Platelet-rich plasma (PRP) therapy has emerged as a promising treatment option in various fields of medicine, including orthopedics, dermatology, dentistry, and sports medicine. This innovative approach utilizes the patient’s own blood to promote healing, regeneration, and rejuvenation. The growing interest in PRP therapy is driven by its potential to provide effective, minimally invasive treatments for a range of conditions. This article explores the science behind PRP, its applications, benefits, challenges, and future directions.
Table of Contents
ToggleUnderstanding Platelet-Rich Plasma
PRP is derived from whole blood, which is processed to concentrate platelets in plasma. Platelets are small, disc-shaped cells in the blood that play a crucial role in hemostasis and wound healing. Beyond their clotting capabilities, platelets are reservoirs of growth factors, cytokines, and other bioactive molecules that drive tissue repair and regeneration.
Composition of PRP
- Platelets
- Plasma
- White Blood Cells (WBCs)
Platelets
Platelets are the primary components of PRP and are rich in growth factors such as platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), and transforming growth factor-beta (TGF-β). These growth factors regulate cellular functions like proliferation, differentiation, and angiogenesis.
Plasma
Plasma acts as a carrier for platelets and contains essential proteins, electrolytes, and nutrients that support cellular activities and the healing process.
White Blood Cells (WBCs)
Depending on the preparation method, PRP may include varying levels of white blood cells. These cells contribute to the immune response and can influence inflammation regulation, which plays a role in tissue repair.
Mechanism of Action
PRP works by harnessing the body’s natural healing mechanisms. When injected into injured or damaged tissue, Platelet-rich plasma releases a concentrated dose of growth factors and cytokines that:
- Stimulate Cellular Proliferation and Differentiation: Growth factors in PRP encourage the growth and division of cells, including fibroblasts, chondrocytes, and endothelial cells, which are vital for tissue repair.
- Promote Angiogenesis: The formation of new blood vessels is essential for delivering oxygen and nutrients to damaged tissues, aiding the regeneration process.
- Modulate Inflammation: Platelet-rich plasma helps regulate the inflammatory response, reducing pain and swelling while creating a favorable environment for healing.
- Enhance Extracellular Matrix Formation: PRP stimulates the production of collagen and other matrix components, providing structural integrity and strength to the healing tissue.
Preparation of PRP
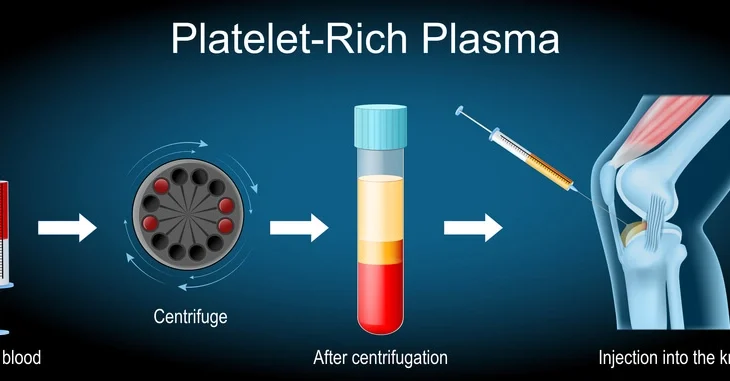
The preparation of PRP typically involves the following steps:
- Blood Collection: A small volume of the patient’s blood (usually 10-20 milliliters) is drawn using standard venipuncture techniques.
- Centrifugation: The blood sample is subjected to centrifugation, which separates it into three distinct layers of blood components: Red blood cells (bottom layer), Platelet-rich plasma (middle layer), Platelet-poor plasma (top layer)
- Extraction: The PRP layer is carefully extracted and prepared for injection. Depending on the intended application, the PRP may be activated using agents such as calcium chloride or thrombin to release growth factors before injection.
Different preparation protocols may be employed based on the desired concentration of platelets and the inclusion or exclusion of leukocytes, tailored to specific therapeutic needs.
Applications of PRP Therapy
PRP therapy’s versatility has made it a valuable tool in multiple medical disciplines. Some of its most common applications include:
- Orthopedics and Sports Medicine
- Dermatology and Aesthetic Medicine
- Wound Healing
- Dentistry
- Ophthalmology
Orthopedics and Sports Medicine
PRP is widely used to treat musculoskeletal injuries, including tendonitis, ligament sprains, and osteoarthritis. For instance, in cases of tennis elbow or rotator cuff injuries, Platelet-rich plasma injections promote tendon repair by stimulating collagen production. In osteoarthritis, PRP has been shown to reduce inflammation and improve joint function by regenerating cartilage.
Dermatology and Aesthetic Medicine
In dermatology, PRP is employed for facial rejuvenation procedures, often referred to as “vampire facials.” By promoting collagen synthesis and enhancing skin elasticity, PRP helps reduce fine lines, wrinkles, and acne scars. In hair restoration, Platelet-rich plasma stimulates dormant hair follicles, making it an effective treatment for androgenic alopecia and other forms of hair loss.
Wound Healing
Chronic wounds, such as diabetic ulcers and pressure sores, often fail to heal due to impaired vascularization and inflammation. PRP accelerates healing by enhancing angiogenesis and reducing inflammation, which restores the wound’s microenvironment.
