Hypothyroidism, a common endocrine disorder, occurs when the thyroid gland fails to produce sufficient amounts of thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3). These hormones play a crucial role in regulating the body’s metabolism, growth, and development. Hypothyroidism can significantly impact various systems in the body, including the cardiovascular, nervous, and musculoskeletal systems. Consequently, this condition can also influence dental health and patient management in a dental setting.
This article will delve into the pathophysiology of hypothyroidism, its oral manifestations, and the essential considerations dental professionals should bear in mind when treating patients with this condition.
Table of Contents
TogglePathophysiology of Hypothyroidism
To understand the dental implications of hypothyroidism, it is crucial first to grasp the basics of thyroid hormone function. The thyroid gland, located in the neck, secretes thyroid hormones that are pivotal in regulating metabolism. These hormones influence nearly every tissue in the body, affecting heart rate, body temperature, and even how the body metabolizes nutrients.
In hypothyroidism, there is a deficiency of thyroid hormones, which can be primary (due to thyroid gland dysfunction) or secondary (due to pituitary or hypothalamic disorders). The most common cause of primary hypothyroidism is Hashimoto’s thyroiditis, an autoimmune condition where the immune system attacks the thyroid gland. Other causes include iodine deficiency, thyroid surgery, and radiation therapy.
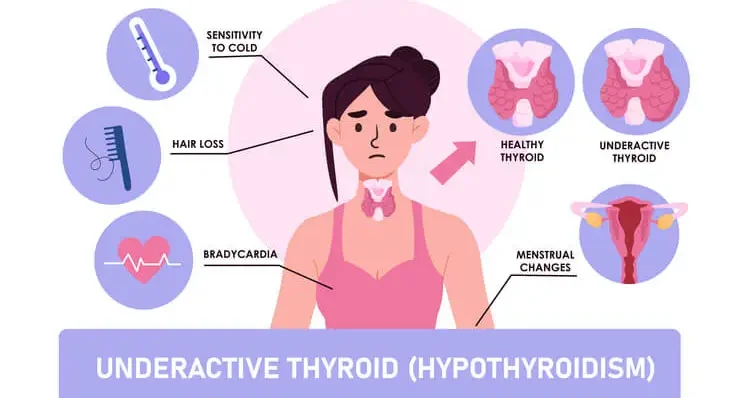
When thyroid hormone levels drop, the body’s metabolic processes slow down. This can lead to a wide range of symptoms, including fatigue, weight gain, cold intolerance, dry skin, constipation, and depression. From a dental perspective, hypothyroidism can lead to specific oral manifestations and complications, making it essential for dental professionals to recognize and manage these patients effectively.
Oral Manifestations of Hypothyroidism
Hypothyroidism can have a range of oral manifestations that may be evident during a dental examination. These manifestations can vary depending on the severity and duration of the hypothyroid state. Common oral symptoms and conditions associated with hypothyroidism include:
- Macroglossia (Enlarged Tongue)
- Delayed Dental Eruption
- Malocclusion
- Increased Risk of Caries
- Periodontal Disease
- Dysgeusia (Altered Taste Sensation)
- Glossitis
- Myxedema
Macroglossia (Enlarged Tongue)
One of the most noticeable oral signs of hypothyroidism is an enlarged tongue, known as macroglossia. The tongue may appear swollen and have scalloped edges due to indentation by the teeth. This can cause difficulties in speech, swallowing, and even breathing in severe cases.
Delayed Dental Eruption
In children with untreated or poorly managed hypothyroidism, dental development may be delayed. This can result in late eruption of both primary and permanent teeth, which can complicate orthodontic treatment planning.
Malocclusion
The altered growth and development of the jaws and dental arches in hypothyroid patients can lead to malocclusion. This may require orthodontic or surgical intervention to correct.
Increased Risk of Caries
Hypothyroidism can lead to dry mouth (xerostomia) due to reduced salivary gland function. Saliva plays a crucial role in protecting teeth from decay, and its reduction can increase the risk of dental caries.
Periodontal Disease
Hypothyroidism may be associated with an increased risk of periodontal (gum) disease. This is likely due to the immune system alterations that occur with thyroid dysfunction, which can affect the body’s ability to combat oral bacteria effectively.
Dysgeusia (Altered Taste Sensation)
Some hypothyroid patients report changes in taste, such as a metallic or salty taste in the mouth. This can affect appetite and nutrition, potentially leading to further complications.
Glossitis
Inflammation of the tongue, known as glossitis, can occur in hypothyroid patients. The tongue may appear red, smooth, and shiny due to atrophy of the papillae (small bumps on the tongue’s surface).
