Glossitis is a condition characterized by inflammation of the tongue, often resulting in changes to its color, texture, and overall function. While it may seem like a localized issue, glossitis can indicate underlying systemic health problems, ranging from nutritional deficiencies to autoimmune diseases. Its causes are varied, its symptoms often uncomfortable, and its treatment necessitates a comprehensive understanding of both the immediate inflammation and any underlying health concerns.
This article delves deep into glossitis, exploring its causes, symptoms, diagnostic methods, and treatment options. Additionally, it will highlight preventive measures, offering a holistic perspective on managing this condition.
Table of Contents
ToggleWhat is Glossitis?
Glossitis refers to inflammation of the tongue, often resulting in swelling, pain, changes in color, and loss of papillae on the tongue’s surface, leading to a smooth and shiny appearance. Depending on the cause, glossitis can either be acute (lasting for a short time) or chronic (long-lasting). It may also recur if the underlying cause isn’t adequately addressed.
Types of Glossitis
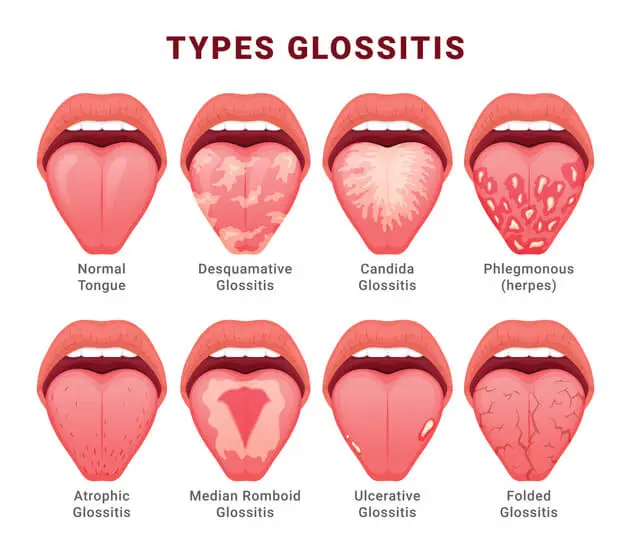
There are different types of glossitis, often categorized based on their clinical presentation:
- Acute Glossitis
- Chronic Glossitis
- Atrophic Glossitis (Hunter’s Glossitis)
- Geographic Tongue (Benign Migratory Glossitis)
- Median Rhomboid Glossitis
Acute Glossitis
This occurs suddenly and is often due to allergic reactions, infections, or trauma to the tongue. It is generally temporary but may cause significant discomfort.
Chronic Glossitis
This form persists over time and is often linked to systemic health issues like nutritional deficiencies or autoimmune conditions.
Atrophic Glossitis (Hunter’s Glossitis)
In this type, the papillae on the tongue’s surface shrink, resulting in a smooth and glossy appearance. It’s often associated with deficiencies in nutrients like vitamin B12, iron, and folic acid.
Geographic Tongue (Benign Migratory Glossitis)
This is a non-inflammatory type of glossitis where certain areas of the tongue lose papillae, giving the tongue a map-like appearance. While it may be alarming, this condition is usually harmless.
Median Rhomboid Glossitis
This is characterized by a smooth, red, and flat lesion in the middle of the tongue. It’s often linked to a chronic fungal infection (Candida) and may not present any noticeable symptoms in some cases.
Causes of Glossitis
Glossitis has various causes, which can range from local irritants to systemic health conditions. Understanding the underlying causes is crucial for proper diagnosis and treatment.
- Nutritional Deficiencies
- Infections
- Allergic Reactions
- Trauma and Irritation
- Autoimmune Diseases
- Other Causes
Nutritional Deficiencies
Nutritional imbalances are one of the most common causes of glossitis. Deficiencies in certain vitamins and minerals can impair the health of the tongue’s tissue:
- Vitamin B12 Deficiency
- Iron Deficiency
- Folic Acid Deficiency
Vitamin B12 Deficiency
A lack of vitamin B12 can lead to megaloblastic anemia, which is characterized by large and abnormal red blood cells. A telltale sign of this condition is a red, smooth, and swollen tongue (atrophic glossitis).
