Oral candidiasis, commonly known as oral thrush, is a fungal infection caused by the overgrowth of Candida species, primarily Candida albicans, in the mucous membranes of the mouth. This condition is prevalent across all age groups, from neonates to the elderly, and can range from mild to severe, depending on various factors such as the patient’s immune status, underlying health conditions, and the presence of risk factors. While generally not life-threatening, oral candidiasis can cause significant discomfort, difficulty eating, and, in severe cases, may signal a more serious underlying condition, such as an immune deficiency.
This article provides a detailed exploration of oral candidiasis, including its etiology, pathophysiology, epidemiology, clinical manifestations, diagnosis, treatment, and prevention. Additionally, we will discuss the impact of oral candidiasis on specific populations, such as immunocompromised individuals, and the importance of managing this condition effectively to prevent complications.
Table of Contents
ToggleEtiology and Pathophysiology of Oral Candidiasis
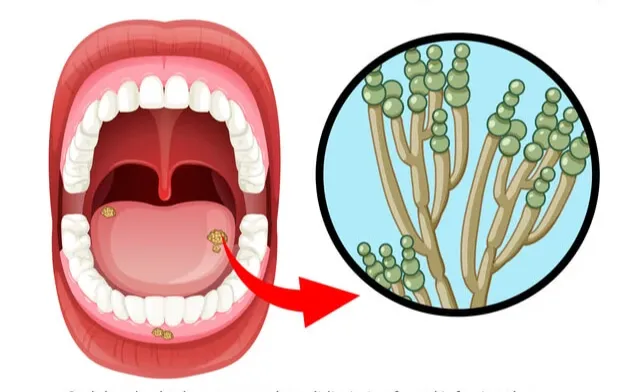
Candida albicans is a dimorphic fungus that exists as a commensal organism in the human body, primarily colonizing the gastrointestinal tract, skin, and mucous membranes. Under normal conditions, the immune system and the natural microbiota of the mouth keep the growth of Candida species in check. However, certain factors can disrupt this balance, leading to the overgrowth of Candida and the development of oral candidiasis.
The pathophysiology of oral candidiasis involves the transition of Candida albicans from its commensal yeast form to its pathogenic hyphal form. This morphological change is associated with the organism’s ability to invade mucosal tissues and evade the host’s immune responses. The hyphal form of Candida produces various virulence factors, such as secreted aspartyl proteases and phospholipases, which facilitate tissue invasion and damage.
Several factors contribute to the development of oral candidiasis, including:
- Immunosuppression
- Antibiotic Use
- Diabetes Mellitus
- Xerostomia (Dry Mouth)
- Poor Oral Hygiene and Denture Use
- Nutritional Deficiencies
Immunosuppression
Individuals with compromised immune systems, such as those with HIV/AIDS, cancer patients undergoing chemotherapy, organ transplant recipients, and those on long-term corticosteroid therapy, are at a higher risk of developing oral candidiasis.
Antibiotic Use
Broad-spectrum antibiotics can disrupt the natural balance of oral microbiota, reducing bacterial competition and allowing for the overgrowth of Candida species.
Diabetes Mellitus
Poorly controlled diabetes mellitus can lead to hyperglycemia, which creates a favorable environment for Candida growth and reduces the effectiveness of immune responses.
Xerostomia (Dry Mouth)
Reduced salivary flow, which can be caused by medications, radiation therapy, or autoimmune conditions like Sjögren’s syndrome, decreases the mechanical clearance of Candida from the oral cavity.
Poor Oral Hygiene and Denture Use
Poor oral hygiene, particularly in denture wearers, can create an environment conducive to Candida overgrowth, particularly under ill-fitting dentures or where food debris accumulates.
Nutritional Deficiencies
Deficiencies in iron, folic acid, or vitamin B12 can impair the immune system’s ability to control Candida growth.
Epidemiology
Oral candidiasis is a common condition, particularly in certain at-risk populations. The prevalence of oral candidiasis varies depending on the population studied, with estimates ranging from 5% to 60% in different groups.
