Dental implants have revolutionized modern dentistry, providing a long term solution for the replacement of missing teeth. Despite their high success rates and functional benefits, dental implants are not devoid of complications. One of the most critical and widely studied issues is marginal bone loss (MBL), which can significantly affect the longevity and success of dental implants. This article delves into the concept of marginal bone loss, its etiological factors, diagnostic approaches, clinical implications, prevention strategies, and current research trends, providing a comprehensive understanding of this crucial phenomenon.
Table of Contents
ToggleDefinition and Importance of Marginal Bone Loss
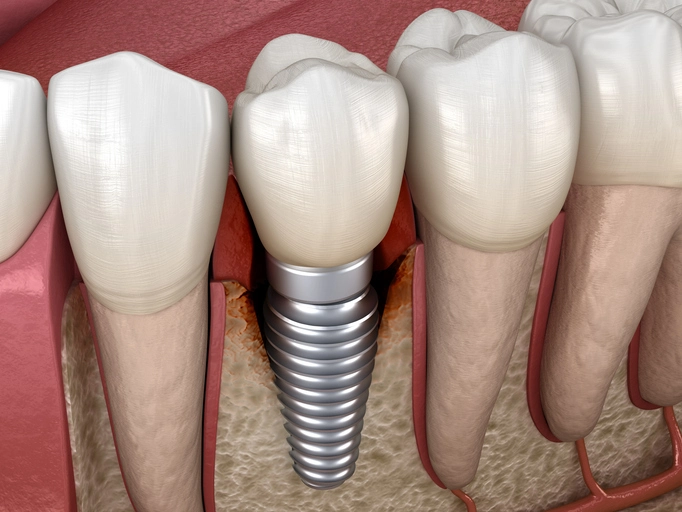
Marginal bone loss (MBL) refers to the vertical resorption of alveolar bone that occurs at the marginal or crestal level around a dental implant. It is a complex biological phenomenon and one of the key indicators of peri-implant health. This bone remodeling process begins shortly after implant placement and is influenced by a combination of mechanical, microbial, and host-related factors.
Clinically, it is generally accepted that some degree of bone remodeling is expected and physiological. Research suggests that up to 1.5 mm of marginal bone loss during the first year of function, followed by an annual loss of 0.2 mm, can be considered within normal limits. However, when this loss becomes excessive or progresses beyond the expected physiological limits, it is termed pathological and is a cause for concern.
The importance of monitoring and understanding marginal bone loss lies in its direct impact on the long-term stability and success of dental implants. MBL can compromise the osseointegration of the implant, which is the direct structural and functional connection between living bone and the surface of the implant. Significant bone loss can expose implant threads, reduce bone support, and ultimately lead to implant failure if not addressed timely.
Furthermore, MBL can have substantial aesthetic consequences, particularly in the anterior region of the mouth where bone and soft tissue architecture play a crucial role in the final appearance of the restoration. Gingival recession and exposure of implant components can lead to unsatisfactory outcomes for patients, affecting both their self-esteem and satisfaction with treatment.
Therefore, marginal bone loss is not merely a radiographic observation but a multifactorial clinical indicator that necessitates comprehensive evaluation. Understanding its underlying causes, monitoring its progression, and implementing strategies for its prevention and management are fundamental for achieving long-term implant success and maintaining patient health and satisfaction.
Etiology of Marginal Bone Loss
Understanding the multifactorial causes of marginal bone loss is essential for effective prevention and management. The following are key etiological factors, elaborated to reflect their complex interrelationships and clinical significance:
- Surgical Trauma
- Microgap and Bacterial Infiltration
- Biomechanical Overload
- Peri-implantitis
- Host Factors
- Prosthetic Design and Misfit
- Soft Tissue Biotype and Mucosal Seal Integrity
- Implant Surface and Design Characteristics
Surgical Trauma
Trauma during implant placement is a primary cause of early marginal bone loss. Factors such as overheating of the bone (temperatures exceeding 47°C), excessive drilling force, and improper osteotomy techniques can result in bone necrosis. Inadequate irrigation and poor surgical visibility further exacerbate this issue. Suboptimal implant angulation or placement depth may also contribute to stress concentrations, which can initiate bone resorption.
Microgap and Bacterial Infiltration
The microgap at the implant-abutment junction is a critical site for microbial colonization. Despite technological advancements, this microscopic space can harbor anaerobic bacteria, leading to the formation of biofilms. These biofilms trigger an inflammatory response in peri-implant tissues, which in turn stimulates osteoclastic activity and bone degradation. The extent of microbial infiltration is influenced by the precision of the implant abutment fit and the type of connection system used (internal vs. external).
