Measles, a highly contagious viral disease, has been a significant public health concern for centuries. Despite the development of an effective vaccine, measles continues to pose a threat in many parts of the world. This article delves into the history, transmission, symptoms, treatment, and prevention of measles, as well as the challenges and successes in the fight against this preventable disease.
Table of Contents
ToggleHistory of Measles
Measles, also known as rubeola, is one of the oldest known diseases, with records dating back to at least the 9th century. The Persian physician Rhazes (Muhammad ibn Zakariya al-Razi) first described the disease in detail in the 10th century. However, it wasn’t until the 18th century that measles was recognized as a distinct illness from smallpox and other febrile diseases.
The virus responsible for measles, a member of the Paramyxoviridae family, was identified in 1954 by John F. Enders and Thomas C. Peebles. This discovery was crucial in the development of the first effective measles vaccine, which was introduced in 1963. The widespread use of the vaccine led to a dramatic decline in measles cases and deaths, especially in developed countries.
Transmission and Epidemiology
Measles is one of the most contagious diseases known to humans. The virus is transmitted primarily through respiratory droplets when an infected person coughs or sneezes. It can also spread by direct contact with nasal or throat secretions of infected individuals. The virus can remain infectious in the air or on surfaces for up to two hours.
The basic reproduction number (R0) for measles is estimated to be between 12 and 18, meaning that one infected person can potentially spread the virus to 12-18 susceptible individuals. This high R0 underscores the importance of high vaccination coverage to achieve herd immunity and prevent outbreaks.
Symptoms and Clinical Presentation
The incubation period for measles is typically 10-12 days from exposure to the onset of symptoms. The disease progresses through several stages:
- Prodromal Stage
- Exanthem Stage
- Recovery Stage
Prodromal Stage
This stage lasts 2-4 days and is characterized by high fever, cough, runny nose (coryza), and conjunctivitis (red, watery eyes). Koplik’s spots, small white lesions on the inner cheeks, may appear during this stage and are pathognomonic for measles.
Exanthem Stage
A maculopapular rash begins on the face and spreads downward to the trunk and limbs. The rash typically lasts for 5-6 days and fades in the same order it appeared. The fever often peaks with the appearance of the rash and gradually subsides thereafter.
Recovery Stage
The rash fades, and symptoms improve, but the person may still be contagious for several days after the rash onset. Complications can arise during this stage, especially in individuals with weakened immune systems or underlying health conditions.
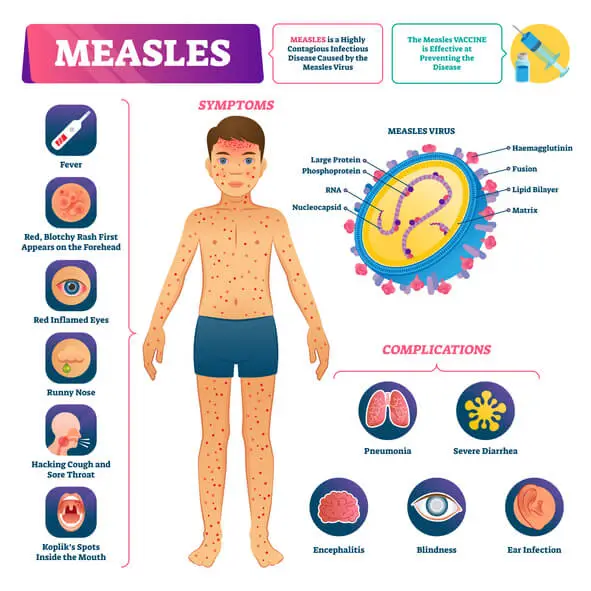
Complications of Measles
While measles is often self-limiting, it can lead to severe complications, particularly in young children, pregnant women, and immunocompromised individuals. Common complications include:
- Otitis Media
- Pneumonia
- Diarrhea
- Encephalitis
- Subacute Sclerosing Panencephalitis (SSPE)
Otitis Media
Middle ear infection, which can lead to hearing loss.
Pneumonia
A serious lung infection and the leading cause of death associated with measles.