- Infants
- Elderly
- HIV/AIDS Patients
- Cancer Patients
Infants
Oral candidiasis is commonly seen in neonates and infants, where it is often referred to as “thrush.” The prevalence in this age group can be as high as 5% to 7%, due to the immaturity of their immune systems and exposure to Candida during birth or breastfeeding.
Elderly
The elderly population is also at an increased risk, particularly those with dentures, xerostomia, or underlying chronic conditions. The prevalence in this group can be as high as 60%, particularly in institutionalized elderly patients.
HIV/AIDS Patients
Oral candidiasis is one of the most common opportunistic infections in individuals with HIV/AIDS, with a prevalence of up to 90% in untreated or advanced cases. It is often one of the first signs of immune suppression in these patients.
Cancer Patients
Those undergoing chemotherapy or radiation therapy for head and neck cancers are at a high risk of developing oral candidiasis due to mucosal damage and immunosuppression.
Clinical Manifestations of Oral Candidiasis
Oral candidiasis can present in several different forms, each with distinct clinical features. The most common forms include:
- Pseudomembranous Candidiasis (Thrush)
- Erythematous Candidiasis
- Erythematous Candidiasis
- Hyperplastic Candidiasis
- Angular Cheilitis
- Median Rhomboid Glossitis
- Denture Stomatitis
Pseudomembranous Candidiasis (Thrush)
This is the most recognizable form of oral candidiasis, characterized by the presence of white, curd-like plaques on the mucosal surfaces of the mouth, including the tongue, palate, and inner cheeks. These plaques can be wiped away, often leaving behind erythematous or bleeding areas. Patients may experience a burning sensation, discomfort, or a metallic taste in the mouth.
Erythematous Candidiasis
Also known as atrophic candidiasis, this form presents as red, inflamed areas, particularly on the palate, tongue, or the corners of the mouth (angular cheilitis). This type is often associated with denture wearers and can occur after the use of broad-spectrum antibiotics or inhaled corticosteroids. Symptoms may include a burning sensation and soreness.
Hyperplastic Candidiasis
This form is less common and presents as thick, white plaques that cannot be easily scraped off. These lesions are often found on the tongue or the buccal mucosa and may be associated with chronic irritation, such as from ill-fitting dentures.
Angular Cheilitis
This condition presents as erythematous, fissured lesions at the corners of the mouth. It is often associated with a mixed infection of Candida and Staphylococcus aureus and can occur in individuals with poor denture hygiene, nutritional deficiencies, or those with a tendency to drool.
Median Rhomboid Glossitis
This form presents as a well-demarcated, red, rhomboid-shaped lesion on the midline of the dorsal tongue. It is thought to result from chronic Candida infection in combination with other factors, such as smoking or denture use.
Denture Stomatitis
This form of candidiasis occurs in denture wearers, particularly those who do not remove their dentures regularly or who have poor denture hygiene. It presents as generalized erythema of the mucosa that comes into contact with the denture, often with associated soreness.
Diagnosis of Oral Candidiasis
The diagnosis of oral candidiasis is primarily clinical, based on the characteristic appearance of the lesions and the patient’s history. However, laboratory tests may be necessary in certain cases, particularly when the diagnosis is uncertain or when the patient does not respond to initial treatment.
- Clinical Examination
- Microscopic Examination
- Culture
- Histopathology
- Blood Tests
Clinical Examination
A thorough examination of the oral cavity is essential, including an assessment of the patient’s oral hygiene, denture use, and any other predisposing factors. The presence of characteristic white plaques, erythematous areas, or other lesions can help confirm the diagnosis.
Microscopic Examination
A potassium hydroxide (KOH) preparation of a sample taken from a suspected lesion can be used to visualize the presence of fungal elements, such as pseudohyphae or yeast cells, under a microscope. This is a quick and simple test that can confirm the presence of Candida.
Culture
In some cases, particularly when the diagnosis is uncertain, a culture of the lesion may be obtained. This involves taking a swab of the lesion and culturing it on appropriate media to identify the species of Candida. While this is more specific, it is not routinely necessary for most cases.
Histopathology
In rare cases, particularly when hyperplastic candidiasis is suspected, a biopsy of the lesion may be performed. Histopathological examination can reveal the presence of Candida hyphae within the epithelial layers, confirming the diagnosis.
