Menopause is a natural biological process that marks the end of a woman’s reproductive years. It typically occurs around the age of 45 to 55, although the exact age can vary widely among individuals. During menopause, a woman’s body undergoes significant hormonal changes, particularly a decrease in estrogen levels. While most people are aware of the physical and emotional symptoms associated with menopause, such as hot flashes, mood swings, and night sweats, many are unaware of its potential impact on oral health. As dentists, understanding the oral health implications of menopause is crucial for providing comprehensive care to our patients. In this article, we will explore the effects of menopause on oral health and discuss strategies for managing these changes in the dental setting.
Table of Contents
ToggleSymptoms of Menopause
The symptoms of menopause can vary widely among individuals, and some women may experience few or no symptoms at all. However, common symptoms of menopause include:
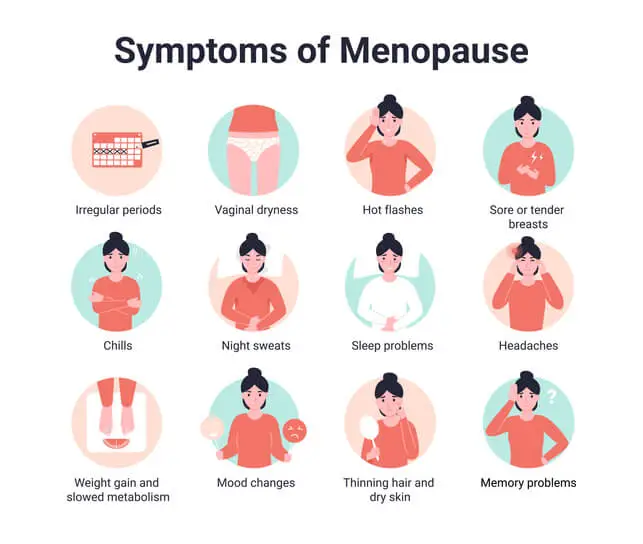
- Irregular periods
- Hot flashes
- Night sweats
- Vaginal dryness and discomfort
- Mood changes
- Sleep disturbances
- Fatigue
- Changes in libido
- Cognitive changes
- Physical changes
Irregular periods
Menstrual cycles may become irregular in the years leading up to menopause (perimenopause) and eventually stop altogether.
Hot flashes
Sudden feelings of warmth, often accompanied by sweating and flushing of the face and neck.
Night sweats
Similar to hot flashes but occurring during sleep, leading to night waking and disrupted sleep patterns.
Vaginal dryness and discomfort
Decreased estrogen levels can lead to thinning and dryness of the vaginal tissues, causing discomfort during intercourse and an increased risk of urinary tract infections.
Mood changes
Hormonal fluctuations during menopause can lead to mood swings, irritability, anxiety, and even depression in some women.
Sleep disturbances
Night sweats and hormonal changes can disrupt sleep patterns, leading to insomnia or poor-quality sleep.
Fatigue
Some women may experience increased fatigue or a lack of energy during menopause.
Changes in libido
Fluctuating hormone levels can affect sexual desire and arousal in some women.
Cognitive changes
Some women may experience difficulty concentrating, memory lapses, or “brain fog” during menopause.
Physical changes
Menopause can also be associated with changes in weight distribution, hair thinning or loss, and changes in skin elasticity.
It’s important to note that not all women will experience all of these symptoms, and the severity of symptoms can vary widely. Additionally, symptoms can begin during perimenopause (the transitional period leading up to menopause) and may continue for several years after menopause.
Hormonal Changes and Oral Health
Estrogen plays a crucial role in maintaining oral health by protecting the integrity of the oral mucosa, promoting saliva production, and supporting bone density in the jaw. During menopause, the decline in estrogen levels can lead to several oral health issues, including:
- Dry Mouth (Xerostomia)
- Gum Disease (Periodontitis)
- Oral Discomfort
Dry Mouth (Xerostomia)
Estrogen helps stimulate saliva production, so a decrease in estrogen levels can result in reduced saliva flow. This condition, known as xerostomia, can increase the risk of cavities, gum disease, and oral infections due to a lack of protective saliva.
Gum Disease (Periodontitis)
Estrogen deficiency can contribute to changes in the oral microbiome and alter the body’s immune response, making women more susceptible to gum disease during menopause. Additionally, hormonal fluctuations may exacerbate existing periodontal conditions, leading to inflammation, bleeding gums, and bone loss around the teeth.
Oral Discomfort
Menopausal women may experience oral discomfort, including burning mouth syndrome, altered taste perception, and increased sensitivity to spicy or acidic foods. These symptoms can affect a woman’s quality of life and may require intervention from dental professionals.
Osteoporosis and Tooth Loss
Menopause is also associated with a decrease in bone density, a condition known as osteoporosis. While osteoporosis primarily affects the bones of the spine, hips, and wrists, it can also impact the jawbone, leading to tooth loss and compromised oral health. Women with osteoporosis may experience tooth mobility, bone resorption around the teeth, and an increased risk of dental fractures. Dentists should be vigilant in assessing the oral health of menopausal women with osteoporosis and implementing appropriate preventive measures to maintain their oral function and aesthetics.