Iron Deficiency
Iron is essential for the production of hemoglobin. Iron-deficiency anemia can lead to glossitis, causing a pale, swollen, and smooth tongue. Iron helps in the regeneration of the papillae, and its deficiency often results in their loss.
Folic Acid Deficiency
Folic acid, or vitamin B9, plays a vital role in cell division and tissue growth. Deficiency can also result in megaloblastic anemia and glossitis, which presents similarly to that caused by vitamin B12 deficiency.
Infections
Infections, both fungal and bacterial, can cause glossitis.
- Candidiasis (Oral Thrush)
- Bacterial Infections
- Viral Infections
Candidiasis (Oral Thrush)
Candida albicans, a yeast-like fungus, is often found in small amounts in the mouth. However, under certain conditions (such as a weakened immune system or antibiotic use), it can overgrow and cause glossitis. The tongue may appear red and raw or develop white patches that are difficult to scrape off.
Bacterial Infections
Bacterial infections, particularly from organisms like Streptococcus and Staphylococcus, can cause glossitis. This may occur following injury or trauma to the tongue or as a result of poor oral hygiene.
Viral Infections
Viruses, such as herpes simplex virus (HSV), can lead to glossitis, especially during an outbreak of oral herpes, which causes painful sores on the tongue.
Allergic Reactions
Glossitis can be triggered by allergic reactions to various substances:
- Foods
- Medications
- Dental Products
Foods
Some people develop glossitis due to an allergic reaction to certain foods, especially spicy or acidic foods, which can irritate the tongue.
Medications
Certain medications, like antibiotics or NSAIDs (non-steroidal anti-inflammatory drugs), can cause allergic reactions that lead to glossitis.
Dental Products
Ingredients in toothpaste, mouthwashes, or other oral care products may irritate the tongue and cause an allergic reaction.
Trauma and Irritation
Physical trauma or continuous irritation to the tongue can lead to glossitis. Some common causes include:
- Burns
- Biting or Scraping
- Dentures and Braces
Burns
Eating or drinking something too hot can burn the tongue, leading to temporary glossitis.
Biting or Scraping
Accidentally biting the tongue or scraping it with rough or sharp objects can cause injury, inflammation, and swelling.
Dentures and Braces
Poorly fitting dentures or braces can rub against the tongue, leading to chronic irritation and inflammation.
Autoimmune Diseases
Certain autoimmune diseases are linked to glossitis, as the body’s immune system mistakenly attacks healthy cells in the tongue:
- Sjogren’s Syndrome
- Lupus (Systemic Lupus Erythematosus)
- Pemphigus Vulgaris
Sjogren’s Syndrome
This autoimmune disorder primarily affects the body’s moisture-producing glands, leading to dry mouth, which can result in tongue inflammation.
Lupus (Systemic Lupus Erythematosus)
Lupus can cause inflammation in various parts of the body, including the tongue.
Pemphigus Vulgaris
Pemphigus is a rare autoimmune disorder that causes painful blisters in the mouth, including on the tongue.
Other Causes
- Hormonal Imbalances
- Tobacco Use
- Dehydration
Hormonal Imbalances
Hormonal changes, such as those that occur during pregnancy, menopause, or due to thyroid disorders, can lead to glossitis.
Tobacco Use
Smoking or chewing tobacco irritates the tongue, leading to inflammation over time. Tobacco can also increase the risk of fungal infections, such as oral thrush, which can contribute to glossitis.
Dehydration
Chronic dehydration can dry out the mucous membranes, including those on the tongue, making them more prone to inflammation.
Symptoms of Glossitis
The symptoms of glossitis vary depending on the underlying cause and the type of glossitis present. Some of the most common symptoms include:
- Tongue Swelling
- Changes in Color
- Smooth Appearance
- Pain or Tenderness
- Difficulty in Eating or Speaking
- Burning Sensation
- Dry Mouth
- Taste Alterations
Tongue Swelling
The tongue may become swollen, which can interfere with speech, chewing, and swallowing.
Changes in Color
Glossitis often causes changes in the color of the tongue. The tongue may become bright red, pale, or darker than usual.
Smooth Appearance
In atrophic glossitis, the tongue loses its bumpy, textured surface due to the loss of papillae. This results in a smooth, shiny appearance.
Pain or Tenderness
Glossitis can cause the tongue to become painful or tender, especially when eating spicy or acidic foods.