Blood Tests
Blood tests are generally not required for diagnosing oral candidiasis but may be useful in identifying underlying conditions, such as diabetes or immunosuppression, that may be contributing to the infection.
Treatment of Oral Candidiasis
The treatment of oral candidiasis involves addressing the underlying cause, if identifiable, and the use of antifungal agents. Treatment varies depending on the severity of the infection, the patient’s overall health, and the presence of predisposing factors.
- Topical Antifungals
- Systemic Antifungals
- Management of Underlying Conditions
Topical Antifungals
For mild to moderate cases of oral candidiasis, topical antifungal agents are typically the first line of treatment. These agents include:
- Nystatin
- Clotrimazole
- Miconazole
Nystatin
Available as a suspension or lozenges, nystatin is a polyene antifungal that is commonly used to treat oral candidiasis. It is generally well-tolerated, although its taste can be unpleasant.
Clotrimazole
This azole antifungal is available as a lozenge and is effective against Candida albicans. It is often used when patients do not respond to nystatin or if they have a preference for an alternative agent.
Miconazole
Another azole antifungal, miconazole is available as an oral gel and is particularly useful for patients with denture-associated candidiasis.
Systemic Antifungals
In cases of severe or refractory oral candidiasis, or when the patient is immunocompromised, systemic antifungal therapy may be required. Commonly used systemic agents include:
- Fluconazole
- Itraconazole
- Amphotericin B
- Echinocandins
Fluconazole
This oral azole antifungal is commonly used for systemic treatment of oral candidiasis. It is generally well-tolerated and effective, particularly in cases that do not respond to topical therapy.
Itraconazole
Another systemic azole antifungal, itraconazole is sometimes used as an alternative to fluconazole, particularly in cases of fluconazole-resistant Candida species. It is available in both capsule and liquid forms and is usually reserved for more severe or refractory cases.
Amphotericin B
This polyene antifungal is used in severe cases, particularly in immunocompromised patients who do not respond to other treatments. However, due to its potential nephrotoxicity and the availability of safer alternatives, amphotericin B is typically used only in severe systemic infections.
Echinocandins
Drugs like caspofungin, micafungin, and anidulafungin are newer classes of antifungals that are effective against most Candida species, including those resistant to azoles. They are typically reserved for systemic infections or cases where other treatments have failed.
Management of Underlying Conditions
Successful treatment of oral candidiasis often requires addressing the underlying conditions that predispose the patient to infection. This may include:
- Improving Oral Hygiene
- Diabetes Management
- Reducing Xerostomia
- Adjusting Medications
- Addressing Nutritional Deficiencies
Improving Oral Hygiene
Educating patients on the importance of regular brushing, flossing, and proper denture care can help prevent the recurrence of oral candidiasis. Dentures should be cleaned thoroughly and removed at night to reduce the risk of denture stomatitis.
Diabetes Management
For patients with poorly controlled diabetes, achieving better glycemic control is crucial in reducing the risk of recurrent candidiasis. This may involve adjusting medications, diet, or exercise routines in consultation with a healthcare provider.
Reducing Xerostomia
Patients with dry mouth may benefit from increased hydration, the use of saliva substitutes, or medications that stimulate saliva production, such as pilocarpine. Avoiding caffeine, alcohol, and tobacco, which can exacerbate dry mouth, is also advisable.
Adjusting Medications
If oral candidiasis is related to the use of inhaled corticosteroids (common in asthma or COPD patients), rinsing the mouth with water after each use can help reduce the risk. Alternatively, switching to a lower-dose corticosteroid or a different delivery system may be considered.
Addressing Nutritional Deficiencies
Correcting deficiencies in iron, folic acid, or vitamin B12 can help bolster the immune system and reduce the risk of candidiasis.
Prevention of Oral Candidiasis
Preventing oral candidiasis involves a combination of good oral hygiene practices, proper management of underlying conditions, and sometimes prophylactic antifungal therapy in high-risk patients.
