Endocrine system plays a crucial role in regulating numerous bodily functions, ranging from metabolism and growth to reproduction and mood. Comprised of glands that secrete hormones, this system ensures that various processes occur in harmony. However, when the endocrine system malfunctions, it can lead to a wide range of disorders, collectively known as endocrine disorders. These conditions can have profound effects on an individual’s health and quality of life, and understanding them is essential for effective management and treatment.
This article provides a comprehensive overview of endocrine disorders, including their causes, symptoms, diagnosis, and treatment options.
Table of Contents
ToggleWhat is the Endocrine System?
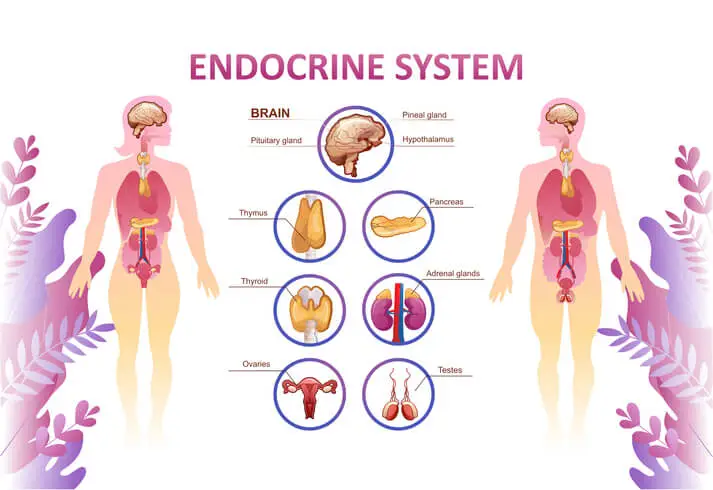
The endocrine system consists of glands and organs that produce and release hormones. Hormones are chemical messengers that travel through the bloodstream, regulating numerous physiological processes. The major components of the endocrine system include:
- Pituitary gland – Often referred to as the “master gland,” it controls other endocrine glands and regulates growth, reproduction, and metabolism.
- Thyroid gland – Produces hormones that regulate metabolism, energy production, and growth.
- Adrenal glands – Located above the kidneys, they produce hormones involved in stress response, metabolism, and immune system regulation.
- Pancreas – Produces insulin and glucagon, which control blood sugar levels.
- Gonads (ovaries and testes) – Regulate reproduction and secondary sexual characteristics.
- Parathyroid glands – Control calcium levels in the blood.
- Pineal gland – Produces melatonin, which influences sleep-wake cycles.
Disruptions in the production, regulation, or action of hormones can result in endocrine disorders.
Types of Endocrine Disorders
Endocrine disorders encompass a wide spectrum of conditions. Here are some of the most common types:
- Diabetes Mellitus
- Thyroid Disorders
- Cushing’s Syndrome
- Addison’s Disease
- Polycystic Ovary Syndrome (PCOS)
- Acromegaly and Gigantism
- Hypoparathyroidism and Hyperparathyroidism
- Pheochromocytoma
- Pituitary Disorders
- Congenital Adrenal Hyperplasia (CAH)
Diabetes Mellitus
Diabetes is one of the most prevalent endocrine disorders, affecting millions worldwide. It occurs when the pancreas either does not produce enough insulin or the body cannot use it effectively. There are two primary types:
- Type 1 Diabetes – An autoimmune condition where the immune system attacks insulin-producing cells.
- Type 2 Diabetes – Characterized by insulin resistance and often associated with obesity and lifestyle factors.
Thyroid Disorders
Thyroid disorders are among the most common endocrine conditions, affecting the thyroid gland’s function.
- Hypothyroidism – The thyroid produces insufficient hormones, leading to fatigue, weight gain, and depression.
- Hyperthyroidism – Excessive thyroid hormone production causes symptoms like weight loss, rapid heartbeat, and irritability.
- Goiter – Enlargement of the thyroid, often due to iodine deficiency.
- Thyroid cancer – Malignancy of the thyroid gland.
Cushing’s Syndrome
This condition results from excessive cortisol production, often due to long-term corticosteroid use or a tumor in the adrenal gland. Symptoms include weight gain, high blood pressure, and muscle weakness.
Addison’s Disease
Also known as adrenal insufficiency, Addison’s disease occurs when the adrenal glands do not produce enough cortisol and aldosterone. Symptoms include fatigue, low blood pressure, and hyperpigmentation of the skin.
Polycystic Ovary Syndrome (PCOS)
PCOS is a hormonal disorder affecting women of reproductive age. It is characterized by irregular menstrual cycles, ovarian cysts, and excessive androgen levels, leading to symptoms like acne, excessive hair growth, and infertility.
Acromegaly and Gigantism
These conditions arise from excessive growth hormone production, often due to a pituitary tumor. Gigantism occurs in children, leading to abnormal height, while acromegaly affects adults, causing enlarged facial features and extremities.
