Table of Contents
ToggleAbstract:
Introduction:
Insertion of dental implants in alveolar bone could be performed following flap reflection or using flapless technique. The aim of the current study was to systematically review and compare implant treatment outcome including success and survival rates, marginal bone loss and post-operative complications between two techniques of implant insertion: flapped and flapless.
Material and Methods
A PubMed search was performed in February 2017 using relevant keywords limited to human studies and English language. Clinical studies evaluating the survival rate, alveolar bone loss and rate of complications between flapped and flapless techniques for implant insertion were included. More than 6 months follow up and more than 10 patients were the inclusion criteria. The review process was performed by two reviewers and the relevant data was extracted from the included studies. Data was compared in a qualitative manner.
Results
PubMed database search resulted in 1529 studies. Out of these studies 21 were selected based on inclusion and exclusion criteria. 13 studies were randomized clinical trial, 7 were prospective and one study was retrospective. Five studies assess implant treatment outcome only using flapless technique while other 16 studies compared both techniques. The Total number of patients were 1069 ones (age ranged between 18 to 86 years). Total number of implants was 2331 implants. No significant difference was found between success and survival rate of implants using two techniques except for one study that reported higher success rate in flapless group. 7 studies reported higher marginal bone loss in flapped groups and 6 studies reported no difference in marginal bone loss between two groups. Less pain following flapless technique was reported in 6 studies. One study, however, showed more pain in flapless technique. Less oedema and shorted surgical time in flapless group was also reported
Conclusion
Considering the limitations of this systematic review it could be concluded that implant survival rate using flapped and flapless technique is comparable. Also, marginal bone loss using flapless technique is similar or less than flapped technique. Concerning post-operative complications, it seems that flapless technique would probably have less post-operative pain and oedema. In addition, flapless approach could be performed in shorter surgical time compared to reflecting flaps.
Keywords: dental implant, flap, flapless, open flap, survival, and success
Introduction
Tooth loss could cause a not aesthetic appearance and may deteriorate mastication and speech. Nowadays, dental implants are common treatment modality for restoring missing or extracted teeth. The aim of implant therapy in dentistry is to restore tissue contour, function, comfort, aesthetic and speech. Several studies have shown relatively high success rate of dental implants (Ormianer and Palti 2006). Dental implants are the only treatment that can reach these goals without causing severe alveolar bone loss (Jokstad et al. 2003, Behnia et al. 2015). However, marginal bone loss is a common complication of dental implants (Morad et al. 2014, Vohra et al. 2015).
Several attempts have been done to prevent alveolar bone loss and increase dental implant success rate. These attempts include implant surface modification (acid etch, sandblast and hydroxyapatite coating) (Eroglu et al. 2016), implant geometry alteration (conical and cylindrical fixtures) (Cecchinato et al. 2015) and changing in implant threads (type, shape and depth of threads) (Jokstad et al. 2003, Khorsand et al. 2016). In addition, several modifications have been performed to reduce marginal bone loss following implant insertion.
On the one hand, conventional implant placement technique involves full thickness flap prior to implant insertion. This approach allows clinician to directly visualize the alveolar bone and assess bone morphology of the ridge. Also, using this technique crestal ridge morphology alteration and augmentation could be performed. The current guidelines indicate this technique in case of lack of sufficient attached gingiva and necessity of simultaneous recipient site augmentation (Stoupel et al. 2016). However, this technique is relatively invasive and cause patient discomfort and marginal bone loss. When flap is reflected, catabolic activities shifts and osteoclastic activity and bone loss increase .
On the other hand, flapless implant insertion technique which involves soft tissue removal using punch without flap reflection. Shorted surgery time and less patient discomfort has been reported using this technique . Although the clinicians suppose that flapless technique result in less marginal bone loss due to less invasive approach, the proposed disadvantage of this technique is less implant survival rate . This approach is indicated in some situations including but not limited to patients who demand for aesthetic treatment and the implant is supposed to be placed in the aesthetic zone (Chen et al. 2009), fractured teeth, endodontic failures, non-restorable caries, radicular caries (Scala et al. 2012). In these cases, the periodontal tissue should be healthy prior to the implant placement and any sign of soft tissue dehiscence and fenestrations in contraindication for flapless implant insertion (Scala et al. 2012).
Implant treatment outcome by flapless approach have been reviewed previously (Brodala 2009, Doan et al. 2012, Moraschini et al. 2015). A review of 13 studies revealed that flapless technique would result in 97.2% survival rate of dental implants and a mean 1.45 mm marginal bone loss during 1-4 years of follow up(Moraschini et al. 2015). Another review also showed 98.6% of implant survival rate using flapless technique (Brodala 2009). Flap less technique had 97.1% implant survival rate placed in the posterior of the maxilla (Doan et al. 2012). Also the rate of complications for this approach was 3.8% (Brodala 2009) and for posterior of the maxilla rate of complication was 6.55% (Doan et al. 2012).