- Oral Hygiene
- Denture Care
- Prophylactic Antifungals
- Dietary Considerations
- Medication Management
Oral Hygiene
Maintaining good oral hygiene is essential in preventing oral candidiasis, particularly in those who are predisposed to the condition. This includes regular brushing and flossing, using an antiseptic mouthwash, and ensuring proper care of dentures.
Denture Care
For denture wearers, it is important to clean dentures thoroughly every day, remove them at night, and soak them in an antifungal solution if necessary. Ill-fitting dentures should be adjusted by a dental professional to avoid irritation and the subsequent risk of infection.
Prophylactic Antifungals
In some cases, such as in immunocompromised patients (e.g., those with HIV/AIDS or undergoing chemotherapy), prophylactic antifungal therapy may be prescribed to prevent oral candidiasis. This is particularly relevant for patients who have had previous episodes of candidiasis or are at high risk due to their underlying condition.
Dietary Considerations
Reducing sugar intake can help prevent oral candidiasis, as Candida thrives in environments rich in sugars. A balanced diet rich in nutrients that support the immune system is also beneficial.
Medication Management
For patients on long-term antibiotics or corticosteroids, regular monitoring and adjustments may be necessary to reduce the risk of developing oral candidiasis. For example, using a spacer with inhaled corticosteroids and rinsing the mouth afterward can significantly lower the risk.
Impact on Special Populations
Oral candidiasis can have a more significant impact on certain populations, particularly those who are immunocompromised or have other underlying health conditions. Understanding the specific challenges faced by these groups is crucial in managing and preventing the condition effectively.
- Immunocompromised Individuals
- Infants and Neonates
- Elderly Patients
- Patients with Diabetes
- Cancer Patients
Immunocompromised Individuals
Patients with compromised immune systems, such as those with HIV/AIDS, cancer, or organ transplants, are at a higher risk of developing severe and recurrent oral candidiasis. In these individuals, the infection may be more resistant to treatment, and the risk of systemic spread (candidemia) is higher. Prophylactic antifungal therapy and regular monitoring are often necessary for these patients.
Infants and Neonates
Oral candidiasis is relatively common in infants, often due to their immature immune systems and exposure to Candida during birth or breastfeeding. While usually mild, thrush in infants can cause feeding difficulties and discomfort. Treatment typically involves topical antifungals, and in breastfeeding mothers, both the infant and mother may need treatment to prevent reinfection.
Elderly Patients
The elderly population, particularly those in long-term care facilities, are at an increased risk of oral candidiasis due to factors such as xerostomia, poor oral hygiene, and the use of dentures. In this group, the condition can cause significant discomfort, nutritional issues due to pain while eating, and a higher risk of systemic infection. Preventive measures and early treatment are key to managing oral candidiasis in the elderly.
Patients with Diabetes
Poorly controlled diabetes increases the risk of oral candidiasis due to hyperglycemia and impaired immune function. These patients may experience more frequent and severe episodes of candidiasis, and managing their blood sugar levels is crucial in preventing the condition. Regular dental check-ups and good oral hygiene practices are also important.
Cancer Patients
Those undergoing chemotherapy or radiation therapy, particularly for head and neck cancers, are at high risk of developing oral candidiasis due to mucosal damage and immunosuppression. In these patients, oral candidiasis can contribute to mucositis, a painful condition that can severely impact the ability to eat and speak. Prophylactic antifungal therapy, along with meticulous oral care, is often recommended.
Complications of Oral Candidiasis
While oral candidiasis is generally considered a mild and treatable condition, it can lead to complications if left untreated, particularly in high-risk populations.
- Chronic Mucocutaneous Candidiasis (CMC)
- Candidemia
- Esophageal Candidiasis
- Nutritional Deficiencies
Chronic Mucocutaneous Candidiasis (CMC)
In some cases, particularly in patients with specific immunodeficiencies, oral candidiasis can become chronic and resistant to treatment, leading to chronic mucocutaneous candidiasis. This condition involves persistent and widespread infection of the skin, nails, and mucous membranes and can be challenging to manage.
Candidemia
In severely immunocompromised patients, untreated oral candidiasis can lead to the spread of Candida into the bloodstream, resulting in candidemia. This is a serious, life-threatening condition that requires aggressive systemic antifungal therapy and hospitalization.
