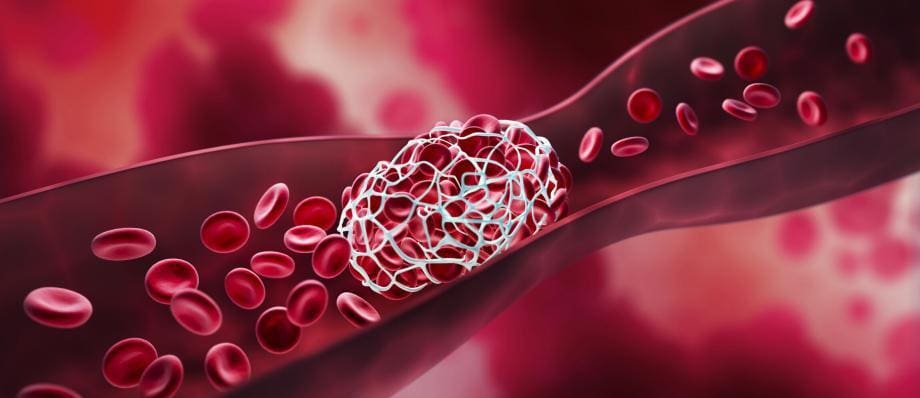
The blood clotting process, also known as hemostasis, is a complex and essential mechanism that ensures the integrity of our circulatory system. When a blood vessel is injured, the body initiates a series of events to stop bleeding and repair the damage. While this process is crucial for our survival, it can also lead to health issues when it goes awry. In this comprehensive guide, we will delve into the intricacies of the blood clotting process, its significance, regulation, and potential complications.
Components of Blood Clotting
- Blood Vessels
- Blood Cells
Blood Vessels
Blood clotting primarily takes place within our blood vessels, which can be broadly classified into three types: arteries, veins, and capillaries. Arteries carry oxygenated blood away from the heart, while veins return deoxygenated blood to the heart. Capillaries, on the other hand, are tiny blood vessels that connect arteries and veins. The type of blood vessel involved in an injury affects the clotting process.
Blood Cells
Blood consists of various components, including red blood cells (RBCs), white blood cells (WBCs), and platelets, suspended in a liquid known as plasma. Platelets, also called thrombocytes, are crucial to the clotting process. When a blood vessel is injured, platelets play a vital role in forming a temporary plug to stop bleeding.
Phases of Blood Clotting
The blood clotting process occurs in several phases:
- Vasoconstriction
- Primary Hemostasis
- Secondary Hemostasis
- Clot Retraction and Repair
- Fibrinolysis
Vasoconstriction
When a blood vessel is injured, it first undergoes vasoconstriction, which is the narrowing of the vessel to reduce blood flow to the site of injury. This constriction is primarily a reflex response and helps minimize blood loss.
Primary Hemostasis
Primary hemostasis involves the formation of a temporary plug at the site of injury. It is primarily mediated by platelets. When exposed to collagen in the damaged blood vessel wall, platelets become activated and adhere to the site. This adhesion is followed by platelet aggregation, where platelets stick together to form a plug.
Secondary Hemostasis
Secondary hemostasis is the next step in the process and involves the coagulation cascade, a series of chemical reactions that ultimately leads to the formation of a stable blood clot. This cascade consists of various clotting factors, including fibrinogen, prothrombin, and thrombin. These factors interact in a complex sequence, culminating in the conversion of soluble fibrinogen into insoluble fibrin threads. These threads create a mesh that traps blood cells, forming a solid clot.
Clot Retraction and Repair
Once the clot is formed, it begins to contract and pull the edges of the broken blood vessel closer together. This process, known as clot retraction, helps in sealing the wound. Concurrently, tissue repair mechanisms are initiated to heal the damaged blood vessel.
Fibrinolysis
After the wound is healed, the body initiates fibrinolysis, which is the process of breaking down the fibrin clot. Plasmin, an enzyme, plays a crucial role in this phase, ensuring that the clot is dissolved, and blood flow is restored to normal.
Regulation of Blood Clotting
The blood clotting process is tightly regulated to prevent excessive clot formation, which can lead to serious health issues such as thrombosis or embolism. Several mechanisms ensure a delicate balance in clotting:
- Anticoagulants
- Endothelial Cells
- Platelet Inhibition
Anticoagulants
The body produces natural anticoagulants to prevent excessive clotting. These include heparin, which inhibits clotting factors, and proteins C and S, which regulate the coagulation cascade.
Endothelial Cells
The endothelial cells lining the blood vessels play a vital role in maintaining a non-thrombotic state. They release substances like prostacyclin and nitric oxide, which inhibit platelet aggregation and promote vasodilation, respectively.
Platelet Inhibition
Platelet activation and aggregation are tightly controlled to prevent uncontrolled clotting. Aspirin, for example, inhibits platelet function and is often prescribed to reduce the risk of cardiovascular events.
Blood Clotting Disorders
Disruptions in the blood clotting process can lead to various disorders, including:
- Hemophilia
- Thrombophilia
- Disseminated Intravascular Coagulation (DIC)
Hemophilia
Hemophilia is a genetic disorder characterized by a deficiency in clotting factors, particularly Factor VIII (Hemophilia A) or Factor IX (Hemophilia B). Individuals with hemophilia experience prolonged bleeding and bruising, even with minor injuries.
Thrombophilia
Thrombophilia refers to a group of conditions where individuals have an increased tendency to develop blood clots. This can lead to deep vein thrombosis (DVT), pulmonary embolism, or stroke. Common thrombophilic conditions include Factor V Leiden mutation and antiphospholipid syndrome.
Disseminated Intravascular Coagulation (DIC)
DIC is a life-threatening condition characterized by excessive clot formation throughout the body, followed by bleeding. It often occurs in response to severe illnesses, such as sepsis, trauma, or cancer.
Clinical Applications
Understanding the blood clotting process is essential in medicine for various reasons:
- Surgery
- Anticoagulant Therapy
- Monitoring and Diagnostics
Surgery
Surgeons must carefully manage blood clotting during procedures to prevent excessive bleeding or clot formation, which can lead to complications.
Anticoagulant Therapy
Patients at risk of excessive clotting, such as those with atrial fibrillation or deep vein thrombosis, may require anticoagulant medications like warfarin or direct oral anticoagulants (DOACs) to prevent clot formation.
Monitoring and Diagnostics
Various tests, such as prothrombin time (PT), activated partial thromboplastin time (aPTT), and international normalized ratio (INR), help assess the blood’s clotting ability and diagnose clotting disorders.
Future Directions
Research in blood clotting continues to advance our understanding of the process and its regulation. Emerging technologies and therapies aim to improve the treatment of clotting disorders and reduce the risks associated with anticoagulation therapy.
Targeted Therapies
Advancements in biotechnology allow for the development of more targeted therapies for clotting disorders, minimizing side effects and optimizing treatment.
Personalized Medicine
Genetic testing can help identify individuals at risk of clotting disorders, enabling personalized treatment plans and preventive measures.
Artificial Blood
Scientists are working on developing artificial blood substitutes that can mimic the oxygen-carrying capacity of red blood cells while minimizing the risk of clot formation.
Conclusion
The blood clotting process is a remarkable and intricate mechanism that safeguards our circulatory system. While essential for our survival, it also poses risks when it malfunctions. Understanding the various components, phases, and regulation of blood clotting is crucial for healthcare professionals and patients alike. With ongoing research and advancements in medical science, we can better manage clotting disorders and improve patient outcomes while maintaining the delicate balance of hemostasis in the body.