Myxedema
In severe cases of hypothyroidism, patients may develop myxedema, a condition characterized by the accumulation of mucopolysaccharides in the skin and other tissues. In the oral cavity, this can manifest as thickened, swollen lips and an enlarged, protruding tongue.
Considerations for Dental Management of Hypothyroid Patients
Given the various oral manifestations and systemic effects of hypothyroidism, dental professionals must take specific precautions when treating these patients. A thorough understanding of the patient’s medical history, current thyroid status, and medication regimen is essential. The following are key considerations for the dental management of hypothyroid patients:
- Medical History and Communication with Healthcare Providers
- Evaluation of Thyroid Function
- Stress Management and Sedation
- Local Anesthesia Considerations
- Management of Xerostomia and Caries Prevention
- Periodontal Care
- Dental Surgery and Myxedema Risk
- Orthodontic Treatment Considerations
- Emergency Preparedness
Medical History and Communication with Healthcare Providers
Before initiating dental treatment, it is crucial to obtain a comprehensive medical history from the patient. This should include information about the diagnosis, duration, and severity of hypothyroidism, as well as any medications being taken, such as levothyroxine. In some cases, it may be necessary to consult with the patient’s endocrinologist or primary care physician to ensure that the patient’s thyroid levels are well-controlled and to discuss any potential risks associated with dental procedures.
Evaluation of Thyroid Function
Dental professionals should be aware of the signs and symptoms of hypothyroidism, especially if the condition has not been diagnosed or is poorly controlled. If a patient presents with symptoms suggestive of hypothyroidism, such as fatigue, weight gain, and cold intolerance, referral to a physician for evaluation and thyroid function testing (e.g., serum TSH, T4 levels) is recommended before proceeding with elective dental treatment.
Stress Management and Sedation
Hypothyroid patients may have a diminished ability to tolerate stress due to their reduced metabolic rate and cardiovascular complications. This can increase the risk of adverse events during dental procedures, such as hypertension, bradycardia, or even myxedema coma, a life-threatening condition. Therefore, stress management techniques, such as the use of anxiolytics, sedation, or shorter appointment durations, may be beneficial. However, sedatives and anesthetic agents should be used with caution, as hypothyroid patients may be more sensitive to these medications.
Local Anesthesia Considerations
When administering local anesthesia to hypothyroid patients, it is important to consider their cardiovascular status. Epinephrine, commonly used in local anesthetics, can exacerbate cardiovascular issues in hypothyroid patients, such as tachycardia or hypertension. Therefore, the use of low-dose epinephrine or epinephrine-free anesthetics should be considered, particularly in patients with severe hypothyroidism or those with a history of cardiovascular disease.
Management of Xerostomia and Caries Prevention
Xerostomia, or dry mouth, is a common complaint among hypothyroid patients due to reduced salivary gland function. This can increase the risk of dental caries, oral infections, and difficulties with speech and swallowing. Dental professionals should educate patients about the importance of maintaining good oral hygiene and recommend fluoride treatments, saliva substitutes, or sugar-free chewing gum to stimulate saliva production. Regular dental check-ups are essential for monitoring oral health and preventing complications.
Periodontal Care
As hypothyroidism may increase the risk of periodontal disease, dental professionals should closely monitor the periodontal health of these patients. This includes performing thorough periodontal examinations, providing professional cleanings, and educating patients about the importance of proper oral hygiene practices at home. In some cases, adjunctive therapies, such as antimicrobial rinses or systemic antibiotics, may be necessary to manage periodontal infections effectively.
Dental Surgery and Myxedema Risk
In patients with severe, untreated hypothyroidism, there is a risk of precipitating myxedema coma during or after dental surgery. This life-threatening condition is characterized by extreme hypothyroidism, hypothermia, and altered mental status, and it requires immediate medical intervention. Therefore, elective dental surgeries should be postponed until the patient’s thyroid function is stabilized. For urgent dental procedures, hospitalization and close monitoring may be necessary.
Orthodontic Treatment Considerations
For children and adolescents with hypothyroidism, orthodontic treatment may be complicated by delayed dental eruption, malocclusion, and altered craniofacial growth. Dental professionals should collaborate with endocrinologists to ensure that the patient’s thyroid function is well-managed before initiating orthodontic treatment. Additionally, the timing and duration of orthodontic interventions may need to be adjusted based on the patient’s growth and development.
Emergency Preparedness
Dental professionals should be prepared to manage potential emergencies in hypothyroid patients, such as myxedema coma or cardiovascular events. This includes having emergency medications, such as intravenous corticosteroids, and supportive measures, such as oxygen and intravenous fluids, readily available in the dental office. A well-established emergency protocol and training for the dental team are essential for ensuring patient safety.