Esophageal Candidiasis
Oral candidiasis can extend into the esophagus, particularly in immunocompromised patients, leading to esophageal candidiasis. This condition can cause severe pain and difficulty swallowing and may require systemic antifungal treatment.
Nutritional Deficiencies
Chronic or severe oral candidiasis can cause significant discomfort, leading to reduced food intake and subsequent nutritional deficiencies. This is particularly concerning in vulnerable populations, such as the elderly, infants, and those with chronic illnesses.
Prognosis for Oral Candidiasis
The prognosis for oral candidiasis is generally good, particularly when the condition is diagnosed early and treated appropriately. Most cases respond well to topical or systemic antifungal therapy, and with proper management of underlying conditions, recurrence can often be prevented.
However, in high-risk populations, such as those with severe immunosuppression or poorly controlled diabetes, the condition can be more difficult to treat and may recur frequently. In such cases, ongoing management and preventive measures are essential to maintaining oral health and preventing complications.
Frequently Asked Questions (FAQs)
What is the main cause of oral candidiasis?
Oral candidiasis, also known as oral thrush, is primarily caused by an overgrowth of the Candida fungus, particularly Candida albicans. This yeast naturally lives in the mouth, digestive tract, and skin without causing harm. However, when the balance of microorganisms in the body is disrupted, Candida can grow uncontrollably and lead to infection.
Common causes include:
- Weakened immune system – People with HIV/AIDS, cancer patients undergoing chemotherapy, or organ transplant recipients taking immunosuppressants are at higher risk.
- Use of antibiotics – Broad-spectrum antibiotics kill both harmful and beneficial bacteria, allowing Candida to thrive.
- Diabetes – High blood sugar levels create a favorable environment for yeast growth.
- Dry mouth (Xerostomia) – Saliva helps control the growth of Candida, so a lack of saliva can contribute to an overgrowth.
- Poor oral hygiene – Not brushing or flossing regularly can encourage fungal infections.
- Smoking – Tobacco use weakens oral tissues and promotes Candida overgrowth.
- Denture use – Ill-fitting dentures can cause irritation, leading to yeast buildup.
What kills Candida fast in the mouth?
To eliminate Candida quickly, a combination of antifungal medications, natural remedies, and lifestyle changes is recommended.
Effective treatments include:
Prescription antifungal medications:
- Nystatin (oral rinse or lozenge) – Kills Candida upon contact.
- Clotrimazole (troche/lozenge) – Slowly dissolves in the mouth to combat the infection.
- Fluconazole (oral pill) – Used for more severe cases or recurrent infections.
Natural remedies:
- Coconut oil pulling – Contains caprylic acid, which has antifungal properties.
- Baking soda rinse – Helps neutralize acidity and disrupts Candida growth.
- Apple cider vinegar rinse – Diluted vinegar has antifungal effects that can inhibit Candida.
- Probiotic foods (yogurt, kefir, sauerkraut) – Help restore beneficial bacteria in the mouth.
Maintaining good oral hygiene and avoiding sugary foods that feed Candida can also speed up recovery.
How do you treat oral Candida?
Oral candidiasis is treated with a combination of medical and home-based treatments.
Medical treatments include:
- Topical antifungal medications: Nystatin mouthwash, clotrimazole lozenges, or miconazole gel.
- Oral antifungals: Fluconazole or itraconazole pills, prescribed for severe or resistant cases.
Home remedies and preventive measures:
- Good oral hygiene – Brush your teeth twice a day, floss daily, and clean your tongue.
- Antifungal mouth rinses – Rinsing with salt water, baking soda, or diluted apple cider vinegar can help control yeast growth.
- Limit sugar and refined carbs – Candida thrives on sugar, so reducing intake can prevent overgrowth.
- Probiotics – Consuming yogurt or probiotic supplements can help restore balance in the mouth and gut.
- Denture care – If you wear dentures, clean them daily and ensure they fit properly.
Is oral candidiasis an STD?
No, oral candidiasis is not considered a sexually transmitted disease (STD). However, it can be transmitted through oral contact, such as kissing or oral sex, especially if one person has an active infection and the other has a weakened immune system.
