Kidney diseases, encompassing a range of conditions that impair the function of the kidneys, have significant implications not only for general health but also for dental care. The interconnectedness of bodily systems means that chronic kidney disease (CKD) and other renal issues can have profound effects on oral health, necessitating specialized care from dental professionals. This article explores the nature of kidney diseases, their impact on oral health, and the importance of integrating nephrology with dentistry to ensure comprehensive patient care.
Table of Contents
ToggleUnderstanding Kidney Diseases
The kidneys, two bean-shaped organs located on either side of the spine, are crucial for filtering waste products and excess fluids from the blood, which are then excreted as urine. They also play a vital role in maintaining electrolyte balance, regulating blood pressure, and producing hormones that influence red blood cell production and bone health. Kidney diseases can disrupt these functions, leading to a cascade of health issues.
Chronic Kidney Disease (CKD)
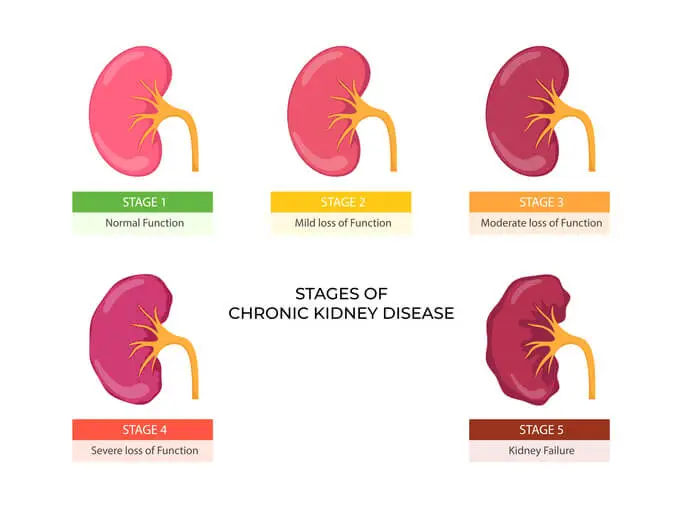
CKD is the most common form of kidney disease, characterized by a gradual loss of kidney function over months or years. The leading causes of CKD are diabetes and hypertension, accounting for about two-thirds of cases. Other causes include glomerulonephritis, polycystic kidney disease, and prolonged obstruction of the urinary tract. CKD is typically classified into five stages, based on the glomerular filtration rate (GFR), with stage 5 being end-stage renal disease (ESRD), where dialysis or a kidney transplant becomes necessary.
Acute Kidney Injury (AKI)
AKI is a sudden decline in kidney function, often resulting from severe illness, injury, or complications from surgery. Unlike CKD, which is gradual, AKI can occur within hours or days and can be reversible if treated promptly. Common causes include severe infections, sepsis, dehydration, and exposure to nephrotoxic drugs or contrast agents used in imaging studies.
Oral Health Implications of Kidney Diseases
The relationship between kidney diseases and oral health is bidirectional. Poor oral health can contribute to the progression of kidney diseases, and conversely, kidney diseases can lead to various oral manifestations.
Oral manifestations in CKD are:
- Xerostomia (Dry Mouth)
- Uremic Stomatitis
- Periodontal Disease
- Oral Infections
- Altered Taste Sensation
- Bone Metabolism Disorders
Xerostomia (Dry Mouth)
Reduced salivary flow is common in CKD patients, often due to medication side effects or fluid restrictions. Saliva is crucial for maintaining oral health by neutralizing acids and washing away food particles. Xerostomia increases the risk of dental caries, oral infections, and difficulties in speaking and swallowing.
Uremic Stomatitis
This condition arises from the accumulation of urea in the blood (uremia) and its subsequent breakdown to ammonia in the oral cavity, causing mucosal irritation and ulcers. It is more prevalent in advanced CKD and ESRD patients.
Periodontal Disease
CKD patients are at a higher risk for periodontal disease due to impaired immune responses and altered inflammatory processes. Periodontal disease, characterized by inflammation and destruction of the supporting structures of teeth, can exacerbate systemic inflammation and contribute to the progression of CKD.
Oral Infections
Due to compromised immunity, CKD patients are more susceptible to oral infections, including candidiasis and bacterial infections. These infections can complicate overall health and potentially lead to systemic infections.
Altered Taste Sensation
CKD can lead to dysgeusia, a distortion of the sense of taste, which affects nutritional intake and overall quality of life. Patients often report metallic or bitter tastes.
Bone Metabolism Disorders
CKD impacts the regulation of calcium, phosphate, and vitamin D, leading to renal osteodystrophy. This condition affects jawbones, increasing the risk of bone fractures and impacting the success of dental implants.
Dental Management of Patients with Kidney Diseases
The complexities of kidney diseases require dental professionals to adopt tailored approaches when treating affected patients. A comprehensive understanding of the patient’s medical history, current medications, and renal function status is crucial.