Menopausal Medications and Oral Health
Many menopausal women may be prescribed medications to manage symptoms such as hot flashes, mood swings, and osteoporosis. Some of these medications, such as hormone replacement therapy (HRT) and bisphosphonates, can have implications for oral health:
- Hormone Replacement Therapy (HRT)
- Bisphosphonates
Hormone Replacement Therapy (HRT)
While HRT can alleviate menopausal symptoms by supplementing estrogen levels, it may also affect oral health. Studies have suggested that women taking HRT may have a reduced risk of tooth loss and gum disease compared to those who do not. However, HRT has been associated with an increased risk of blood clots and certain cancers, so its use should be carefully considered based on individual risk factors and medical history.
Bisphosphonates
Bisphosphonates are commonly prescribed to treat osteoporosis and prevent bone loss. However, long-term use of these medications has been linked to a rare but serious condition called medication-related osteonecrosis of the jaw (MRONJ). Dentists should be aware of this potential complication and collaborate with physicians to minimize the risk of MRONJ in menopausal women undergoing bisphosphonate therapy.
Oral Health Management Strategies
To effectively manage the oral health needs of menopausal women, dentists can implement the following strategies:
- Comprehensive Oral Examinations
- Oral Hygiene Education
- Saliva Substitutes and Moisturizers
- Periodontal Therapy
- Collaboration with Healthcare Providers
- Regular Dental Visits
Comprehensive Oral Examinations
Conduct thorough oral examinations to assess for signs of gum disease, dry mouth, tooth mobility, and other menopause-related oral health issues.
Oral Hygiene Education
Provide tailored oral hygiene instructions to menopausal women, emphasizing the importance of regular brushing, flossing, and using fluoridated oral care products to maintain oral health.
Saliva Substitutes and Moisturizers
Recommend saliva substitutes, mouth rinses, or moisturizing gels to alleviate dry mouth symptoms and minimize the risk of dental caries and oral infections.
Periodontal Therapy
Offer periodontal therapy, including scaling and root planing, to manage gum disease and prevent further progression of periodontal conditions in menopausal women.
Collaboration with Healthcare Providers
Collaborate with primary care physicians, gynecologists, and other healthcare providers to coordinate care for menopausal women, especially those receiving hormone therapy or medications that may affect oral health.
Regular Dental Visits
Encourage menopausal women to maintain regular dental visits for preventive care, early detection of oral health issues, and timely intervention to preserve oral function and aesthetics.
Special Considerations for Dental Procedures
Menopausal women may require special considerations during dental procedures to minimize potential complications and ensure optimal outcomes. Dentists should be mindful of the following factors:
- Bleeding Risk
- Bone Density
- Medication Considerations
- Stress Management
Bleeding Risk
Due to hormonal changes and potential underlying medical conditions, menopausal women may be at an increased risk of bleeding during dental procedures. Dentists should obtain a thorough medical history, including information about any bleeding disorders or medications that may affect blood clotting, and take appropriate precautions to manage bleeding during treatment.
Bone Density
Women undergoing menopause are at risk of osteoporosis and decreased bone density, which may affect the success of dental procedures such as dental implant placement or tooth extraction. Dentists should assess bone density using imaging techniques such as panoramic radiographs or cone-beam computed tomography (CBCT) and consider alternative treatment options or modifications to the surgical approach to optimize outcomes in menopausal women with compromised bone quality.
Medication Considerations
Dentists should be aware of any medications that menopausal women are taking, including hormone therapy, bisphosphonates, and other medications that may impact oral health or alter the response to dental treatment. Collaboration with the patient’s healthcare providers is essential to ensure safe and effective dental care while minimizing the risk of adverse drug interactions or complications.
Stress Management
Menopausal women may experience increased stress and anxiety related to hormonal changes and associated symptoms. Dentists should be sensitive to the emotional needs of menopausal patients and employ strategies to alleviate anxiety, such as providing a calming environment, explaining procedures thoroughly, and offering sedation options if necessary.
Future Directions in Menopausal Dentistry
As our understanding of the oral health implications of menopause continues to evolve, future research directions in menopausal dentistry may include:
- Hormonal Therapies
- Personalized Treatment Approaches
- Multidisciplinary Collaboration
- Patient Education and Empowerment
Hormonal Therapies
Investigating the effects of hormonal therapies on oral health outcomes in menopausal women, including the potential benefits and risks of hormone replacement therapy (HRT) and alternative treatment options for managing menopausal symptoms while minimizing oral health complications.
Personalized Treatment Approaches
Developing personalized treatment approaches for menopausal women based on individual risk factors, including genetic predisposition, medical history, and hormonal status, to optimize oral health outcomes and quality of life during menopause and beyond.
Multidisciplinary Collaboration
Promoting collaboration between dental professionals, gynecologists, endocrinologists, and other healthcare providers to provide comprehensive care for menopausal women, address systemic health issues, and optimize overall well-being through an integrated approach to healthcare.
Patient Education and Empowerment
Empowering menopausal women to take an active role in their oral health by providing tailored education, resources, and support to help them navigate the unique challenges of menopause and make informed decisions about their dental care.
Conclusion
Menopause is a significant life transition that can impact oral health through hormonal changes, osteoporosis, and medication use. Dentists play a crucial role in addressing the oral health needs of menopausal women by conducting comprehensive evaluations, providing education and preventive care, and collaborating with other healthcare professionals to optimize patient outcomes. By understanding the unique challenges faced by menopausal women and implementing targeted interventions, dentists can contribute to improving the overall health and well-being of their patients during this transitional phase of life. Continued research and multidisciplinary collaboration are essential for advancing our understanding of menopausal dentistry and developing personalized approaches to care for menopausal women.