Comparison of implant treatment outcome between flapped and flapless groups has been performed is some clinical studies (Becker et al. 2005, Ozan et al. 2007, Jeong et al. 2008, Job et al. 2008, Sunitha et al. 2008, Becker et al. 2009, Van de Velde et al. 2010, Jeong et al. 2011, Al-Juboori et al. 2012, Tsoukaki et al. 2013). Most studies revealed no significant difference in survival rate of dental implants between these two techniques. However, study by Jeong et al. (Jeong et al. 2008) reported higher success rate in flapless group. Comparison of mean marginal bone loss in flapped and flapless techniques showed significantly less bone loss using flapless technique in some studies (Becker et al. 2005, Job et al. 2008, Sunitha et al. 2008, Jeong et al. 2011, Tsoukaki et al. 2013)while some other researches showed no significant difference between these two implant insertion technique (Ozan et al. 2007, Becker et al. 2009, Van de Velde et al. 2010, Al-Juboori et al. 2012).
In addition, post-operative complications of flapless technique compared to the conventional flapped approach has been some other studies. The results of these studies have revealed less post-operative pain (Fortin et al. 2006, Cannizzaro et al. 2008, Cannizzaro et al. 2011, Al-Juboori et al. 2012, Tsoukaki et al. 2013) and oedema(Cannizzaro et al. 2008) using flapless technique.
On the other hand, comparison of these two technique has been performed in a systematic review (Vohra et al. 2015) and two meta-analyses (Chrcanovic et al. 2014, Lin et al. 2014). In review of Vohra et al. (Vohra et al. 2015) half of the include studies showed no difference in marginal bone loss two techniques while the other half reported less marginal bone loss in their flapless groups.Lin et al. (Lin et al. 2014) showed that the mean survival rate of implants in flapped and flapless techniques was 98.6% and 97%, respectively. Also comparison of the mean marginal bone loss showed a mean difference of 0.03 mm which was not statistically different. On the contrary, a meta-analysis by Chrcanovic et al. (Chrcanovic et al. 2014) showed significantly higher implant survival rate in flapped group compared to the flapless group. They concluded that implant placement using flapless technique increase risk of implant failure by 75%. In their meta-analysis, post-operative complication and marginal bone loss of flapped and flapless techniques showed no significant difference.
Purpose
The main purpose of this study was to systematically review published articles comparing implant survival rate, alveolar bone loss and post-operative complications between flapless and flapped implant insertion techniques.
Aim
The aim of the current study was to update previous reviews and compare implant treatment outcome between flapped and flapless techniques.
Background to Thesis and Review of the literature
Since the introduction of dental implants by Brånemark, several modifications have been done on the original technique. These aim of these modifications were not only more efficient treatment, but also better aesthetics and soft and hard tissue preservation(Bhat and Bangawala 2014).
Originally, dental implants were inserted following flap reflection only after dental socket filling and alveolar bone healing. In this traditional method, an incision would be made through the gingiva and a full thickness flap is elevated using manual instruments. Following flap elevation, drills are used in sequence to preform osteotomy. Using this method, the clinician would be able to visualize the bone during implant site preparation and insertion. In addition, re-contouring knife edge crestal ridge and alveolar bone augmentation could be performed(Summers 1994).
The concept of immediate implant placement was introduced to reduce dental implant treatment period(Chen et al. 2004). Several techniques have been introduced to perform immediate implant placement(Chen et al. 2004). Schwartz et al. (Schwartz-Arad and Chaushu 1997) described a surgical technique-reflecting flap for immediate implant placement. However, in this technique interdental papilla and alveolar bone loss could occur. On the other hand, Al-Ansari et al. (al-Ansari and Morris 1998) introduced immediate implant placement without flap reflection. In their study, 20 implants were inserted in the mandible and the maxilla and periodic clinical and radiologic evaluation of the results was performed for two years. They observed less bleeding and post-operative patient discomfort with no infection and necrosis. All the implants were survived. They concluded that immediate implant placement using flapless technique could result in more favourable outcome compared to the step technique.
Tsoukaki et al. (Tsoukaki et al. 2013)compared conventional and flapless technique and showed less marginal bone loss in the flapless group when the implants were still not loaded. However, other studies revealed no significant between two techniques regarding marginal bone loss of unloaded implants(Al-Juboori et al. 2012).
Later, Van de Velde et al. (Van de Velde et al. 2010) compared immediate placement of dental implants following flapless procedure to the delayed implant placement in flapped technique. The reported that a mean 1.9 mm marginal bone loss occurred in both groups after 18 months follow up. On the other hand, immediate implant insertion after flapped and flapless techniques revealed higher marginal bone loss in flapped group(Job et al. 2008).
Study of Sunitha et al. (Sunitha et al. 2008) showed 100% success rate of dental implants during 6 months of follow-ups. The placed 10 dental implant using flapped technique and 10 using flapless technique. The mean marginal bone losses in flapped and flapless groups were 1.01 mm and 0.68 mm, respectively.
Another study (Jeong et al. 2008), on the other hand, showed 96.47% of survival rate of dental implant (5 failures) using conventional flapped technique while the survival rate of implants in flapless group was 100%. In this study follow up period was 4 months and the mean marginal bone loss in flapless and flapped groups was 0.26 mm 0.20 mm, respectively.
On the contrary to the cited studies, the survival rate of dental implants using flapless technique is not always high. In study of Oh et al. (Oh et al. 2006) dental implants inserted using flapless technique had 87.5% survival rate during 6 months.