Frequently Asked Questions (FAQs)
What is the dental consideration of hypothyroidism?
Patients with hypothyroidism may experience delayed healing, increased sensitivity to medications, an increased risk of infections, and dry mouth, which can contribute to tooth decay and periodontal disease. Additionally, they may have a decreased metabolic rate, which can impact drug metabolism and increase the risk of complications during dental procedures. Dentists should assess thyroid function, review the patient’s medical history, and adjust treatment plans accordingly to ensure patient safety.
What are the complications of hypothyroidism in dentistry?
Hypothyroidism can lead to several complications in dental care, including delayed wound healing, an increased risk of oral infections such as candidiasis, excessive bleeding due to coagulation abnormalities, and heightened sensitivity to sedatives and anesthetics. Additionally, hypothyroid patients may experience macroglossia (enlarged tongue), which can impact speech, swallowing, and airway management during dental procedures.
What precautions should be taken in hypothyroidism?
Precautions include evaluating thyroid function before any invasive dental procedures, avoiding sedatives and opioids in untreated or severely hypothyroid patients to prevent respiratory depression, and ensuring proper post-operative care to reduce the risk of complications. Dentists should also monitor patients for signs of myxedema, a severe form of hypothyroidism that can lead to life-threatening complications. Patients should be encouraged to maintain good oral hygiene to prevent infections and dental issues associated with dry mouth.
Can you have dental anesthesia with hypothyroidism?
Yes, but careful consideration is required. Local anesthetics without vasoconstrictors (such as epinephrine) are preferred, especially in patients with severe hypothyroidism, as epinephrine can lead to cardiovascular instability. The dosage of anesthesia should be carefully monitored, and patients should be observed for prolonged recovery times due to their decreased metabolic rate. Collaboration with the patient’s primary care physician or endocrinologist may be necessary for safe management.
Why is local anesthesia contraindicated in hypothyroidism?
In severe or uncontrolled hypothyroidism, local anesthesia with epinephrine is contraindicated because it can lead to adverse cardiovascular effects, such as hypotension (low blood pressure), bradycardia (slow heart rate), and even cardiac arrest in extreme cases. Additionally, hypothyroid patients have a reduced metabolic rate, which can prolong the effects of anesthesia, leading to delayed recovery and potential complications.
What are the side effects of thyroid medication at the dentist?
Common thyroid medications, such as levothyroxine, can have side effects that may impact dental procedures. These include increased heart rate, nervousness, anxiety, dry mouth (xerostomia), and altered pain perception. Patients on thyroid replacement therapy may also have an increased sensitivity to catecholamines, which are present in local anesthetics with epinephrine, increasing the risk of hypertensive episodes or palpitations.
How does hypothyroidism affect anesthesia?
Hypothyroidism can lead to increased sensitivity to sedatives and anesthetics due to a slower metabolic rate. This can result in prolonged sedation, delayed emergence from anesthesia, and an increased risk of respiratory depression. It is essential to use the lowest effective dose of sedatives and closely monitor the patient’s vital signs during and after the procedure.
What is the most common complication of hypothyroidism?
One of the most serious complications of hypothyroidism is myxedema, a condition characterized by severe hypothyroidism that can lead to life-threatening symptoms such as hypothermia, bradycardia, and even myxedema coma. In dental settings, the most common concerns include excessive bleeding, prolonged healing, and increased risk of infections, all of which can complicate both routine and invasive procedures.
How does hypothyroidism affect the dental developmental pattern?
In children, hypothyroidism can cause delayed tooth eruption, enamel hypoplasia (defective enamel formation), and malocclusion due to altered craniofacial growth patterns. Additionally, these children may experience macroglossia (enlarged tongue), which can affect speech development and occlusion. Early diagnosis and treatment of hypothyroidism are essential to prevent long-term dental and orthodontic issues.
Conclusion
Hypothyroidism is a common endocrine disorder with significant implications for dental care. The oral manifestations of hypothyroidism, such as macroglossia, delayed dental eruption, and increased risk of caries and periodontal disease, necessitate a thorough understanding of the condition and its impact on dental treatment. Dental professionals must take into account the patient’s thyroid status, medication regimen, and potential complications when planning and delivering care.
Effective management of hypothyroid patients in the dental setting requires a multidisciplinary approach, involving communication with the patient’s healthcare providers, careful treatment planning, and vigilant monitoring for any signs of complications. By adopting these strategies, dental professionals can help ensure that patients with hypothyroidism receive safe and effective care, ultimately improving their oral health and overall well-being.

YouTube Downloader
27 August 2024Thank you for sharing this insightful article! I found the information really useful and thought-provoking. Your writing style is engaging, and it made the topic much easier to understand. Looking forward to reading more of your posts!