Diarrhea
Can lead to dehydration, especially in young children.
Encephalitis
Inflammation of the brain, which can result in seizures, brain damage, or death.
Subacute Sclerosing Panencephalitis (SSPE)
A rare, fatal, degenerative disease of the central nervous system that occurs years after measles infection.
Diagnosis and Treatment
Measles is typically diagnosed based on clinical presentation and history of exposure. Laboratory confirmation can be obtained through serological testing for measles-specific IgM antibodies or reverse transcription polymerase chain reaction (RT-PCR) for measles RNA.
There is no specific antiviral treatment for measles. Management focuses on supportive care to relieve symptoms and prevent complications. This includes:
- Hydration
- Antipyretics
- Vitamin A
Hydration
Ensuring adequate fluid intake to prevent dehydration.
Antipyretics
Medications like acetaminophen or ibuprofen to reduce fever and alleviate discomfort.
Vitamin A
Supplementation in children, as it has been shown to reduce the severity of symptoms and complications.
Hospitalization may be necessary for severe cases or complications, particularly in young children and immunocompromised individuals.
Prevention and Vaccination
Vaccination is the most effective way to prevent measles. The measles vaccine, often administered as part of the combined measles, mumps, and rubella (MMR) vaccine, is highly effective. Two doses of the MMR vaccine provide approximately 97% protection against measles.
The World Health Organization (WHO) recommends that all children receive two doses of the MMR vaccine, with the first dose given at 9-12 months of age and the second dose at 15-18 months or at school entry. In countries with high measles transmission, the first dose may be given as early as 6 months, with subsequent doses according to the national immunization schedule.
High vaccination coverage is essential to achieve herd immunity and prevent outbreaks. Herd immunity for measles requires about 95% of the population to be immunized, which helps protect those who cannot be vaccinated, such as infants and individuals with certain medical conditions.
Global Measles Control and Elimination Efforts
Significant progress has been made in reducing measles cases and deaths worldwide. According to the WHO, global measles mortality decreased by 73% between 2000 and 2018, thanks to widespread vaccination efforts. However, challenges remain, particularly in low- and middle-income countries with weak health systems and low vaccination coverage.
The WHO and its partners have set ambitious goals for measles control and elimination. The Global Vaccine Action Plan aims to achieve measles elimination in at least five WHO regions by 2020. Despite setbacks, efforts continue to strengthen immunization programs, improve surveillance, and respond to outbreaks.
Challenges in Measles Elimination
Several challenges hinder the global elimination of measles:
- Vaccine Hesitancy
- Health System Barriers
- Conflict and Displacement
- Global Mobility
Vaccine Hesitancy
Misinformation and misconceptions about vaccine safety have led to vaccine hesitancy in some communities, resulting in lower vaccination rates and outbreaks of measles.
Health System Barriers
Inadequate healthcare infrastructure, lack of access to vaccines, and insufficient healthcare worker training can impede vaccination efforts.
Conflict and Displacement
Armed conflicts, political instability, and displacement of populations can disrupt vaccination programs and increase the risk of measles transmission.
Global Mobility
International travel can facilitate the spread of measles, as travelers from areas with high measles transmission can introduce the virus to regions where it had been eliminated.
Success Stories and Lessons Learned
Despite the challenges, there have been notable successes in measles control and elimination. For example, the Americas region achieved measles elimination in 2016, thanks to sustained high vaccination coverage and strong public health systems. Although imported cases have occurred, rapid response measures have prevented widespread transmission.
Countries like Bhutan, Maldives, and Sri Lanka have also achieved measles elimination, demonstrating that even resource-limited nations can succeed with strong political commitment, robust health systems, and community engagement.
Key lessons from these success stories include the importance of:
- Political Commitment
- Community Engagement
- Strong Surveillance Systems
- Integration with Other Health Services
Political Commitment
Strong leadership and sustained political commitment are crucial for the success of measles elimination programs.
Community Engagement
Involving communities in vaccination efforts helps build trust and address vaccine hesitancy.
Strong Surveillance Systems
Effective surveillance and rapid response to outbreaks are essential to detect and contain measles transmission.