As some authors question success of flapless implants due to lack of visualization , some studies used computer guided technique for precise angulation of implant during insertion without flap reflection(Ozan et al. 2007, Van de Velde et al. 2010). Both cited studies reported very high success rate of implants placed using CT-guided flapless technique.
Hypothesis
Null hypothesis: There are no differences between flap reflection and flapless technique for implant placement regarding survival rate, bone loss and complications.
Material and Methods
Study design
In this current review, clinical studies evaluating the survival rate, alveolar bone loss and rate of complications between flapped and flapless techniques for implant insertion were included.
Inclusion Criteria
- Using flapless technique was necessary for inclusion while using flapped technique was not considered as inclusion criteria.
- Also, the minimum number of patients for inclusion was 10 patients.
Exclusion Criteria
- Animal studies, case reports and case series were excluded.
- Also, studies with less than 10 patients were excluded.
- Short implants (less than 8 mm length) were also excluded.
Electronic search and study selection
An electronic search was performed using PubMed and Medline until February 2017 limited to English language and human studies.
Search Terms
The following search terms wereused according to the PICO:
- clinical study
- human
- randomized clinical trial
- RCT
- Dental
- implant
- surgery
- flap
- flapless
- survival rate
- success rate
- failure
- bone loss
- marginal bone loss
- complication*
- pain
The search terms were grouped to the subjects (dental implants complications between flapped and flapless techniques) and linked with “AND” as follows:
A combination of relevant keywords was:
“Dental Implants ” [MeSH] AND “dentalimplants” AND “dent* implant* flap” AND [MeSH] AND “dent* implant* flapless” [MeSH] AND “dent* implant* flapless” technique AND bone loss.
Thereafter, the search results from the subject (two subjectgroups) were combined with each other using the Boolean Operator “OR.” An electronic search was complemented by manualsearching of the bibliographies/references of the most recent systematicreviewsand of all included publications.
In addition, the references of the included studies were search for further relevant studies.
Initial screening of titles and abstracts was carried out and full texts of the potentially eligible studies were obtained for further evaluation. Studies were included based on established inclusion/exclusion criteria by two reviewers separately. Disagreements were discussed with the third reviewer.
Data extraction
Relevant data including study methodology, number of patients, number of implants and mean length and diameter, mean age, and surgical procedure data including flapped or flapless technique, brand and type of implants, implant insertion site, and loading protocol as well as implant therapy outcome including follow up duration, success, failure and survival rates, marginal bone loss and other complications were extracted from each study.
This study was performed in compliance with the PRISMA statement (Liberati et al. 2009).
Data analysis/Statistical Methods
Included studies were evaluated in a qualitative manner and no statistical and meta-analyses were performed. Survival and success rate, alveolar bone loss and occurrence of complications between two techniques were compared between two techniques.
A descriptive analysis was performed.
Results
Search process
Study design is demonstrated in figure 1. Initial search in PubMed database resulted in 1529 studies. First, PubMed filters were applied to specify the results. Filters were used included: English language, Human, clinical trial, controlled trial. Filtering the search results resulted in 176 studies. Then, screening step through reviewing titles and abstracts was done. This step resulted in 38 studies out of which 21 studies were included after meticulous assessment of the full-texts based on inclusion and exclusion criteria.
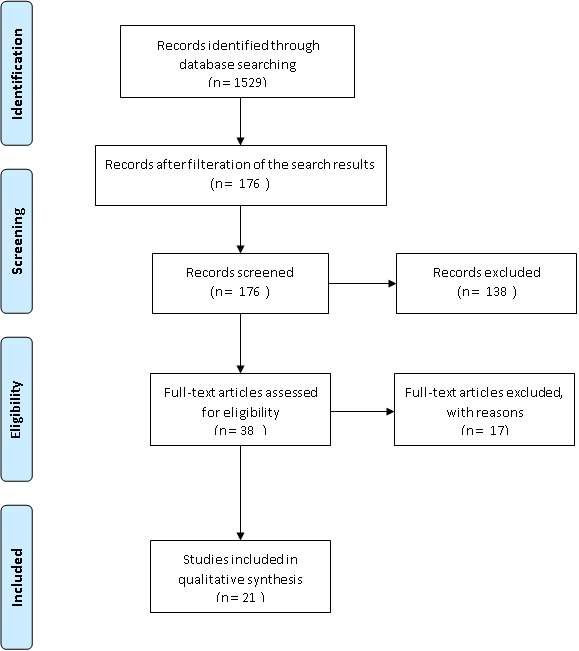
Figure 1
Method of the included studies
Among the included 21 included studies, 13 studies (Fortin et al. 2006, Oh et al. 2006, Ozan et al. 2007, Cannizzaro et al. 2008, Lindeboom and van Wijk 2010, Cannizzaro et al. 2011, Froum et al. 2011, Al-Juboori et al. 2012, Bashutski et al. 2013, Parmigiani-Izquierdo et al. 2013, Sunitha and Sapthagiri 2013, Tsoukaki et al. 2013) were randomized clinical trial (RCT) (Table 1). One study(Berdougo et al. 2010) was retrospective including 169 patients while other studies had prospective design.
Total number of patients
A total number of 1069 patients were evaluated in the included studies. Among them, 384, 516 and 169 ones were in RCTs, prospective and retrospective studies, respectively.
