2 (PGE2), which contribute to the breakdown of connective tissue and bone.
- Shared Genetic Susceptibility: Genetic factors, such as polymorphisms in the HLA-DRB1 gene, have been implicated in both RA and periodontal disease.
- Bacterial Infections: The bacterium Porphyromonas gingivalis, which is associated with periodontitis, has been shown to produce enzymes that may play a role in the citrullination of proteins, a key process in the pathogenesis of RA.
Clinical Implications of Periodontal Disease in RA:
- Increased Tooth Loss: RA patients with severe periodontitis may be more prone to tooth loss due to alveolar bone destruction.
- Exacerbation of RA Symptoms: Chronic periodontal infections can potentially worsen RA symptoms by contributing to systemic inflammation.
- Oral Hygiene Challenges: Joint deformities and reduced manual dexterity in RA patients can make it difficult to maintain proper oral hygiene, further increasing the risk of periodontal disease.
Impact of RA Medications on Dental Care
RA is commonly managed with a combination of medications, including NSAIDs, corticosteroids, DMARDs, and biologic agents like TNF-α inhibitors. While these medications can effectively control RA symptoms and slow disease progression, they can also have important implications for dental care.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
- Corticosteroids
- Disease-Modifying Antirheumatic Drugs (DMARDs)
- Biologic Agents
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs are commonly used to relieve pain and inflammation in RA patients. However, they can increase the risk of gastrointestinal bleeding, which may complicate surgical dental procedures. Additionally, long-term NSAID use has been associated with xerostomia and an increased risk of dental caries.
Corticosteroids
Corticosteroids, such as prednisone, are often prescribed for RA to reduce inflammation. However, long-term corticosteroid use can have several oral health implications, including:
- Delayed Wound Healing: Corticosteroids impair the body’s ability to heal, which can be problematic in dental procedures that involve tissue trauma, such as extractions or periodontal surgery.
- Increased Risk of Infection: Corticosteroids suppress the immune system, increasing the risk of oral infections.
- Bone Loss: Prolonged corticosteroid use is associated with osteopenia and osteoporosis, which can affect the alveolar bone and contribute to tooth loss.
Disease-Modifying Antirheumatic Drugs (DMARDs)
DMARDs, such as methotrexate and sulfasalazine, are used to slow the progression of RA. While these drugs are effective in managing the disease, they can cause oral side effects such as:
- Oral Ulcerations: Methotrexate, in particular, can lead to the development of painful oral ulcers, which may affect a patient’s ability to eat and speak.
- Increased Risk of Infection: DMARDs suppress the immune system, making patients more susceptible to oral infections.
Biologic Agents
Biologic agents, such as TNF-α inhibitors (e.g., etanercept and adalimumab), target specific components of the immune system involved in RA. These medications can increase the risk of infections, including periodontal infections, and may affect the success of dental implants due to their impact on bone remodeling.
Dental Management of Patients with Rheumatoid Arthritis
Effective dental management of RA patients requires a multidisciplinary approach that takes into account the patient’s systemic condition, medication use, and oral health needs. The following are key considerations for dental professionals when treating patients with RA:
- Medical History and Communication with the Rheumatologist
- Prevention and Oral Hygiene Maintenance
- Management of TMJ Disorders
- Perioperative Considerations
- Addressing Periodontal Disease
Medical History and Communication with the Rheumatologist
Before initiating dental treatment, it is essential to obtain a comprehensive medical history from the patient, including details about their RA diagnosis, current medications, and any comorbidities. Close communication with the patient’s rheumatologist is critical, especially if surgical procedures are planned or if there are concerns about medication interactions.
Prevention and Oral Hygiene Maintenance
Preventive care is a cornerstone of dental management for RA patients. Given the challenges that RA patients face with manual dexterity, dental professionals should provide tailored oral hygiene instructions and recommend adaptive devices such as electric toothbrushes, floss holders, and interdental brushes.
Saliva Substitutes and Fluoride Treatments
For patients with xerostomia, saliva substitutes and fluoride treatments can help reduce the risk of dental caries and maintain oral health.
Management of TMJ Disorders
For RA patients with TMJ involvement, management options may include:
- Pain Management: NSAIDs and corticosteroids can help alleviate TMJ pain, though care should be taken to minimize long-term side effects.
- Physical Therapy: Jaw exercises and physical therapy may improve jaw function and reduce pain.
- Occlusal Splints: In some cases, occlusal splints may be recommended to alleviate stress on the TMJ and reduce bruxism.
- Surgical Intervention: Severe TMJ destruction may require surgical intervention, including joint replacement or arthroscopy.
Perioperative Considerations
For RA patients undergoing dental surgery, perioperative management is crucial. Corticosteroid use may necessitate supplemental doses to prevent adrenal insufficiency, while DMARDs and biologics may need to be temporarily discontinued to reduce the risk of infection. Additionally, meticulous infection control and postoperative care are essential to minimize complications.
Addressing Periodontal Disease
RA patients should be regularly screened for periodontal disease, and early intervention is key to preventing tooth loss and further systemic complications. Scaling and root planing, along with antimicrobial treatments, may be necessary to control periodontal infections. In severe cases, surgical intervention may be required to restore periodontal health.
Conclusion
Rheumatoid arthritis presents unique challenges in the field of dentistry, with both direct and indirect effects on oral health. From TMJ involvement and xerostomia to an increased risk of periodontal disease, RA can significantly impact a patient’s dental care needs. Medications used to manage RA, such as NSAIDs, corticosteroids, DMARDs, and biologic agents, further complicate dental treatment by introducing risks related to infection, healing, and bone health.
For dental professionals, understanding the systemic nature of RA and its oral manifestations is essential for providing comprehensive care to these patients. By working closely with rheumatologists, employing preventive strategies, and tailoring dental treatments to the individual needs of RA patients, dental practitioners can play a crucial role in maintaining both oral and overall health for individuals living with rheumatoid arthritis.