Difficulty in Eating or Speaking
Swelling and pain in the tongue may make it difficult to chew, swallow, or articulate words properly.
Burning Sensation
A burning sensation on the tongue is common, particularly in glossitis caused by infections or nutritional deficiencies.
Dry Mouth
If glossitis is associated with conditions like Sjogren’s syndrome, a dry mouth may accompany the tongue inflammation.
Taste Alterations
Glossitis may lead to changes in taste perception, particularly if the papillae (which house taste buds) are affected.
Potential Complications
If left untreated, glossitis can lead to several complications, including:
- Difficulty in Breathing
- Malnutrition
- Chronic Pain and Discomfort
- Secondary Infections
Difficulty in Breathing
Severe tongue swelling can obstruct the airway, making it difficult to breathe.
Malnutrition
If glossitis makes it painful to eat, it can result in reduced food intake, potentially leading to malnutrition.
Chronic Pain and Discomfort
Chronic glossitis, especially when caused by underlying systemic conditions, can lead to ongoing pain and discomfort that may interfere with daily activities.
Secondary Infections
In cases where the tongue’s surface is damaged or ulcerated due to trauma or inflammation, secondary bacterial or fungal infections can develop, complicating the primary condition.
Diagnosis of Glossitis
Accurate diagnosis of glossitis involves a comprehensive clinical evaluation, which may include a thorough medical history, physical examination, and diagnostic tests. The healthcare provider will need to identify both the immediate cause of the tongue inflammation and any potential underlying health issues contributing to the condition.
Medical History and Physical Examination
The initial diagnostic step usually involves obtaining a detailed medical history. The healthcare provider will ask questions about:
- Duration of Symptoms: How long the patient has been experiencing tongue inflammation and associated symptoms.
- Recent Diet Changes: Any changes in the patient’s diet, including potential food allergies, deficiencies in vitamins or minerals, or the consumption of hot, spicy, or irritating foods.
- Medications: A review of medications the patient is taking, including those that may cause allergic reactions or nutrient deficiencies.
- Allergies: A history of allergies to foods, dental products, or medications.
- Oral Hygiene Practices: Habits related to oral care, including the use of toothpaste, mouthwash, or any dental prosthetics that may be irritating the tongue.
- Other Health Conditions: An assessment of any pre-existing medical conditions, such as autoimmune diseases, anemia, or hormonal imbalances, that could be linked to glossitis.
During the physical examination, the healthcare provider will inspect the tongue’s appearance, noting its color, texture, and any visible signs of infection, ulcers, or other abnormalities. The provider will also check for other signs of systemic health problems, such as pale skin (which may indicate anemia), swollen lymph nodes (which could suggest infection), or dry mucous membranes.
Laboratory Tests
If the cause of glossitis isn’t immediately apparent, or if an underlying systemic condition is suspected, the following laboratory tests may be ordered:
- Complete Blood Count (CBC): Blood test is useful for diagnosing anemia, which is often associated with glossitis caused by vitamin B12, iron, or folic acid deficiencies. It also helps assess the overall health of the immune system.
- Serum Ferritin and Iron Levels: To detect iron deficiency, which is a common cause of atrophic glossitis, doctors may measure the levels of ferritin (a protein that stores iron) and serum iron.
- Vitamin B12 and Folate Levels: Deficiencies in these nutrients can lead to atrophic glossitis. Testing for serum levels of vitamin B12 and folate will help determine if supplementation is necessary.
- Thyroid Function Tests: If glossitis is suspected to be linked to hormonal imbalances, such as those caused by hypothyroidism, thyroid function tests may be performed to measure levels of thyroid hormones (TSH, T3, T4).
- Culture Tests: If a bacterial or fungal infection is suspected, a culture of the tongue’s surface may be taken to identify the responsible microorganism. This is particularly useful in cases of oral candidiasis.
- Allergy Testing: For patients with suspected allergic glossitis, patch testing or other forms of allergy testing may be conducted to identify potential allergens.
Biopsy
In cases where glossitis is chronic or recurrent, and the underlying cause remains unclear, a biopsy of the tongue tissue may be performed. A biopsy involves taking a small sample of tissue from the tongue for microscopic examination. This can help rule out serious conditions such as cancer, autoimmune diseases, or chronic infections.