Age
The age of the patients ranged in between 18 to 86. Age range was not reported in two studies (Sunitha et al. 2008, Froum et al. 2011).
Gender
Only 3 studies (Job et al. 2008, Sunitha et al. 2008, Cannizzaro et al. 2011) did not mention the gender distribution in their study. In the other 18 studies a total of 564 females and a total of 449 male patients were included.
Surgical methods
Table 2 demonstrates number of implants and their features as well as implant insertion site and loading protocol.
Five studies(Becker et al. 2005, Oh et al. 2006, Becker et al. 2009, Nikzad and Azari 2010, Jeong et al. 2011) only used flapless surgical technique while comparison of flapless and flapped techniques was performed in the other 16 studies. In 9 trials(Fortin et al. 2006, Ozan et al. 2007, Cannizzaro et al. 2008, Berdougo et al. 2010, Lindeboom and van Wijk 2010, Nikzad and Azari 2010, Van de Velde et al. 2010, Froum et al. 2011, Bashutski et al. 2013), implant insertion was performed using computer guided equipment.
Implant specifics
One study (Parmigiani-Izquierdo et al. 2013) did not report exact number of the implants. A total number of 2331 implants were inserted in the other included studies. The length and diameter of implants ranged between 8 mm to 16 mm and 3.3 mm to 5 mm in 16 studies(Becker et al. 2005, Oh et al. 2006, Ozan et al. 2007, Cannizzaro et al. 2008, Job et al. 2008, Sunitha et al. 2008, Berdougo et al. 2010, Nikzad and Azari 2010, Van de Velde et al. 2010, Cannizzaro et al. 2011, Froum et al. 2011, Jeong et al. 2011, Al-Juboori et al. 2012, Bashutski et al. 2013, Sunitha and Sapthagiri 2013, Tsoukaki et al. 2013), respectively. All implants in the included studies had rough surface dental implant types.
The following implant systems were used in the selected studies.
- Swiss plus®
- Zimmer®
- ITI®
- Astra®
- Easy implant
- Nobel Biocare
- Single piece root
- Ostem
- Keystone
Site of implant insertion
13 studies (Becker et al. 2005, Oh et al. 2006, Ozan et al. 2007, Cannizzaro et al. 2008, Jeong et al. 2008, Berdougo et al. 2010, Lindeboom and van Wijk 2010, Nikzad and Azari 2010, Van de Velde et al. 2010, Jeong et al. 2011, Al-Juboori et al. 2012, Bashutski et al. 2013, Sunitha and Sapthagiri 2013) reported implant insertion site. In these studies, 1068 implants were inserted in the maxilla while 781 implants were inserted in the mandible.
Loading protocol
In the study of Job et al. (Job et al. 2008) all implants were loaded immediately and in three other studies (Oh et al. 2006, Cannizzaro et al. 2008, Van de Velde et al. 2010) immediate implant loading was only done using flapless technique. In other studies, implants were loaded following conventional protocols.
Implant success and survival rate
While no significant difference was found between success and survival rate of implants using two techniques, Jeong et al. (Jeong et al. 2008) reported higher success rate in flapless group.
Alveolar bone loss
7 studies(Becker et al. 2005, Job et al. 2008, Sunitha et al. 2008, Froum et al. 2011, Jeong et al. 2011, Sunitha and Sapthagiri 2013, Tsoukaki et al. 2013) reported higher marginal bone loss in flapped groups compared to flapless technique. However, the difference was not significant in 6 studies(Ozan et al. 2007, Jeong et al. 2008, Becker et al. 2009, Van de Velde et al. 2010, Cannizzaro et al. 2011, Al-Juboori et al. 2012).
Post-operative complications
Although in 6 studies (Fortin et al. 2006, Cannizzaro et al. 2008, Cannizzaro et al. 2011, Al-Juboori et al. 2012, Parmigiani-Izquierdo et al. 2013, Tsoukaki et al. 2013) less pain was reported following flapless technique, in study of Lindeboom et al. (Lindeboom and van Wijk 2010) Flapless group had more pain. In addition, less oedema in flapless group was reported by Cannizzaro et al. (Cannizzaro et al. 2008). Shorter surgical time using flapless technique was reported in two studies (Becker et al. 2005, Cannizzaro et al. 2011).
Discussion and Conclusion
Discussion
When lost teeth are going to be substituted by dental implants, several factors concerning dental implant properties and surgical and prosthetic methods should be considered to increase success rate of the treatment as well as patient satisfaction. The clinician should use proper materials and methods in each case. One of the important factors that could affect implant treatment outcome is sought to be flap design at the time of implant insertion (Brodala 2009, Doan et al. 2012). In clinical situations, the surgeon should choose between flapped and flapless approaches prior to the dental implant procedure. Each of these approaches has been reported to have its own advantages and disadvantages. While flapped technique permit visual evaluation of the insertion site (Bhat and Bangawala 2014), flapless approach is associated with less surgical time(Becker et al. 2005, Cannizzaro et al. 2011) and patient discomfort(al-Ansari and Morris 1998, Al-Juboori et al. 2012, Tsoukaki et al. 2013). However, in the recent dentistry, such clinical decision-making should be evidence based. Systematic reviews can provide reliable evidences through gathering information of previous isolated clinical trials.