Hypoparathyroidism and Hyperparathyroidism
- Hypoparathyroidism – Low parathyroid hormone levels lead to calcium deficiency, causing muscle cramps and seizures.
- Hyperparathyroidism – Excess parathyroid hormone results in high calcium levels, leading to kidney stones and bone weakness.
Pheochromocytoma
A rare tumor of the adrenal gland that results in excessive production of adrenaline, causing high blood pressure, sweating, and rapid heartbeat.
Pituitary Disorders
These include conditions like:
- Hypopituitarism – Reduced hormone production by the pituitary gland.
- Prolactinoma – A benign tumor causing excessive prolactin production, leading to infertility and sexual dysfunction.
Congenital Adrenal Hyperplasia (CAH)
A group of genetic disorders affecting adrenal gland function, often leading to abnormal hormone production and ambiguous genitalia in newborns.
Causes of Endocrine Disorders
Endocrine disorders can arise from various factors, including:
- Genetic Mutations – Many endocrine disorders, such as CAH and hereditary thyroid cancers, are inherited.
- Autoimmune Disorders – Conditions like Type 1 diabetes and Hashimoto’s thyroiditis occur when the immune system attacks endocrine glands.
- Tumors – Benign or malignant growths can disrupt glandular function.
- Infections – Some infections can damage endocrine organs, such as the pancreas in viral-induced diabetes.
- Lifestyle Factors – Obesity, poor diet, and lack of exercise can contribute to Type 2 diabetes and PCOS.
- Environmental Factors – Exposure to endocrine-disrupting chemicals (EDCs), such as pesticides and plastics, can interfere with hormone production.
- Medications – Long-term use of certain drugs, such as corticosteroids, can affect hormone balance.
Symptoms of Endocrine Disorders
Symptoms vary depending on the specific disorder but often include:
- Fatigue – A common symptom in conditions like hypothyroidism and Addison’s disease.
- Weight Changes – Unexplained weight gain or loss is often associated with thyroid and adrenal disorders.
- Mood Swings – Depression, anxiety, and irritability can occur due to hormonal imbalances.
- Changes in Heart Rate – Tachycardia in hyperthyroidism or bradycardia in hypothyroidism.
- Reproductive Issues – Irregular menstrual cycles, infertility, or sexual dysfunction in disorders like PCOS and prolactinoma.
- Muscle Weakness – Common in Cushing’s syndrome and hyperparathyroidism.
- Skin Changes – Hyperpigmentation in Addison’s disease or dry skin in hypothyroidism.
- Excessive Thirst and Urination – Hallmarks of diabetes mellitus.
Diagnosis of Endocrine Disorders
Diagnosis often involves a combination of medical history, physical examination, and laboratory tests. Key diagnostic tools include:
- Blood Tests – Measure hormone levels to identify deficiencies or excesses.
- Imaging Studies – Ultrasound, MRI, or CT scans help visualize gland abnormalities, such as tumors or enlargement.
- Stimulation or Suppression Tests – Assess gland function by stimulating or suppressing hormone production.
- Biopsy – Tissue sampling may be necessary for suspected cancers.
- Genetic Testing – Identifies inherited endocrine disorders.
Treatment Options
Treatment for endocrine disorders varies depending on the underlying condition:
- Hormone Replacement Therapy
- Medications
- Surgery
- Radiation Therapy
- Lifestyle Modifications
- Monitoring and Follow-Up
Hormone Replacement Therapy
- Used for conditions like hypothyroidism, Addison’s disease, and hypopituitarism.
- Involves administering synthetic hormones to restore balance.
Medications
- Anti-thyroid drugs – Treat hyperthyroidism by reducing thyroid hormone production.
- Insulin – Essential for managing Type 1 diabetes.
- Metformin – A common drug for Type 2 diabetes and PCOS.
Surgery
- Removal of tumors in the thyroid, adrenal glands, or pituitary gland.
- Thyroidectomy for thyroid cancer or severe hyperthyroidism.
Radiation Therapy
Used for certain types of endocrine cancers or overactive thyroid tissue.
Lifestyle Modifications
Diet and exercise play a crucial role in managing diabetes, PCOS, and obesity-related endocrine disorders.
Monitoring and Follow-Up
Regular monitoring of hormone levels and gland function is vital to prevent complications.
Complications of Untreated Endocrine Disorders
Without proper treatment, endocrine disorders can lead to severe complications, including:
- Cardiovascular Disease – Common in diabetes and hyperthyroidism.
- Osteoporosis – Associated with hyperparathyroidism and Cushing’s syndrome.
- Infertility – Seen in PCOS and prolactinoma.
- Vision Loss – Diabetes-related retinopathy or pituitary tumor-induced compression of optic nerves.
- Neurological Issues – Peripheral neuropathy in diabetes or seizures in hypoparathyroidism.
Preventing Endocrine Disorders
While some endocrine disorders cannot be prevented due to genetic or autoimmune causes, lifestyle changes can reduce the risk of others:
- Healthy Diet – Focus on balanced nutrition to prevent obesity and Type 2 diabetes.
