The vitality of a tooth refers to its health and function, determined primarily by the status of its pulp—the living part of the tooth containing nerves, blood vessels, and connective tissues. Tooth vitality is a key component of overall oral health, as it affects not only the tooth’s structural integrity but also its ability to respond to stimuli and infections. Understanding the vitality of teeth is essential in diagnosing dental diseases, determining the appropriate treatment, and preventing further complications. Vitality tests, therefore, serve a crucial role in clinical dentistry.
This article aims to provide an in-depth exploration of tooth vitality, including the anatomy and function of the dental pulp, causes of vitality loss, and various methods for testing vitality, as well as the clinical implications of these tests.
Table of Contents
ToggleAnatomy of the Tooth and Its Vital Components
A human tooth consists of several layers, each serving distinct functions. These include:
- Enamel: The outermost layer, which is highly mineralized and protects the tooth from wear and decay.
- Dentin: Located beneath the enamel, dentin is less mineralized but still firm, forming the bulk of the tooth structure.
- Pulp: The innermost layer of the tooth, where the blood vessels, nerves, and connective tissues are located. The pulp is essential for the tooth’s vitality.
The Role of the Dental Pulp
The pulp is the living core of the tooth and serves multiple functions:
- Sensory: The pulp contains nerves that respond to various stimuli, such as temperature changes and pressure.
- Nutritive: The pulp supplies nutrients to the tooth through its blood vessels, ensuring that the tooth stays healthy and can repair minor damages.
- Protective: When bacteria invade the tooth, the pulp initiates an immune response to protect against infection.
- Formative: The pulp contributes to the development and formation of dentin throughout the tooth’s life.
Any disruption in the function of the pulp, whether due to trauma, infection, or decay, can impair the tooth’s vitality, potentially leading to tooth death if not treated promptly.
Tooth Vitality vs. Tooth Viability
It’s important to distinguish between vitality and viability when discussing dental health. Tooth vitality refers to the ability of the tooth’s pulp to perform its functions, whereas tooth viability simply refers to the survival of the dental pulp’s cells. A tooth may be viable (i.e., still have living cells in the pulp) but not vital if the cells are not functioning properly.
This distinction becomes relevant when assessing the prognosis of dental treatments. For example, a tooth that has experienced significant trauma may have viable cells but lack proper function due to nerve damage. In such cases, dental vitality testing becomes crucial for determining the appropriate course of action.
Causes of Loss of Tooth Vitality
Tooth vitality can be compromised due to several factors, including physical trauma, infections, dental decay, and iatrogenic causes. Understanding these causes helps clinicians make informed decisions during vitality testing.
- Dental Decay
- Trauma
- Dental Procedures
- Periodontal Disease
- Age-Related Changes
- Pulpitis and Necrosis
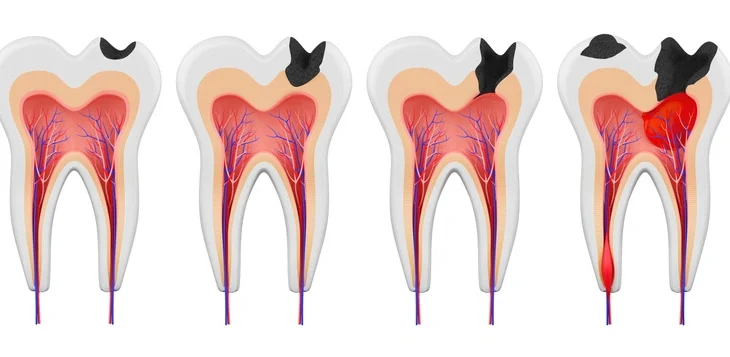
Dental Decay
Dental caries, or cavities, result from bacterial infection in the mouth. When untreated, tooth decay penetrates the enamel and dentin layers, eventually reaching the pulp. This exposure to bacteria can cause inflammation (pulpitis), which, if left untreated, may lead to necrosis of the pulp.
Trauma
Physical trauma to the tooth, such as from a blow to the face or sports injury, can cause the pulp to become damaged or severed from its blood supply. This can lead to partial or complete loss of tooth vitality, depending on the severity of the trauma.
Dental Procedures
Sometimes, dental procedures such as deep restorations or root canal treatments can inadvertently damage the pulp, leading to vitality loss. Excessive heat or pressure during procedures can traumatize the pulp, compromising its ability to function.
Periodontal Disease
Severe gum disease can also affect tooth vitality. As periodontal disease progresses, the infection can reach the tooth root, damaging the blood vessels and nerves that keep the pulp vital. This connection between the pulp and the surrounding tissues is essential for the health of the tooth.
Age-Related Changes
With aging, the dental pulp can become smaller due to the continuous deposition of dentin. This natural process can reduce the tooth’s ability to respond to vitality tests, though it may still be technically “alive.”
Pulpitis and Necrosis
- Reversible Pulpitis: Inflammation of the pulp can sometimes be treated, and the vitality can be restored. The tooth may remain sensitive but otherwise healthy.
- Irreversible Pulpitis: In cases of severe inflammation, irreversible damage occurs, often leading to pulp necrosis (death). A necrotic pulp is non-vital, requiring further intervention, such as root canal therapy or extraction.
Importance of Tooth Vitality Testing
Vitality testing is essential in the diagnosis and management of dental issues. Determining the vitality of a tooth allows clinicians to assess whether the pulp is healthy, inflamed, or necrotic, and make decisions regarding necessary treatments, such as root canals, pulp capping, or extractions.