The aim of the current study was to systematically review the articles comparing implant treatment outcome between flapped and flapless implant insertion techniques. The results were categorized based on implant survival rate, amount of marginal bone loss and post-operative complications. The results indicated no difference in implant survival rate while the flapless technique seemed to be associated with comparable or less marginal bone loss and less pain and discomfort. Previously, some studies have reviewed and compared these techniques and reported comparable outcome(Chrcanovic et al. 2014, Lin et al. 2014, Vohra et al. 2015).
Lin et al.(Lin et al. 2014) performed a meta-analysis for comparison of survival rate and marginal bone loss in flapped and flapless techniques. They included 12 studies with different designs and showed that the mean survival rate of implants in flapped and flapless techniques was 98.6% and 97%, respectively. When the difference was analysed considering study design, no statistically difference was found. Also comparison of the mean marginal bone loss showed a mean difference of 0.03 mm. This difference also was not statistically different between the two surgical techniques.
A systematic review by Chen et al. (Chen et al. 2004) showed similar survival rate and clinical outcome between implants inserted immediately and those inserted using delayed approached in healed sites. In the current review we did not consider implant site situation as an inclusion criterion. Therefore, implants inserted in fresh socket, augmented and healed sites were included. In review of Vohra et al. (Vohra et al. 2015) only studies that inserted dental implants in healed alveolar ridge were included. Including 10 studies, they showed that in half of the studies there was no difference in marginal bone loss two techniques while the other half reported less marginal bone loss in their flapless groups.
In comparison to other reviews(Lin et al. 2014, Vohra et al. 2015), a meta-analysis by Chrcanovic et al.(Chrcanovic et al. 2014) showed significantly higher implant survival rate in flapped group compared to the flapless group. They included 23 studies and reported odds ratio of implant failure in flapless technique compared to flapped technique was 1.75 (p=0.04). This means that implant placement using flapless technique increase risk of implant failure by 75%. The reason for this controversy might be due to the fact that in their review, all studies comparing implant treatment outcome between flapped and flapless technique were included regardless of sample size, study design and follow up period. They also compared post-operative complication of flapped and flapless techniques and showed no significant difference. Similar to the other reviews(Lin et al. 2014, Vohra et al. 2015), comparison of mean marginal bone loss between flapped and flapless techniques in study of Chrcanovic et al.(Chrcanovic et al. 2014) showed no significant difference.
A systematic review by Moraschini et al. (Moraschini et al. 2015) was performed on implant treatment outcome using flapless technique only. They included 13 studies form PubMed and Cochrane databases and revealed that flapless technique would result in 97.2% survival rate and a mean 1.45 mm marginal bone loss during 1-4 years of follow up. In their meta-analysis they included studies which placed more than 5 implants in each patient. They mentioned that surgical and prosthetic complications could happen using this technique and more studies are required to assess flapless technique more precisely. Other two reviews on outcome of dental implant treatment in flapless technique show 98.6% (Brodala 2009) and 97.1% (Doan et al. 2012) of survival rate and the rate of post-operative complication in this technique to be 3.8% (Brodala 2009) and 6.55% (Doan et al. 2012).
Regarding the level of evidence, 13(Fortin et al. 2006, Oh et al. 2006, Ozan et al. 2007, Cannizzaro et al. 2008, Lindeboom and van Wijk 2010, Cannizzaro et al. 2011, Froum et al. 2011, Al-Juboori et al. 2012, Bashutski et al. 2013, Parmigiani-Izquierdo et al. 2013, Sunitha and Sapthagiri 2013, Tsoukaki et al. 2013) out of 21 reviewed studieswere randomized clinical trials (RCTs). The exclusive results of these studies were similar to the results of all studies combined. In RCTs, No difference in implant survival rate between both techniques were found. ThreeRCTs(Froum et al. 2011, Sunitha and Sapthagiri 2013, Tsoukaki et al. 2013) reported higher marginal bone loss in flapped groups compared to flapless technique while the difference was not significant in 4 RCTs(Ozan et al. 2007, Van de Velde et al. 2010, Cannizzaro et al. 2011, Al-Juboori et al. 2012). All 6 studies that reported less post-operative pain in flapless approach(Fortin et al. 2006, Cannizzaro et al. 2008, Cannizzaro et al. 2011, Al-Juboori et al. 2012, Parmigiani-Izquierdo et al. 2013, Tsoukaki et al. 2013)were RCTs. However, study of Lindeboom et al. (Lindeboom and van Wijk 2010)who shoed flapless group had more pain was also performed as RCT. Less oedema in flapless group was reported in RCT by Cannizzaro et al. (Cannizzaro et al. 2008) and shorter surgical time using flapless technique was reported in another RCT by Cannizzaro et al. (Cannizzaro et al. 2011).
Some factors could influence implant treatment outcome which were not considered in this review. Soft tissue biotype in an influential factor as facial bone loss in thick biotypes is less than 1 mm while it is 1-1.5 mm in thin biotypes . Also, oral hygiene has an important role in the success of dental implant treatment (Serino et al. 2015) which was not considered in included studies. A definitive factor which could influence survival rate of dental implants is smoking. Marginal bone loss has been demonstrated to be more in smokers compared to non-smokers (Vervaeke et al. 2012). It has been stated that survival rate of implant for non-smokers and smokers using flapless technique is 98.9% and 81.2%, respectively . Also, the corresponding numbers for marginal bone loss was 1.2 and 2.6 mm, respectively . However, none of the reviewed studies reported implant treatment outcome in flapped and flapless groups based on smoking of the patients.Finally, the experience of the surgeon also could influence treatment outcome (Cushen and Turkyilmaz 2013) as some surgeons may be more skilful in flapped technique while others may prefer flapless technique.