Treatment of Glossitis
Treatment for glossitis depends largely on the underlying cause. Once the specific cause is identified, the goal of treatment is to reduce inflammation, alleviate symptoms, and address any contributing factors such as infections, allergies, or nutritional deficiencies.
Dietary and Nutritional Management
- Vitamin B12 Supplementation
- Iron Supplements
- Folic Acid Supplements
- Dietary Adjustments
Vitamin B12 Supplementation
If glossitis is caused by a vitamin B12 deficiency, oral or intramuscular B12 supplements will be prescribed. Regular monitoring of B12 levels is necessary to ensure proper management.
Iron Supplements
For cases of iron-deficiency anemia, iron supplements are recommended to restore hemoglobin levels and improve the health of the tongue. Iron-rich foods, such as lean meats, leafy greens, and legumes, may also be advised.
Folic Acid Supplements
In cases of folic acid deficiency, folic acid supplements can help regenerate the papillae on the tongue, reducing the smoothness and inflammation.
Dietary Adjustments
Eating a balanced diet rich in vitamins and minerals is essential for maintaining oral health. Patients may be advised to avoid spicy, hot, or acidic foods that could exacerbate tongue irritation.
Treatment for Infections
- Antifungal Medications
- Antibiotics
- Antiviral Medications
Antifungal Medications
If glossitis is caused by oral thrush (candidiasis), antifungal medications such as nystatin, clotrimazole, or fluconazole will be prescribed to eliminate the infection. Topical antifungal treatments may also be used directly on the affected areas of the tongue.
Antibiotics
In cases of bacterial glossitis, oral antibiotics may be necessary to treat the infection. Careful use of antibiotics is essential to prevent antibiotic resistance and protect the healthy flora in the mouth.
Antiviral Medications
For viral infections like herpes simplex, antiviral medications such as acyclovir or valacyclovir may be used to reduce the severity and duration of the outbreak.
Managing Allergic Reactions
- Allergen Avoidance
- Antihistamines
- Corticosteroids
Allergen Avoidance
If the glossitis is triggered by an allergic reaction, identifying and avoiding the allergen is crucial. For example, if a food allergy is responsible, the patient must eliminate that food from their diet.
Antihistamines
In cases of mild allergic glossitis, over-the-counter antihistamines may be recommended to reduce inflammation and swelling of the tongue.
Corticosteroids
For more severe allergic reactions, corticosteroids (either topical or systemic) may be prescribed to reduce inflammation and suppress the immune response.
Addressing Autoimmune and Systemic Conditions
If glossitis is a symptom of an underlying autoimmune disorder, treating the primary condition is crucial. Depending on the specific disorder, treatment may involve:
- Immunosuppressive Therapy
- Saliva Substitutes
Immunosuppressive Therapy
Autoimmune diseases like lupus or pemphigus vulgaris may require immunosuppressive drugs such as corticosteroids, methotrexate, or azathioprine to manage the immune system’s overactivity.
Saliva Substitutes
For patients with Sjogren’s syndrome or other conditions causing dry mouth, saliva substitutes or medications that stimulate saliva production may help reduce tongue inflammation.
Addressing Trauma and Irritation
- Mouth Guards or Dental Adjustments
- Avoiding Irritants
- Oral Care Products
Mouth Guards or Dental Adjustments
If glossitis is caused by irritation from dentures or braces, adjusting the fit of the dental prosthetics or using a mouthguard can alleviate the problem.
Avoiding Irritants
Patients are advised to avoid tobacco, alcohol, and irritants like hot or spicy foods that can aggravate the tongue’s surface.
Oral Care Products
Switching to mild, non-irritating toothpaste and mouthwash can help reduce glossitis caused by reactions to dental hygiene products.
Prevention of Glossitis
While some cases of glossitis are unavoidable, such as those caused by autoimmune diseases or genetic factors, many cases can be prevented by taking steps to maintain good oral and overall health.
Maintain Good Oral Hygiene
Practicing proper oral hygiene is key to preventing infections and irritations that can lead to glossitis. This includes:
- Brushing teeth twice daily with a soft-bristled toothbrush.
- Using a mild toothpaste free of harsh chemicals.
- Flossing daily to remove food particles and plaque between teeth.
- Using an alcohol-free mouthwash to kill bacteria without irritating the tongue.