Integration with Other Health Services
Integrating measles vaccination with other health services, such as routine immunizations and maternal and child health programs, can improve coverage and efficiency.
The Future of Measles Control and Elimination
Looking ahead, achieving global measles elimination will require renewed efforts and innovative strategies. Key priorities include:
- Strengthening Health Systems
- Addressing Vaccine Hesitancy
- Enhancing Surveillance and Outbreak Response
- Reaching Underserved Populations
- Global Collaboration
Strengthening Health Systems
Investing in health infrastructure, training healthcare workers, and ensuring reliable vaccine supply chains are essential for improving vaccination coverage and response to outbreaks.
Addressing Vaccine Hesitancy
Combating misinformation and building public trust in vaccines through effective communication strategies, community engagement, and addressing the root causes of vaccine hesitancy.
Enhancing Surveillance and Outbreak Response
Strengthening surveillance systems to detect and respond to measles cases and outbreaks promptly, including the use of new technologies for real-time monitoring and data analysis.
Reaching Underserved Populations
Ensuring that vaccination efforts reach marginalized and underserved populations, including those in remote areas, conflict zones, and refugee camps.
Global Collaboration
Sustaining and enhancing international cooperation and partnerships to support measles control and elimination efforts, particularly in regions with high disease burden.
Oral Manifestations of Measles
One of the hallmark features of measles is its distinctive oral manifestations. These signs are not only important for diagnosing measles but also have implications for oral health:
- Koplik’s Spots
- Ulcerative Stomatitis
- Secondary Oral Infections
Koplik’s Spots
Koplik’s spots are pathognomonic for measles and are considered an early diagnostic sign. These are small, bluish-white lesions with a red halo, typically appearing on the buccal mucosa opposite the lower molars. They precede the characteristic skin rash by 1-2 days and usually fade as the rash appears. While Koplik’s spots themselves are not harmful, their presence can indicate an active measles infection, prompting the need for isolation and careful management to prevent the spread of the virus.
Ulcerative Stomatitis
During a measles infection, patients may develop ulcerative stomatitis, characterized by painful ulcers in the mouth. These ulcers can make eating and drinking difficult, contributing to dehydration and nutritional deficiencies, particularly in young children.
Secondary Oral Infections
Measles weakens the immune system, making individuals more susceptible to secondary infections, including those in the oral cavity. Some of the secondary oral infections that can occur during or after measles include:
Oral Thrush (Candidiasis)
The immunosuppressive effects of measles can lead to an overgrowth of Candida species in the mouth, resulting in oral thrush. This fungal infection appears as creamy white lesions on the tongue, inner cheeks, and sometimes the roof of the mouth, gums, and tonsils. Oral thrush can cause discomfort, pain, and difficulty swallowing.
Herpes Simplex Virus (HSV) Infections
Reactivation of herpes simplex virus (HSV) can occur during or after a measles infection, leading to herpetic stomatitis or cold sores. These painful blisters can form on the lips, gums, and other oral tissues, further complicating oral health during the recovery phase of measles.
Impact on Oral Hygiene and Dental Care
The systemic symptoms of measles, such as high fever, malaise, and general discomfort, can lead to neglect of oral hygiene. This neglect, combined with a weakened immune system, increases the risk of dental problems, such as:
- Dental Caries
- Gingivitis and Periodontitis
Dental Caries
Reduced oral hygiene during a measles infection can lead to an increased risk of dental caries. The presence of Koplik’s spots, ulcerative stomatitis, and secondary infections can make routine oral care, like brushing and flossing, more painful and challenging. This can result in the buildup of plaque and the development of cavities.
Gingivitis and Periodontitis
Poor oral hygiene and the immunosuppressive effects of measles can contribute to the development of gingivitis, an inflammation of the gums. If left untreated, gingivitis can progress to periodontitis, a more severe form of gum disease that can lead to tooth loss and other serious oral health issues.