Dentistry
PRP is used in oral surgery and periodontal treatments to promote bone and soft tissue regeneration. For instance, after tooth extractions or dental implant procedures, Platelet-rich plasma can reduce healing time and improve tissue integration, ensuring better outcomes for patients.
Ophthalmology
PRP-based eye drops are emerging as an innovative treatment for ocular surface disorders, including dry eye syndrome and corneal ulcers. These drops utilize the regenerative properties of Platelet-rich plasma to restore damaged epithelial cells and reduce discomfort.
Benefits of PRP Therapy
The popularity of PRP therapy stems from several key advantages:
- Autologous Nature: Since PRP is derived from the patient’s own blood, it minimizes the risk of allergic reactions, infections, and other adverse effects that are often associated with foreign substances or medications.
- Non-Invasive Procedure: PRP therapy is typically performed as an outpatient procedure. It involves minimal discomfort, short recovery periods, and low risks compared to surgical interventions.
- Versatility: PRP’s ability to address a wide range of medical and aesthetic conditions highlights its adaptability. Whether for repairing damaged tissues, treating chronic conditions, or rejuvenating the skin, PRP offers diverse solutions.
- Enhanced Healing: By delivering concentrated growth factors directly to the affected area, PRP enhances and accelerates the body’s natural healing mechanisms.
Challenges and Limitations
Despite its potential, PRP therapy faces several challenges that need to be addressed:
- Standardization Issues: Variability in PRP preparation methods and platelet concentrations complicates the standardization of treatment protocols. This makes it difficult to compare results across studies and establish clear guidelines for clinical use.
- Limited Evidence Base: While anecdotal evidence and small-scale studies support PRP’s efficacy, larger, well designed clinical trials are needed to validate its benefits conclusively. The lack of robust evidence has led to skepticism in some medical circles.
- Cost: PRP therapy can be expensive, and its use is not always covered by insurance. This limits accessibility for patients who may benefit from the treatment but cannot afford it.
- Variable Outcomes: Patient responses to Platelet-rich plasma therapy can vary based on factors such as age, overall health, the severity of the condition, and individual biological differences. These variables make it challenging to predict treatment success.
Future Directions
Research into PRP therapy continues to expand, with ongoing studies exploring ways to enhance its efficacy and broaden its applications. Promising areas of investigation include:
- Combination Therapies
- Personalized Medicine
- Advanced Preparation Methods
- Expanded Indications
Combination Therapies
Combining PRP with other regenerative techniques, such as stem cell therapy, biomaterials, or advanced drug delivery systems, could amplify its therapeutic effects. For instance, integrating PRP with mesenchymal stem cells may enhance tissue repair and regeneration.
Personalized Medicine
Advances in precision medicine may allow for tailoring PRP formulations to individual patients based on their unique biological profiles. This approach could optimize treatment outcomes and reduce variability in responses.
Advanced Preparation Methods
Innovations in centrifugation and platelet activation techniques could improve the consistency and potency of PRP preparations. These advancements may include automated systems for precise and reproducible formulations.
Expanded Indications
Emerging evidence suggests potential applications of PRP in areas such as neurology (e.g., enhancing neural repair after stroke), cardiology (e.g., myocardial tissue regeneration), and gynecology (e.g., improving uterine and ovarian function).
Ethical and Regulatory Considerations
The use of PRP therapy raises important ethical and regulatory questions. As PRP treatments often fall into a gray area between standard medical practice and experimental therapy, clear guidelines are essential to ensure patient safety and uphold ethical standards. Regulatory agencies must work to balance innovation with the need for rigorous scientific validation. Transparent communication with patients about the experimental nature of some PRP applications is crucial.
Frequently Asked Questions (FAQs)
Is PRP therapy safe?
Yes, PRP therapy is considered safe as it uses the patient’s own blood, reducing the risk of allergic reactions or infections.
How long does it take to see results from PRP therapy?
Results vary depending on the condition being treated. Some patients experience improvement within a few weeks, while others may take a few months.
How many PRP treatments are needed?
The number of sessions varies based on the medical condition. Typically, 2-3 treatments spaced several weeks apart are recommended for optimal results.
Is PRP therapy painful?
The procedure involves injections, which may cause mild discomfort. However, topical anesthetics or numbing agents can help minimize pain.
Are there any side effects of PRP therapy?
Side effects are minimal but may include temporary swelling, redness, or mild pain at the injection site.
Who is a good candidate for PRP therapy?
PRP is suitable for individuals with musculoskeletal injuries, hair loss, skin concerns, and chronic wounds. However, patients with certain blood disorders or active infections may not be ideal candidates.
Is PRP therapy covered by insurance?
PRP treatment is often considered an elective procedure and may not be covered by insurance. It is advisable to check with the insurance provider.
Can PRP be combined with other treatments?
Yes, PRP is often combined with other therapies such as microneedling, stem cell therapy, and physical therapy to enhance results.
Conclusion
Platelet-rich plasma therapy represents a groundbreaking advancement in regenerative medicine, offering hope for patients with chronic conditions, injuries, and aesthetic concerns. While challenges remain in standardizing treatment protocols and establishing a robust evidence base, the potential of PRP is undeniable. With continued research, technological innovation, and regulatory clarity, PRP therapy is poised to play an increasingly important role in modern medicine, revolutionizing the way we approach healing and recovery.