Pre-Treatment Considerations
- Medical Consultation
- Medication Review
- Timing of Appointments
- Antibiotic Prophylaxis
Medical Consultation
Coordination with the patient’s nephrologist or primary care physician is essential to understand the extent of the kidney disease, current treatment regimens, and any necessary modifications to dental care plans.
Medication Review
CKD patients often take multiple medications, including antihypertensives, phosphate binders, and immunosuppressants. Some of these drugs can have oral side effects or interact with dental medications. For instance, nonsteroidal anti-inflammatory drugs (NSAIDs) should be avoided as they can worsen renal function.
Timing of Appointments
For patients on dialysis, dental procedures should ideally be scheduled on non-dialysis days to avoid complications related to heparin (a blood thinner used during dialysis). Morning appointments are often preferred due to better patient energy levels and reduced risk of bleeding.
Antibiotic Prophylaxis
Patients with certain conditions, such as those with indwelling catheters for dialysis, may require antibiotic prophylaxis to prevent infective endocarditis. The decision should be made in consultation with the nephrologist.
Intra-Treatment Considerations
- Anesthesia and Pain Management
- Bleeding Risks
- Infection Control
Anesthesia and Pain Management
Local anesthetics are generally safe, but doses may need adjustment based on renal function. Avoidance of drugs metabolized by the kidneys is crucial to prevent toxicity. For pain management, acetaminophen is preferred over NSAIDs.
Bleeding Risks
CKD patients often have platelet dysfunction and may be on anticoagulants, increasing the risk of bleeding. Local hemostatic measures and careful surgical technique are vital.
Infection Control
Enhanced infection control measures are necessary due to the increased susceptibility to infections. This includes meticulous aseptic techniques and possibly the use of chlorhexidine mouthwash to reduce microbial load.
Post-Treatment Considerations
- Follow-Up Care
- Oral Hygiene Education
- Dietary Advice
Follow-Up Care
Regular follow-up is essential to monitor healing and manage any complications. This is particularly important for surgical procedures and in patients with diabetes or other comorbidities.
Oral Hygiene Education
CKD patients should receive tailored oral hygiene instructions to manage xerostomia and prevent periodontal disease. This may include the use of saliva substitutes, fluoride treatments, and antimicrobial mouth rinses.
Dietary Advice
Collaboration with dietitians can help manage dietary restrictions that impact oral health, such as phosphate and potassium intake.
The Role of the Dental Professional in Managing Kidney Diseases
Dental professionals play a critical role in the multidisciplinary care of patients with kidney diseases. By recognizing the oral manifestations of CKD and understanding the systemic implications, dentists can contribute to the early detection and management of renal issues.
Screening and Early Detection
Regular dental visits provide an opportunity for early detection of systemic conditions, including kidney diseases. Dentists should be vigilant for signs such as xerostomia, uremic breath, and mucosal lesions, which may warrant further medical evaluation.
Patient Education and Advocacy
Educating patients about the link between oral health and kidney disease is vital. Dentists can advocate for regular medical check-ups and collaborate with healthcare providers to ensure integrated care. This holistic approach can improve patient outcomes and quality of life.
Frequently Asked Questions (FAQs)
What is the dental relevance of kidney disease?
Kidney disease has a significant impact on oral health. Since the kidneys help regulate calcium, phosphorus, and vitamin D levels, their dysfunction can lead to bone-related issues, including jawbone deterioration and delayed tooth eruption in children. Furthermore, patients with kidney disease often experience dry mouth (xerostomia), gum disease (periodontitis), and bad breath (uremic fetor) due to the accumulation of toxins in the body. Dental professionals must take special precautions when treating patients with kidney disease, as they may have an increased risk of infection, excessive bleeding, and delayed healing after procedures.
Can kidney problems cause teeth problems?
Yes, kidney disease can indirectly and directly lead to various dental problems. Some of the effects include:
- Bone loss and weak teeth: Kidney disease can cause imbalances in calcium and phosphorus, leading to brittle bones and weakened tooth structures.
- Gum disease (periodontitis): Patients with chronic kidney disease (CKD) have a higher risk of developing gum disease due to their compromised immune system and inflammatory response.
- Enamel defects: In children with kidney disease, improper mineralization of teeth can lead to thin or soft enamel, making them more susceptible to cavities.
- Dry mouth (xerostomia): Many kidney patients suffer from dry mouth due to reduced saliva production, which increases the risk of cavities, bad breath, and oral infections.
What are the dental precautions for kidney disease?
Patients with kidney disease require special dental care to minimize risks. Some important precautions include:
- Timing of treatment: If the patient is on dialysis, dental procedures should be scheduled on non-dialysis days to avoid excessive bleeding and complications.
- Antibiotic prophylaxis: Some patients with kidney disease may require antibiotics before dental procedures to prevent infections, especially those with dialysis access devices or weakened immune systems.
- Avoiding certain medications: NSAIDs (such as ibuprofen) should be avoided as they can worsen kidney function. Some antibiotics (like tetracyclines and aminoglycosides) should also be used with caution.
- Monitoring bleeding risk: Since kidney disease can affect platelet function and clotting, dentists should assess bleeding risk before performing extractions or surgeries.