Considerations for Dental Care During Measles
Providing dental care to patients with measles requires special considerations to ensure the safety of both the patient and the dental care team:
- Infection Control
- Isolation
- Protective Equipment
- Disinfection
Infection Control
Measles is highly contagious, so strict infection control measures are necessary to prevent the spread of the virus in dental settings. This includes:
Isolation
Patients with active measles should be isolated to prevent transmission. Non-urgent dental procedures should be postponed until the patient is no longer contagious.
Protective Equipment
Dental care providers should use appropriate personal protective equipment (PPE), including masks, gloves, and eye protection, when treating patients with measles.
Disinfection
Thorough disinfection of all surfaces and instruments is crucial to prevent the spread of the virus.
Pain Management
Managing pain and discomfort is essential for patients with oral manifestations of measles. This may involve:
- Topical Anesthetics
- Systemic Pain Relief
Topical Anesthetics
Use of topical anesthetics to relieve pain from ulcerative stomatitis and other oral lesions.
Systemic Pain Relief
Over-the-counter pain relievers, such as acetaminophen or ibuprofen, can help reduce fever and alleviate pain.
Hydration and Nutrition
Ensuring adequate hydration and nutrition is critical, especially for young children who may struggle with eating and drinking due to oral pain. Recommendations include:
- Soft Diet
- Hydration
Soft Diet
Providing a soft diet that is easier to chew and swallow, such as soups, smoothies, and mashed vegetables.
Hydration
Encouraging regular fluid intake to prevent dehydration.
Post-Measles Dental Care
After recovering from measles, patients should receive a comprehensive dental evaluation to address any oral health issues that may have arisen during the infection. Post-measles dental care may include:
- Dental Cleaning
- Restoration of Dental Health
- Education on Oral Hygiene
Dental Cleaning
A professional dental cleaning to remove plaque and tartar buildup that may have accumulated during the illness. This helps to reduce the risk of dental caries and gum disease.
Restoration of Dental Health
Any cavities or dental issues identified during the post-measles evaluation should be promptly addressed. This may involve fillings, extractions, or other restorative procedures to ensure optimal oral health.
Education on Oral Hygiene
Providing education on proper oral hygiene practices to prevent future dental problems. This includes guidance on brushing, flossing, and regular dental check-ups.
Frequently Asked Questions (FAQs)
How many days does measles last?
Measles symptoms typically last about 7 to 10 days. The initial phase, known as the incubation period, lasts about 10-14 days without symptoms. This is followed by the prodromal stage, where flu-like symptoms such as fever, cough, runny nose, and conjunctivitis appear. Around the third to fourth day, a characteristic red rash appears, usually starting on the face and then spreading to the rest of the body. The rash lasts about a week before fading as the body recovers.
Do you have to isolate with measles?
Yes, isolation is crucial to prevent the spread of the measles virus, which is highly contagious. Infected individuals should stay home and avoid contact with others for at least four days after the rash appears. If possible, they should stay in a well-ventilated room separate from other family members. Schools and workplaces should also be informed so that proper precautions can be taken to prevent further outbreaks.
What not to do during measles?
During measles, avoid contact with others to prevent transmission. Strenuous physical activities should be avoided, as the body needs rest to recover. Exposure to bright light can cause eye discomfort due to conjunctivitis, so it may be helpful to stay in a dimly lit room. Scratching the rash should also be avoided to prevent infections and scarring. Additionally, steer clear of unhealthy foods, alcohol, and smoking, as these can weaken the immune system and prolong recovery.
How to treat measles in a child?
There is no specific antiviral treatment for measles, so care focuses on relieving symptoms. Make sure the child gets plenty of rest and drinks fluids to prevent dehydration. Fever reducers such as acetaminophen or ibuprofen can help with fever and discomfort (avoid aspirin in children). If a doctor prescribes vitamin A supplements, they should be given as it has been shown to reduce the severity of measles symptoms. It is also important to monitor for complications such as pneumonia, ear infections, or encephalitis and seek medical attention if symptoms worsen.
Is it safe to be around someone with measles?