Factors that may increase the risk of transmission include:
- Having a compromised immune system
- Taking antibiotics or steroids
- Suffering from diabetes
- Poor oral hygiene
While it is not classified as an STD, it can still spread through intimate contact and cause infections in different parts of the body.
What are the red flags of oral thrush?
The main signs and symptoms of oral thrush include:
- White, creamy lesions on the tongue, inside of the cheeks, gums, roof of the mouth, and throat.
- Pain and soreness in the affected areas, which may make eating or drinking uncomfortable.
- Loss of taste or a cottony feeling in the mouth.
- Cracking and redness at the corners of the mouth (angular cheilitis).
- Difficulty swallowing in severe cases, when the infection spreads to the esophagus.
If symptoms persist or worsen, consult a doctor for medical treatment.
What are four causes of candidiasis?
Candidiasis can be caused by several factors, but four of the most common include:
- Weakened immune system – People with weakened immunity due to diseases like HIV/AIDS or cancer are more prone to Candida infections.
- Use of antibiotics – Antibiotics kill beneficial bacteria that normally keep Candida under control, allowing it to multiply.
- Diabetes and high blood sugar – Candida feeds on sugar, making people with uncontrolled diabetes more susceptible.
- Poor oral hygiene or denture use – Not brushing, flossing, or cleaning dentures properly can contribute to yeast overgrowth.
What are the warning signs of Candida?
Candida infections can affect different areas of the body, leading to various symptoms.
Common warning signs include:
- Oral thrush: White patches on the tongue, inside the mouth, or throat.
- Digestive issues: Bloating, gas, diarrhea, or constipation due to gut Candida overgrowth.
- Chronic fatigue: Candida overgrowth can contribute to low energy and brain fog.
- Frequent yeast infections: Itchy, irritated skin in warm, moist areas such as the groin, under breasts, and armpits.
- Recurring UTIs or vaginal yeast infections: Symptoms include itching, burning, and unusual discharge.
What kills Candida in the gut fast?
To quickly eliminate Candida overgrowth in the gut, follow these steps:
- Adopt an anti-Candida diet – Reduce sugar, processed foods, and refined carbohydrates, which feed Candida.
- Consume antifungal foods and supplements:Garlic (allicin has antifungal properties), Coconut oil (caprylic acid kills yeast), Oregano oil (powerful antifungal), Pau d’arco tea (natural antifungal)
- Take probiotics – Restore healthy gut bacteria to keep Candida in check.
- Use prescription antifungals (if necessary) – Medications like fluconazole or nystatin may be required for severe cases.
What drink kills yeast infections?
Certain drinks contain antifungal properties that may help fight Candida and yeast infections.
- Unsweetened cranberry juice – Helps maintain an acidic environment that inhibits yeast growth.
- Apple cider vinegar (ACV) drink – Diluted in water, ACV helps balance gut flora and has antifungal properties.
- Ginger tea – Contains compounds that help reduce inflammation and fight Candida.
- Lemon water – Alkalizes the body and may create an environment less favorable for yeast growth.
- Probiotic drinks (kefir, kombucha) – Promote beneficial bacteria, which help keep Candida in check.
Conclusion
Oral candidiasis is a common fungal infection that affects a wide range of individuals, from infants to the elderly, and can be a sign of underlying health issues, particularly in immunocompromised patients. Understanding the risk factors, clinical manifestations, and treatment options is essential for healthcare providers in managing this condition effectively.
Early diagnosis and appropriate treatment, combined with preventive measures such as good oral hygiene and the management of underlying conditions, can significantly improve outcomes for patients with oral candidiasis. For those at higher risk, such as the immunocompromised or the elderly, ongoing monitoring and, in some cases, prophylactic antifungal therapy may be necessary to prevent recurrence and complications.
As research continues to evolve, new antifungal agents and treatment strategies may offer improved outcomes for patients with oral candidiasis, particularly those with resistant or recurrent infections. For now, a comprehensive approach that includes patient education, regular dental care, and tailored treatment plans remains the cornerstone of effective management of this condition.