The article examines the clinical factors that influence the choice of cement used by dentists for single-unit crown restorations.
Methods
This study is part of research conducted by The National Dental Practice-Based Research Network, involving 202 dentists who recorded the clinical details of 3,468 single-unit crowns, including the type of cement used.
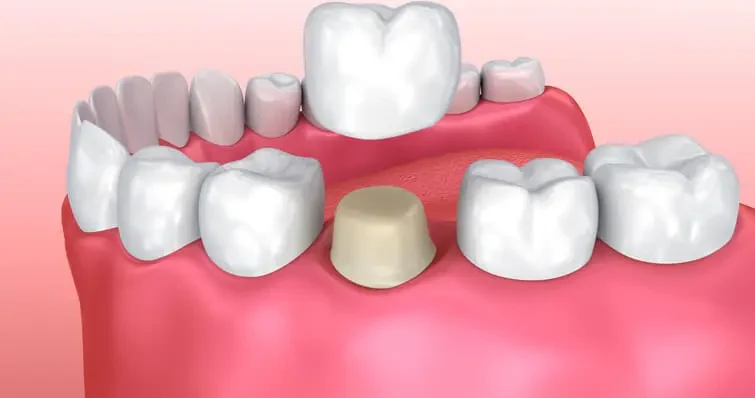
In dentistry, the choice of cement is crucial for the longevity and stability of dental crowns. Dentists have the option to use either bonded or non-bonded cements. Bonded crowns are fixed using resin cement, which typically offers a stronger adhesion compared to non-bonded cements. The study categorized crowns as bonded if resin cement was used.
To understand the factors that influence the decision to bond a crown, the researchers used mixed-model logistic regression, a statistical method that assesses the relationship between various clinical factors and the likelihood of a dentist choosing to bond a crown.
Results
The results showed that 38.1% of the crowns in the study were bonded, while 61.9% were non-bonded. Interestingly, the study revealed a wide range of practices among the participating dentists. About 39.1% (79 of 202) of the dentists never bonded a crown during the study, indicating a preference for non-bonded cements. On the other hand, 20.3% (41 of 202) of the dentists bonded every crown, showing a strong preference for bonded restorations.
Several clinical factors were found to significantly influence the decision to bond a crown. One key factor was the amount of occlusal reduction, which refers to the amount of tooth structure removed to create space for the crown. Crowns with excessive occlusal reduction, as judged by laboratory technicians, were more likely to be bonded (P = .02). This suggests that when a significant amount of tooth structure is removed, dentists may prefer the added retention that bonding provides. However, other factors such as excessive taper (P = .15) and axial reduction (P = .08) did not show a significant association with the decision to bond.
The type of material used for the crown also played a significant role in the decision to bond. Crowns made from leucite-reinforced glass ceramic (76.5%) or lithium disilicate (70.8%) were far more likely to be bonded compared to those made from layered zirconia (38.8%), full-contour zirconia (30.1%), full metal (14.7%), or porcelain-fused-to-metal (13.8%) (P < .01). This finding highlights the preference for bonding when using glass ceramics, likely due to their esthetic properties and the need for strong adhesion to avoid fractures.
The location of the crown within the mouth was another important factor. Crowns placed in the anterior maxilla, which is the front upper part of the mouth, were significantly more likely to be bonded (P < .01). This may be due to the higher esthetic demands in this area, where patients and dentists prefer crowns that are securely attached and less likely to fail.
Interestingly, the study found no significant association between the decision to bond and the location of the crown margin (P = .35), which refers to the edge of the crown where it meets the tooth. This suggests that the decision to bond is more influenced by the overall preparation of the tooth and the type of material used rather than the specific details of the margin placement.
Conclusion
The study identified several key factors that influence a dentist’s decision to use bonded cement for single-unit crowns. Excessive occlusal reduction, anterior crown placement, and the use of glass ceramic materials were all significantly associated with the choice to bond. These findings provide valuable insights for dental practitioners, helping them make informed decisions about crownt cement selection based on the specific clinical circumstances of each case. Understanding these factors can lead to better outcomes for patients, with crowns that are more durable, esthetically pleasing, and less likely to fail over time.
Source: Pubmed