Biomechanical Overload
Excessive or improperly distributed occlusal forces can result in biomechanical overload, especially in cases of bruxism or improperly balanced prosthetics. This overload causes micromovement of the implant within the bone, disrupting the delicate balance between bone resorption and formation. High stress concentrations are particularly detrimental in the crestal region, where they can lead to early bone loss and compromise osseointegration.
Peri-implantitis
Peri-implantitis is a progressive inflammatory condition characterized by the loss of supporting bone around an osseointegrated implant. It is typically associated with poor plaque control, inadequate maintenance, and bacterial biofilm accumulation. Unlike mucositis, which is limited to soft tissue inflammation, peri-implantitis involves both soft and hard tissues and can lead to rapid and severe bone loss if untreated. Risk factors such as smoking, history of periodontitis, and substandard oral hygiene significantly increase susceptibility to peri-implantitis.
Host Factors
Systemic health plays a substantial role in determining bone healing and remodeling capacity. Chronic conditions like uncontrolled diabetes mellitus impair microcirculation and neutrophil function, delaying wound healing and increasing the risk of infection. Osteoporosis alters bone density and architecture, making it more susceptible to resorption. Additionally, lifestyle factors such as smoking reduce oxygen supply to tissues, inhibit fibroblast function, and impair angiogenesis, all of which contribute to increased bone loss.
Prosthetic Design and Misfit
The design and fit of prosthetic components significantly influence stress distribution across the implant system. A poor prosthetic fit can lead to micromotion at the interface, disrupting osseointegration. Moreover, cantilever extensions and non-axial loading configurations create lever forces that exacerbate marginal bone stress. The choice of materials, type of connection, and occlusal scheme should all be carefully considered to minimize mechanical complications and subsequent bone loss.
Soft Tissue Biotype and Mucosal Seal Integrity
A thin mucosal biotype is less resilient to mechanical and inflammatory challenges and may allow easier penetration of bacterial products to the bone level. Additionally, an inadequate or unstable mucosal seal can facilitate microbial ingress, accelerating crestal bone loss. Preservation of soft tissue volume and quality through careful surgical and prosthetic planning is vital to maintaining marginal bone levels.
Implant Surface and Design Characteristics
Implant macrodesign (shape, thread pattern, diameter) and surface topography influence the initial healing response and long-term bone maintenance. Rough-surfaced implants generally show better osseointegration, but may also be more susceptible to biofilm retention if peri-implant hygiene is compromised. Platform switching and tapered designs have been associated with reduced crestal bone loss by improving force distribution and sealing the microgap interface.
Diagnostic Approaches
Early and accurate diagnosis of marginal bone loss is crucial for timely intervention. Several diagnostic tools and techniques are employed:
1. Radiographic Evaluation
Periapical radiographs and cone-beam computed tomography (CBCT) are commonly used to assess bone levels. Standardized radiographs at regular intervals help in monitoring bone changes over time.
2. Clinical Examination
Probing depths, bleeding on probing, and the presence of suppuration are clinical indicators of peri-implant inflammation that may be associated with bone loss.
3. Digital Technologies
Advanced imaging software and digital scanning can provide three dimensional analysis and more precise quantification of bone changes.
Clinical Implications
Marginal bone loss has far-reaching clinical implications that can compromise the function, longevity, and aesthetic outcomes of dental implant therapy. Recognizing these implications is critical for timely intervention and patient satisfaction.
- Aesthetic Complications
- Compromised Implant Stability
- Increased Risk of Infection and Inflammation
- Prosthetic Complications
- Patient Dissatisfaction
- Complexity in Maintenance
Aesthetic Complications
In esthetically sensitive areas, such as the anterior maxilla, even minor bone loss can lead to significant visual issues. This includes soft tissue recession, which exposes implant or abutment components, and results in poor aesthetic integration of the implant with surrounding natural dentition.
Compromised Implant Stability
As bone levels recede, the mechanical stability and support for the implant are reduced. This compromises the functional integrity of the implant, increasing the likelihood of micro-movements that may disrupt osseointegration and lead to progressive bone loss or outright implant failure.
Increased Risk of Infection and Inflammation
Bone loss is often associated with peri-implant mucositis or peri-implantitis. These inflammatory conditions not only threaten the survival of the implant but also require complex and sometimes invasive treatments.
Prosthetic Complications
Marginal bone loss may necessitate modifications or replacements of prosthetic components. Misalignment, reduced support, and exposure of rough implant surfaces can impair function and hygiene, leading to further biological complications.