Balanced Diet
Eating a well-balanced diet rich in essential vitamins and minerals can prevent nutritional deficiencies that contribute to glossitis. Foods high in iron, vitamin B12, and folic acid should be included in the diet. If necessary, dietary supplements may be used to fill nutritional gaps.
Avoiding Irritants
Avoiding known tongue irritants, such as spicy foods, alcohol, and tobacco products, can help prevent tongue inflammation. Patients with a history of allergic reactions to certain foods or dental products should be cautious and read labels carefully.
Regular Medical Checkups
Routine checkups with a healthcare provider or dentist can help detect underlying health issues early on, before they lead to complications like glossitis. Conditions like anemia or autoimmune diseases can often be managed with early intervention.
Stay Hydrated
Ensuring adequate hydration by drinking plenty of water throughout the day helps maintain a moist, healthy oral environment, which can reduce the risk of tongue irritation and inflammation.
Prognosis of Glossitis
The prognosis for glossitis is generally good, especially if the underlying cause is identified and treated promptly. Most cases resolve completely with appropriate treatment, and the tongue regains its normal appearance and function. However, chronic glossitis related to systemic conditions like autoimmune diseases or persistent nutritional deficiencies may require ongoing management to prevent recurrence.
Frequently Asked Questions (FAQs)
What is the main cause of glossitis?
Glossitis is most commonly linked to nutritional deficiencies—especially a lack of B vitamins, iron, or folic acid. Other contributing factors include irritation from spicy or acidic foods, allergies, infections, and sometimes systemic conditions.
How to treat glossitis naturally?
Natural management strategies include maintaining excellent oral hygiene, rinsing with a mild saltwater solution, and using cold compresses or ice chips to soothe discomfort. It’s also important to avoid irritants (such as spicy, acidic foods, and alcohol) and ensure a balanced diet rich in essential vitamins and minerals. Herbal teas like chamomile may provide additional relief.
Does B12 deficiency cause glossitis?
Yes. A deficiency in vitamin B12 is a well-known trigger for glossitis. Insufficient B12 levels can lead to inflammation and a sore, red, or swollen tongue.
Why is my tongue swollen and sore on the sides?
Swelling and soreness on the sides of the tongue can be symptoms of glossitis, but they might also be caused by allergic reactions, irritants, or infections. If the condition persists, it’s wise to seek evaluation from a healthcare professional for an accurate diagnosis.
Is glossitis cancerous?
Glossitis is typically a benign inflammatory condition and is not cancerous. However, any persistent or unusual changes in your tongue should be examined by a healthcare provider to rule out other, more serious conditions.
What does iron deficiency tongue look like?
When linked to iron deficiency, the tongue may appear unusually smooth or glossy, sometimes pale or red, due to the loss of its normal bumps (papillae). This condition is often accompanied by a burning sensation or discomfort.
What foods should you avoid with glossitis?
To minimize irritation, it’s best to steer clear of spicy and acidic foods, as well as rough-textured items that can scrape or further inflame the tongue. Limiting alcohol and hot beverages can also help reduce discomfort.
What triggers geographic tongue?
Geographic tongue, also known as benign migratory glossitis, is thought to be triggered by factors such as stress, hormonal changes, certain dietary components, or even genetic predisposition. Although its exact cause isn’t fully understood, these factors are often associated with its occurrence.
Can stress cause glossitis?
While stress isn’t usually the primary cause of glossitis, it can exacerbate the condition. Stress may weaken the immune system or worsen existing nutritional imbalances, making the tongue more susceptible to inflammation and irritation.
Conclusion
Glossitis is a condition with a wide range of causes, from infections and nutritional deficiencies to trauma and autoimmune diseases. While its symptoms can be uncomfortable and affect daily activities, proper diagnosis and treatment usually lead to a
full recovery. Understanding the underlying cause is key to successful treatment, as glossitis often serves as a sign of broader health issues. By addressing both the immediate symptoms and any systemic conditions, healthcare providers can help patients manage this condition effectively.
The tongue plays an essential role in various functions, including eating, speaking, and maintaining oral health. When this problem disrupts these functions, it can significantly affect a person’s quality of life. Timely intervention—whether through dietary adjustments, medications, or lifestyle changes—can restore the tongue’s health and alleviate discomfort.