No, measles is extremely contagious. The virus spreads through respiratory droplets when an infected person coughs or sneezes, and it can remain in the air or on surfaces for several hours. If you are not vaccinated or have not previously had measles, avoid close contact with infected individuals. People with weakened immune systems, pregnant women, and infants are particularly vulnerable to severe complications and should take extra precautions.
Do you have to stay in a dark room with measles?
Staying in a dark room is not a strict requirement, but it can help relieve discomfort. Many people with measles experience photophobia (sensitivity to light) due to eye inflammation (conjunctivitis). Staying in a dimly lit or darkened room may help reduce eye strain and discomfort.
How long is measles contagious?
Measles is contagious from about four days before the rash appears to four days after it erupts. During this period, the virus is actively spreading through respiratory droplets. People who have been exposed to the virus but are not vaccinated may develop symptoms within 7 to 21 days.
What can be mistaken for measles?
Several conditions can resemble measles, including rubella (German measles), roseola, scarlet fever, and allergic reactions. Other viral infections that cause rashes, such as fifth disease and hand-foot-and-mouth disease, can also be mistaken for measles. A doctor can confirm a measles diagnosis through symptoms, medical history, and laboratory tests.
What are the 3 C’s of the measles?
The 3 C’s of measles are:
- Cough – a persistent, dry cough
- Coryza – runny nose and nasal congestion
- Conjunctivitis – red, watery, and inflamed eyes These symptoms appear early in the illness and are often accompanied by fever.
How do you confirm if I have measles?
A measles diagnosis is confirmed based on symptoms, a physical examination, and laboratory tests. The presence of Koplik spots (small white spots inside the mouth) is a strong indicator. A blood test, throat swab, or urine sample can be analyzed to detect the measles virus or measles-specific antibodies.
Can I kiss someone with measles?
No, kissing someone with measles is highly likely to transmit the virus. Measles spreads through saliva and respiratory droplets, making direct contact a significant risk.
Can I get measles twice?
No, once you have had measles, your body develops lifelong immunity. However, in rare cases, individuals with compromised immune systems may experience a second infection. Vaccination remains the best preventive measure.
What are 5 symptoms of measles?
Common symptoms of measles include:
- High fever (often above 101°F or 38.3°C)
- Persistent cough
- Runny nose (coryza)
- Red, inflamed eyes (conjunctivitis)
- Red rash that starts on the face and spreads to the rest of the body
What is the 3-day measles?
The 3-day measles, also known as rubella or German measles, is a different viral infection that causes a mild rash and typically lasts for about three days. Unlike measles, rubella is generally less severe, though it can be dangerous for pregnant women as it can cause congenital rubella syndrome in unborn babies.
What food is not allowed in measles?
Certain foods can worsen symptoms or slow recovery. Avoid processed foods, sugary snacks, and dairy products if they increase mucus production. Greasy, fried, or spicy foods should also be avoided as they can cause digestive discomfort. Instead, focus on easily digestible, nutrient-rich foods such as fruits, vegetables, soups, and whole grains to support the immune system and promote healing.
Conclusion
Measles remains a significant global health challenge, but it is a preventable disease. The history of measles, from its first descriptions to the development of the vaccine, highlights the remarkable progress made in controlling this disease. However, the recent resurgence of measles in various parts of the world underscores the importance of maintaining high vaccination coverage and addressing the challenges that hinder elimination efforts.
By strengthening health systems, addressing vaccine hesitancy, enhancing surveillance and outbreak response, reaching underserved populations, and fostering global collaboration, we can move closer to a world free of measles. The success of measles elimination programs in several regions demonstrates that with sustained commitment and effort, we can protect future generations from this preventable disease.
Measles, while primarily known for its systemic symptoms, has significant implications for oral health. From the characteristic Koplik’s spots to secondary infections and the impact on oral hygiene, measles can lead to various dental concerns. Effective infection control measures, pain management, and post-measles dental care are essential to address these issues and ensure optimal oral health for patients. Ultimately, prevention through vaccination remains the most powerful tool in combating measles and its associated dental concerns.


kim
27 August 2024With herbal solution I Got rid of Hsv after suffering for 6 years. Via___Robi nsonbuc ler( gm a il..C om ),,,,,,,,