Patient Dissatisfaction
The combination of functional impairments and aesthetic deficits due to bone loss can significantly reduce patient satisfaction. This may lead to additional clinical visits, increased treatment costs, and reduced overall trust in implant therapy.
Complexity in Maintenance
With exposed threads and deeper pockets, routine hygiene becomes challenging. This increases the need for professional maintenance and potentially surgical correction, placing additional long-term demands on both patient and provider.
Understanding these clinical implications underscores the importance of early diagnosis, preventive planning, and tailored maintenance protocols to ensure the long-term success and patient-centered outcomes of dental implant therapy.
Prevention Strategies
Preventing marginal bone loss involves a multi-pronged approach that addresses surgical technique, prosthetic accuracy, patient risk factors, and long-term care:
1. Surgical Best Practices
- Utilize atraumatic surgical techniques to preserve bone integrity.
- Ensure adequate irrigation during drilling to prevent thermal injury.
- Position implants correctly with sufficient bone volume around the fixture.
- Consider flapless or minimally invasive approaches where feasible to preserve soft and hard tissue.
2. Implant Design Innovations
- Choose implants with platform switching to reduce stress on crestal bone.
- Use conical and internal connections to minimize micro-movement and bacterial leakage.
- Select surface-treated implants to enhance osseointegration and bone stability.
3. Prosthetic Considerations
- Ensure a precise passive fit of the prosthesis to avoid undue stress on the implant.
- Design occlusal schemes to distribute forces evenly and avoid overloading.
- Avoid cantilevered extensions and non-axial load configurations that increase mechanical complications.
4. Maintenance Protocols
- Implement a structured follow-up schedule with radiographic evaluations and professional cleanings.
- Educate patients on proper oral hygiene practices around implants, including the use of interdental brushes and antimicrobial mouth rinses.
- Monitor for early signs of inflammation and intervene promptly.
5. Risk Factor Management
- Screen patients thoroughly for systemic conditions that may affect bone health, such as diabetes and osteoporosis.
- Encourage smoking cessation programs and provide support.
- Address parafunctional habits such as bruxism with night guards or behavior modification strategies.
A comprehensive preventive strategy is essential not only to maintain implant success but also to enhance patient satisfaction and reduce long-term treatment costs.
Treatment Modalities for Marginal Bone Loss
Once MBL is diagnosed, treatment depends on the severity and underlying cause. The therapeutic approach should be multifaceted, targeting the resolution of infection, restoration of hard and soft tissue structures, and prevention of recurrence.
Non-Surgical Therapy
Non-surgical treatments are often the first line of intervention for early or mild bone loss:
- Mechanical Debridement: Removal of bacterial biofilm and calculus from the implant surface using plastic, titanium, or ultrasonic instruments.
- Antimicrobial Rinses: Chlorhexidine mouthwash or hydrogen peroxide may help reduce microbial load.
- Systemic and Local Antibiotics: These are used to control infection, especially when peri-implantitis is present.
- Photodynamic Therapy: Use of a light-activated photosensitizer to destroy bacterial cells without harming the implant or surrounding tissues.
Surgical Interventions
Surgical treatment is indicated when non-surgical methods are insufficient or bone loss is advanced:
- Open Flap Debridement: Accessing the affected area through a flap to clean the implant surface thoroughly.
- Guided Bone Regeneration (GBR): Placement of barrier membranes and bone grafts to encourage bone regrowth around the implant.
- Apically Positioned Flaps: In resective therapy, soft tissue is repositioned to eliminate pockets and improve hygiene access.
- Use of Biomaterials: Bone substitutes (xenografts, allografts, or synthetic materials) and biologics like enamel matrix derivative (EMD) to promote regeneration.
Laser Therapy
Laser-assisted therapy is gaining popularity due to its minimally invasive nature:
- Er:YAG Laser: Effective for decontaminating implant surfaces and removing granulation tissue.
- Nd:YAG Laser: Useful for coagulation and bacterial reduction in deeper pockets.
- Combination Protocols: Some clinicians combine lasers with mechanical debridement and antibiotics for enhanced outcomes.
Explantation and Reimplantation
In cases where the implant is no longer viable:
- Explantation: The failed implant is removed, and the site is thoroughly debrided.
- Site Preservation: Bone grafting is often performed immediately to preserve alveolar ridge structure.
- Reimplantation: A new implant may be placed after sufficient healing, often requiring months of follow-up and potential reaugmentation.
The choice of treatment must be patient-specific, considering the severity of bone loss, implant design, systemic health, and compliance with oral hygiene. Long-term follow-up and supportive therapy are essential to prevent recurrence and ensure successful outcomes.