- Oral hygiene education: Patients should be advised to maintain excellent oral hygiene to prevent gum disease and infections.
Why is kidney disease important?
Kidney disease is crucial because it affects multiple body systems and can lead to severe complications, including high blood pressure, anemia, bone disease, and cardiovascular problems. It also impacts oral health, leading to increased risk of infections, delayed healing, and changes in the jawbone structure. Proper management of kidney disease is essential to prevent life-threatening complications and maintain overall well-being.
What is the role of the kidneys in teeth and bone development?
The kidneys play a vital role in maintaining strong bones and teeth by:
- Regulating calcium and phosphorus levels: These minerals are essential for strong teeth and bones. Kidney dysfunction can lead to demineralization, making teeth weaker.
- Activating vitamin D: The kidneys help convert vitamin D into its active form, which is necessary for calcium absorption. Without sufficient vitamin D, bones and teeth become fragile.
- Maintaining acid-base balance: Kidney disease can lead to metabolic acidosis, which may cause demineralization of teeth and bones.
In children, chronic kidney disease (CKD) can lead to delayed or abnormal tooth development, increasing the risk of cavities and misaligned teeth.
What is the most common oral manifestation of kidney disease?
The most common oral signs and symptoms of kidney disease include:
- Dry mouth (xerostomia): Reduced saliva production increases the risk of cavities and infections.
- Uremic fetor (bad breath): A distinctive ammonia-like odor caused by the buildup of urea in the blood, which breaks down into ammonia in the mouth.
- Mouth ulcers: Painful sores in the mouth due to a weakened immune system and toxin buildup.
- Gum disease (periodontitis): More severe in kidney patients due to immune dysfunction.
- Renal osteodystrophy: Bone disease related to kidney failure, which can cause jawbone loss and loose teeth.
Can a kidney infection affect your mouth?
Yes, kidney infections (pyelonephritis) can indirectly affect the mouth. When the kidneys are unable to filter toxins effectively, waste products accumulate in the blood, leading to:
- Bad breath and metallic taste: Due to the buildup of urea in the bloodstream.
- Weakened immune response: Making the patient more susceptible to oral infections like gum disease and oral thrush.
- Dry mouth: As a result of dehydration and certain medications used to treat kidney infections.
What organs affect teeth?
Several organs play a role in maintaining healthy teeth, including:
- Kidneys: Regulate minerals needed for strong teeth and bones.
- Liver: Helps with blood clotting and detoxification, which can impact healing after dental procedures.
- Heart: Poor circulation can affect gum health, and heart conditions are linked to gum disease.
- Endocrine system: Disorders such as diabetes and thyroid disease can lead to dry mouth, delayed healing, and increased infection risk.
Why is tooth extraction contraindicated in renal failure?
Tooth extraction may be risky in patients with advanced kidney disease due to:
- Increased bleeding risk: Due to platelet dysfunction and blood-thinning medications.
- Higher risk of infection: The immune system is often weakened, making infections more likely.
- Delayed healing: Due to metabolic imbalances and poor bone health.
- Risk of medication complications: Some painkillers and anesthetics used in dentistry need to be adjusted for kidney patients.
Dentists must collaborate with the patient’s nephrologist before performing extractions.
What dental anesthesia is used for kidney disease?
Local anesthetics such as lidocaine without epinephrine are commonly used, as epinephrine may cause blood pressure fluctuations. Dosage adjustments may be needed for patients with severe kidney disease. Dentists should also avoid general anesthesia unless medically necessary and supervised by a specialist.
What are the complications of extraction in dentistry?
Common complications of dental extractions in kidney patients include:
- Prolonged bleeding due to clotting abnormalities.
- Delayed healing due to metabolic and mineral imbalances.
- Infection risk due to immune suppression.
- Dry socket (alveolar osteitis) due to poor blood supply and healing issues.
- Drug interactions with medications such as anticoagulants and immunosuppressants.
What can kidney patients take for a toothache?
Pain management in kidney patients must be carefully planned:
- Acetaminophen (paracetamol) is the safest over-the-counter painkiller for mild to moderate pain.
- Opioids may be prescribed for severe pain but must be used cautiously.
- Avoid NSAIDs (like ibuprofen, naproxen, and aspirin), as they can worsen kidney function.
- Topical anesthetics (such as benzocaine) may provide temporary relief.
- Saltwater rinses and cold compresses can help manage pain and inflammation naturally.
For severe or persistent tooth pain, a kidney patient should consult a dentist or nephrologist before taking any medication.
Conclusion
Kidney diseases, particularly CKD, present significant challenges to both general and oral health. The interplay between renal function and oral health necessitates a comprehensive and collaborative approach to patient care. Dental professionals must be well-versed in the oral manifestations of kidney diseases and adept at managing the unique needs of these patients. Through interdisciplinary collaboration, education, and tailored dental care, the impact of kidney diseases on oral health can be mitigated, leading to improved overall health outcomes for affected individuals.