The results of this review could be interpreted into clinical situations considering the inclusion criteria of the reviewed studies. The results indicated comparable clinical outcome of both techniques. In the included RCTs, the healthy patients who needed implant insertion in alveolar bone without augmentation were enrolled. In these situations, the surgeon is free to choose between both techniques. The results of this review could not be used in cases with compromised conditions, systemic diseases or those with insufficient bone at the recipients site.
The limitations of this systematic review should also be considered. The number of RCTs were low (n=13). Also, the method of the studies including study design, duration and periods of follow ups, protocols for loading dental implants, insertion of dental implants in healed, fresh socket or augmented sites, smoking, and implant site, were different. In addition, included studies assess marginal bone loss by comparing periapical radiographs. However, this technique might not be able to properly show amount of facial bone loss. Finally, this review only included studies in English language and is prone to publication bias.
Conclusion
Considering the limitations of this systematic review, the results could be summarized as follows:
- There was no significant difference in success and survival rate of implants between two techniques except for one study that reported higher success rate in flapless group. Therefore, implant survival rate using flapped and flapless technique is comparable.
- 7 studies reported higher marginal bone loss in flapped groups compared to flapless technique. Three of these studies were RTCs. However, the difference was not significant in 6 studies and four of them RCTs. So, marginal bone loss using flapless technique is similar or less than flapped technique.
- Less post-operative pain in flapless group compared to flapped group was reported in 6 RCTs while flapless group had more pain in another RCT. Less oedema in flapless group was reported in a RCT. Therefore, it seems that flapless technique would probably have less post-operative pain and oedema.
- Shorter surgical time using flapless technique was reported in two studies and one RCT.
Future outlook
Further well designed randomized controlled trials should be performed with longer follow ups and larger sample size to further investigate this issue. It is suggested to consider patient hygiene, smoking, soft tissue biotype, previous procedures on the recipient site, protocols for loading dental implants, and implant site. Future studies should be performed to investigate the effect of the aforementioned factors on implant treatment outcome and compare implant success rate, marginal bone loss and rate of complications between flapped and flapless groups considering these factors. Also, it is suggested to perform RCTs measuring amount of facial bone loss using cone beam computed tomography (CBCT) considering ethical issues.
References
Abd El Salam, E. A. (2007) Immediate Aesthetic Implant Therapy (Ch. 6). Fundamentals of Aesthetic Implant Dentistry second ed.:179-207.
al-Ansari, B. H. and R. R. Morris (1998) Placement of dental implants without flap surgery: a clinical report. Int J Oral Maxillofac Implants. 13(6):861-865.
Al-Juboori, M. J., S. Bin Abdulrahaman and A. Jassan (2012) Comparison of flapless and conventional flap and the effect on crestal bone resorption during a 12-week healing period. Dent Implantol Update. 23(2):9-16.
Bashutski, J. D., H. L. Wang, I. Rudek, I. Moreno, T. Koticha and T. J. Oh (2013) Effect of flapless surgery on single-tooth implants in the esthetic zone: a randomized clinical trial. J Periodontol. 84(12):1747-1754.
Becker, W., M. Goldstein, B. E. Becker and L. Sennerby (2005) Minimally invasive flapless implant surgery: a prospective multicenter study. Clin Implant Dent Relat Res. 7 Suppl 1:S21-27.
Becker, W., M. Goldstein, B. E. Becker, L. Sennerby, D. Kois and P. Hujoel (2009) Minimally invasive flapless implant placement: follow-up results from a multicenter study. J Periodontol. 80(2):347-352.
Behnia, H., S. R. Motamedian, M. T. Kiani, G. Morad and A. Khojasteh (2015) Accuracy and reliability of cone beam computed tomographic measurements of the bone labial and palatal to the maxillary anterior teeth. Int J Oral Maxillofac Implants. 30(6):1249-1255.
Berdougo, M., T. Fortin, E. Blanchet, M. Isidori and J. L. Bosson (2010) Flapless implant surgery using an image-guided system. A 1- to 4-year retrospective multicenter comparative clinical study. Clin Implant Dent Relat Res. 12(2):142-152.
Bhat, V. and M. R. Bangawala (2014) Immediate implant placement without flap elevation-a review. Nitte University Journal of Health Science. 4(3):131.
Brodala, N. (2009) Flapless surgery and its effect on dental implant outcomes. Int J Oral Maxillofac Implants. 24 Suppl:118-125.
Campelo, L. and J. Camara (2002) Flapless implant surgery: A 10-year clinical retrospective analysis. Int J Oral Maxillofac Implants. 17:271-276.
Cannizzaro, G., P. Felice, M. Leone, V. Checchi and M. Esposito (2011) Flapless versus open flap implant surgery in partially edentulous patients subjected to immediate loading: 1-year results from a split-mouth randomised controlled trial. Eur J Oral Implantol. 4(3):177-188.