- Regular Exercise – Improves insulin sensitivity and hormonal balance.
- Stress Management – Reduces the risk of stress-related disorders like Cushing’s syndrome.
- Avoiding Endocrine Disruptors – Limit exposure to harmful chemicals in plastics, pesticides, and processed foods.
- Regular Health Check-ups – Early detection of hormonal imbalances through routine screening.
Impact of Endocrine Disorders on Dental Treatments and Oral Health
Endocrine disorders can significantly influence dental treatments and oral health, requiring dentists to adopt specialized approaches when managing patients with such conditions. Hormonal imbalances, such as those seen in diabetes mellitus, can impair wound healing, increase susceptibility to infections, and exacerbate periodontal diseases.
Hyperthyroidism or hypothyroidism can affect the metabolism of anesthetic agents and the patient’s stress response, necessitating careful monitoring during dental procedures.
Similarly, conditions like Cushing’s syndrome and Addison’s disease, which affect adrenal gland function, may require adjustments to corticosteroid therapy to prevent adrenal crises during invasive treatments.
Patients with osteoporosis caused by endocrine disorders such as hyperparathyroidism may be at higher risk for jawbone complications, especially if they are on bisphosphonate therapy. For women with hormonal disorders like PCOS or those undergoing menopause, fluctuating estrogen levels can lead to dry mouth, burning mouth syndrome, or increased oral discomfort.
Understanding the interplay between endocrine health and oral health is vital for tailoring safe, effective, and patient-centered dental care.
Frequently Asked Questions (FAQs)
How do endocrine disorders affect oral health?
Endocrine disorders can impact oral health in various ways, including increased susceptibility to infections, delayed wound healing, dry mouth, gum disease, and changes in bone density. Conditions like diabetes, thyroid disorders, and hormonal imbalances can contribute to oral complications, making regular dental check-ups essential for early detection and management.
Why is diabetes a concern for dental treatments?
Diabetes affects the body’s ability to heal and fight infections, increasing the risk of gum disease, oral infections, and delayed recovery after dental procedures. Poorly controlled diabetes can also lead to dry mouth (xerostomia), which raises the risk of cavities and fungal infections like oral candidiasis.
Can thyroid disorders impact dental procedures?
Yes. Hyperthyroidism can increase sensitivity to epinephrine in local anesthetics, leading to complications such as rapid heart rate or high blood pressure. Hypothyroidism, on the other hand, can cause delayed healing and increased sensitivity to pain, requiring adjustments in dental care plans.
What precautions should be taken for dental treatments in patients with adrenal disorders?
Patients with adrenal disorders, such as Addison’s disease or Cushing’s syndrome, may need special considerations due to their altered stress response. Those on long-term corticosteroids may require steroid supplementation before major dental procedures to prevent an adrenal crisis.
How does osteoporosis affect dental treatments?
Osteoporosis, often linked to endocrine disorders like hyperparathyroidism or menopause, can weaken the jawbone, increasing the risk of fractures and complications after extractions or implant procedures. Patients taking bisphosphonates should inform their dentist, as these medications can lead to osteonecrosis of the jaw (ONJ).
Are women with hormonal disorders at higher risk for oral health problems?
Yes, hormonal fluctuations during puberty, pregnancy, menopause, and conditions like PCOS can contribute to gum inflammation, dry mouth, and an increased risk of cavities and periodontal disease. Hormone-related changes can also lead to burning mouth syndrome and oral discomfort.
What can be done to protect oral health in patients with endocrine disorders?
Patients with endocrine disorders should maintain good oral hygiene, follow a balanced diet, and schedule regular dental check-ups. Dentists may also recommend fluoride treatments, saliva substitutes for dry mouth, and tailored oral care routines based on the patient’s specific hormonal condition.
Should dental procedures be modified for patients with endocrine disorders?
Yes, modifications may be needed depending on the endocrine disorder. For example, blood sugar levels should be stabilized before dental treatments in diabetic patients, and stress reduction techniques should be used for individuals with adrenal insufficiency. Dentists should work closely with endocrinologists to ensure safe and effective treatment.
Can endocrine disorders cause bad breath?
Yes, certain endocrine disorders, such as diabetes (due to ketoacidosis) and hypothyroidism (due to dry mouth), can contribute to persistent bad breath. Proper management of the underlying condition, along with good oral hygiene and hydration, can help alleviate this issue.
Why is it important to inform my dentist about my endocrine disorder?
Informing your dentist about your endocrine condition ensures that they can tailor treatments to minimize risks and complications. Certain medications and dental procedures may need to be adjusted to accommodate your hormonal condition, improving both your safety and treatment outcomes.
Conclusion
Endocrine disorders encompass a diverse range of conditions that can significantly impact an individual’s health. Understanding the causes, symptoms, and treatment options is essential for effective management. Advances in medical research and technology have improved diagnosis and treatment, allowing many individuals with endocrine disorders to lead healthy lives. However, early detection, lifestyle modifications, and adherence to treatment are key to preventing complications and maintaining optimal endocrine health.