Cannizzaro, G., M. Leone, U. Consolo, V. Ferri and M. Esposito (2008) Immediate functional loading of implants placed with flapless surgery versus conventional implants in partially edentulous patients: a 3-year randomized controlled clinical trial. Int J Oral Maxillofac Implants. 23(5):867-875.
Cecchinato, D., D. Lops, G. E. Salvi and M. Sanz (2015) A prospective, randomized, controlled study using OsseoSpeed implants placed in maxillary fresh extraction socket: soft tissues response. Clin Oral Implants Res. 26(1):20-27.
Chen, S. T., I. B. Darby, E. C. Reynolds and J. G. Clement (2009) Immediate implant placement postextraction without flap elevation. J Periodontol. 80(1):163-172.
Chen, S. T., T. G. Wilson, Jr. and C. H. Hammerle (2004) Immediate or early placement of implants following tooth extraction: review of biologic basis, clinical procedures, and outcomes. Int J Oral Maxillofac Implants. 19 Suppl:12-25.
Chrcanovic, B. R., T. Albrektsson and A. Wennerberg (2014) Flapless versus conventional flapped dental implant surgery: a meta-analysis. PLoS ONE. 9(6):e100624.
Costich, E. and S. Ramfjord (1968) Healing after partial denudation of the alveolar process. J Periodontol. 39:127-134.
Cosyn, J., M. Sabzevar and H. De Bruyn (2012) Predictors of interproximal and midfacial recession following single implant treatment in the anterior maxilla: A multivariate analysis. J Clin Periodontol. 39:895-903.
Cushen, S. E. and I. Turkyilmaz (2013) Impact of operator experience on the accuracy of implant placement with stereolithographic surgical templates: an in vitro study. J Prosthet Dent. 109(4):248-254.
Doan, N., Z. Du, R. Crawford, P. Reher and Y. Xiao (2012) Is flapless implant surgery a viable option in posterior maxilla? A review. Int J Oral Maxillofac Surg. 41(9):1064-1071.
Eroglu, C. N., A. S. Ertugrul, M. Eskitascioglu and G. Eskitascioglu (2016) Changes in the surface of bone and acid-etched and sandblasted implants following implantation and removal. Eur J Dent. 10(1):77-81.
Fortin, T., J. L. Bosson, M. Isidori and E. Blanchet (2006) Effect of flapless surgery on pain experienced in implant placement using an image-guided system. Int J Oral Maxillofac Implants. 21(2):298-304.
Froum, S. J., S. C. Cho, N. Elian, G. Romanos, Z. Jalbout, M. Natour, et al. (2011) Survival rate of one-piece dental implants placed with a flapless or flap protocol–a randomized, controlled study: 12-month results. Int J Periodontics Restorative Dent. 31(6):591-601.
Jeong, S. M., B. H. Choi, J. Kim, F. Xuan, D. H. Lee, D. Y. Mo, et al. (2011) A 1-year prospective clinical study of soft tissue conditions and marginal bone changes around dental implants after flapless implant surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 111(1):41-46.
Jeong, S. M., B. H. Choi, J. Li, K. M. Ahn, S. H. Lee and F. Xuan (2008) Bone healing around implants following flap and mini-flap surgeries: a radiographic evaluation between stage I and stage II surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 105(3):293-296.
Job, S., V. Bhat and E. M. Naidu (2008) In vivo evaluation of crestal bone heights following implant placement with ‘flapless’ and ‘with-flap’ techniques in sites of immediately loaded implants. Indian J Dent Res. 19(4):320-325.
Jokstad, A., U. Braegger, J. B. Brunski, A. B. Carr, I. Naert and A. Wennerberg (2003) Quality of dental implants. Int Dent J. 53(6 Suppl 2):409-443.
Katsoulis, J., M. Avrampou and C. Spycher (2012) Comparison of implant stability by means of resonance frequency analysis for flapless and conventionally inserted implants. Clin Implant Dent Relat Res. 14:915-923.
Khorsand, A., A. A. Rasouli-Ghahroudi, N. Naddafpour, Y. S. Shayesteh and A. Khojasteh (2016) Effect of Microthread Design on Marginal Bone Level Around Dental Implants Placed in Fresh Extraction Sockets. Implant Dent. 25(1):90-96.
Liberati, A., D. G. Altman, J. Tetzlaff, C. Mulrow, P. C. Gotzsche, J. P. Ioannidis, et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 151(4):W65-94.
Lin, G. H., H. L. Chan, J. D. Bashutski, T. J. Oh and H. L. Wang (2014) The effect of flapless surgery on implant survival and marginal bone level: a systematic review and meta-analysis. J Periodontol. 85(5):e91-103.
Lindeboom, J. A. and A. J. van Wijk (2010) A comparison of two implant techniques on patient-based outcome measures: a report of flapless vs. conventional flapped implant placement. Clin Oral Implants Res. 21(4):366-370.
Morad, G., H. Behnia, S. R. Motamedian, S. Shahab, P. Gholamin, K. Khosraviani, et al. (2014) Thickness of labial alveolar bone overlying healthy maxillary and mandibular anterior teeth. J Craniofac Surg. 25(6):1985-1991.
Moraschini, V., G. Velloso, D. Luz and E. P. Barboza (2015) Implant survival rates, marginal bone level changes, and complications in full-mouth rehabilitation with flapless computer-guided surgery: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 44(7):892-901.
Nikzad, S. and A. Azari (2010) Custom-made radiographic template, computed tomography, and computer-assisted flapless surgery for treatment planning in partial edentulous patients: a prospective 12-month study. J Oral Maxillofac Surg. 68(6):1353-1359.
Oh, T. J., J. L. Shotwell, E. J. Billy and H. L. Wang (2006) Effect of flapless implant surgery on soft tissue profile: a randomized controlled clinical trial. J Periodontol. 77(5):874-882.
Ormianer, Z. and A. Palti (2006) Long-term clinical evaluation of tapered multi-threaded implants: results and influences of potential risk factors. J Oral Implantol. 32(6):300-307.
Ozan, O., I. Turkyilmaz and B. Yilmaz (2007) A preliminary report of patients treated with early loaded implants using computerized tomography-guided surgical stents: flapless versus conventional flapped surgery. J Oral Rehabil. 34(11):835-840.
Parmigiani-Izquierdo, J. M., A. Sanchez-Perez and M. E. Cabana-Munoz (2013) A pilot study of postoperative pain felt after two implant surgery techniques: a randomized blinded prospective clinical study. Int J Oral Maxillofac Implants. 28(5):1305-1310.
Sanna, A., L. Molly and D. van Steenberghe (2007) Immediately loaded CAD-CAM manufactured fixed complete dentures using flapless implant placement procedures: A cohort study of consecutive patients. J Prosthet Dent. 97:331-339.
Scala, R., P. Ghensi, A. Cucchi and E. Pistoia (2012) Postextraction implant placement with immediate provisionalisation and finalisation, using a simplified technique: technical notes and a case report. Open Dent J. 6:164-169.
Schwartz-Arad, D. and G. Chaushu (1997) Placement of implants into fresh extraction sites: 4 to 7 years retrospective evaluation of 95 immediate implants. J Periodontol. 68(11):1110-1116.
Serino, G., A. Turri and N. P. Lang (2015) Maintenance therapy in patients following the surgical treatment of peri-implantitis: a 5-year follow-up study. Clin Oral Implants Res. 26(8):950-956.
Stoupel, J., C. T. Lee, J. Glick, E. Sanz-Miralles, C. Chiuzan and P. N. Papapanou (2016) Immediate implant placement and provisionalization in the aesthetic zone using a flapless or a flap-involving approach: a randomized controlled trial. J Clin Periodontol. 43(12):1171-1179.
Summers, R. B. (1994) A new concept in maxillary implant surgery: the osteotome technique. Compend Contin Educ Vet. 15(2):152, 154-156, 158 passim; quiz 162.
Sunitha, R. V., T. Ramakrishnan, S. Kumar and P. Emmadi (2008) Soft tissue preservation and crestal bone loss around single-tooth implants. J Oral Implantol. 34(4):223-229.
Sunitha, R. V. and E. Sapthagiri (2013) Flapless implant surgery: a 2-year follow-up study of 40 implants. Oral Surg Oral Med Oral Pathol Oral Radiol. 116(4):e237-243.
TC, S., I. BD, E. CR and J. GC. (2009) Case series Immediate Implant Placement Postextraction Without Flap Elevation. J Clin Periodontol. 80:163-172.
Tsoukaki, M., C. D. Kalpidis, D. Sakellari, L. Tsalikis, G. Mikrogiorgis and A. Konstantinidis (2013) Clinical, radiographic, microbiological, and immunological outcomes of flapped vs. flapless dental implants: a prospective randomized controlled clinical trial. Clin Oral Implants Res. 24(9):969-976.
Van de Velde, T., L. Sennerby and H. De Bruyn (2010) The clinical and radiographic outcome of implants placed in the posterior maxilla with a guided flapless approach and immediately restored with a provisional rehabilitation: a randomized clinical trial. Clin Oral Implants Res. 21(11):1223-1233.
Vervaeke, S., B. Collaert, S. Vandeweghe, J. Cosyn, E. Deschepper and H. De Bruyn (2012) The effect of smoking on survival and bone loss of implants with a fluoride-modified surface: a 2-year retrospective analysis of 1106 implants placed in daily practice. Clin Oral Implants Res. 23(6):758-766.
Vohra, F., A. A. Al-Kheraif, K. Almas and F. Javed (2015) Comparison of crestal bone loss around dental implants placed in healed sites using flapped and flapless techniques: a systematic review. J Periodontol. 86(2):185-191.
Appendix
Certificate of Approval
MASTER’S THESIS
at the
J. W. Goethe University
Frankfurt am Main
This is to certify that the Master thesis of
Dr. Shahrokh Bozorg
With the Title
A Systematic Review of Dental Implant Placement with Flapless and Flapped Technique
has been approved by the Examination Committee
for the thesis requirement for the Master of Science
in Oral Implantology
Examinations Committee:
____________________________________________
Accredited Tutor (Name of Tutor)
____________________________________________
Prof. Dr. J. Pfeilschifter
____________________________________________
Dr. P. Weigl
____________________________________________
Source: UKDiss.com