Vitality tests are commonly performed in several clinical situations:
- Pulpal diagnosis
- Preoperative assessment
- Trauma cases
Pulpal diagnosis
When patients report pain or sensitivity, vitality tests help pinpoint whether the tooth’s pulp is healthy, inflamed, or necrotic.
Preoperative assessment
Before performing invasive procedures, clinicians often test tooth vitality to ensure that the tooth can survive the treatment.
Trauma cases
Following dental trauma, vitality tests help in assessing the damage to the pulp and guide treatment planning.
Types of Tooth Vitality Tests
There are several methods used to assess tooth vitality, each with its advantages and limitations. These can be categorized into three primary types:
- Sensitivity Tests
- Blood Flow Tests
- Radiographic Examination
Sensitivity Tests
Sensitivity tests assess the tooth’s response to stimuli that typically cause a reaction in a healthy pulp. These include:
- Thermal Testing
- Electric Pulp Test (EPT)
- Mechanical Stimulation
Thermal Testing
Thermal testing involves applying either heat or cold to the tooth and observing the patient’s response. The logic is that a vital tooth will respond to temperature changes due to the presence of live nerve fibers in the pulp.
- Cold Test: A cold stimulus, such as ice or ethyl chloride spray, is applied to the tooth. A vital tooth will respond with a brief sensation, while a non-vital tooth may show no response or only a prolonged painful sensation, indicative of irreversible pulpitis.
- Heat Test: Heat stimuli, often using heated gutta-percha or other devices, are applied to the tooth. A delayed or painful response suggests pulpitis, while a lack of response may indicate necrosis.
Electric Pulp Test (EPT)
The electric pulp test delivers a small electrical current to the tooth to stimulate the nerves within the pulp. The patient reports any sensation of tingling or discomfort. While effective, this test has limitations, as it may produce false positives in some cases, such as when the current affects surrounding tissues or restorations.
EPT may not always give accurate results for teeth with calcified pulp chambers, immature teeth with underdeveloped roots, or teeth that have been recently traumatized.
Mechanical Stimulation
In some cases, mechanical stimulation, such as tapping or applying pressure, is used to assess the vitality of a tooth. A vital tooth may respond with a slight discomfort, while a non-vital tooth will often not elicit any sensation. This method is often combined with other tests to improve accuracy.
Blood Flow Tests
Unlike sensitivity tests, which rely on nerve response, blood flow tests aim to directly measure the blood supply to the pulp. Since the pulp is vascularized, assessing blood flow is a more direct indication of vitality.
- Laser Doppler Flowmetry (LDF)
- Pulse Oximetry
- Spectrophotometry
Laser Doppler Flowmetry (LDF)
Laser Doppler Flowmetry is a non-invasive technique that uses a low-powered laser beam to measure blood flow within the tooth. The device detects shifts in the frequency of laser light reflected from moving red blood cells within the pulp’s vasculature, providing a more objective measure of pulp vitality. LDF is considered highly accurate, particularly for assessing the vitality of immature or traumatized teeth where sensitivity tests may be unreliable.
- Advantages: LDF is safe, non-invasive, and provides continuous monitoring of blood flow. It is particularly useful for testing teeth with open apices or those undergoing orthodontic treatment.
- Limitations: This test requires specialized equipment and is sensitive to movement, which can result in inaccurate readings.
Pulse Oximetry
Pulse oximetry, commonly used in medicine to measure oxygen saturation levels in the blood, can also be adapted for dental use. By placing a sensor on the tooth, pulse oximeters can detect the oxygen levels in the blood supply to the pulp, providing an indication of vitality. This test is promising, though not widely used in routine dental practice.
Spectrophotometry
Spectrophotometry is another method for evaluating pulp blood flow by analyzing light absorption characteristics of the pulp’s blood vessels. Like LDF, this test measures the amount of blood circulating in the tooth’s pulp. However, its clinical application is still under investigation, and it is not commonly used in practice.
Radiographic Examination
Though not a vitality test per se, radiographic imaging is an important adjunct in assessing tooth vitality. X-rays can reveal the condition of the surrounding bone, the size and shape of the pulp chamber, and any periapical pathology, all of which are useful in diagnosing pulp health.
Cone Beam Computed Tomography (CBCT)
Advanced imaging technologies like Cone Beam Computed Tomography (CBCT) offer a more detailed view of the tooth and its surrounding structures. CBCT provides three-dimensional imaging, which can help in assessing the extent of damage or infection, especially in complex cases such as root fractures, periapical lesions, or determining the success of previous treatments like root canals.
Limitations of Vitality Testing
While vitality tests are invaluable for diagnosing dental conditions, they are not without limitations. Several factors can influence the accuracy of these tests, including:
- Patient Variability
- False Positives and False Negatives
- Effect of Age
- Dental Restorations
- Traumatized Teeth
Patient Variability
Pain threshold varies significantly among individuals, making it difficult to interpret responses to sensitivity tests uniformly.
Patients with anxiety or those who have experienced trauma may have exaggerated or muted responses to stimuli.
False Positives and False Negatives
False Positive:
A tooth may test as vital despite having a necrotic pulp. This can occur in teeth with multi-rooted canals where one canal remains vital while others are necrotic. Electrical interference from restorations or adjacent teeth can also cause false positive responses.
False Negative:
A tooth may appear non-vital when it is, in fact, vital. This often occurs in teeth with immature roots or in cases of recent trauma where the pulp has a temporary lack of response due to nerve damage or inflammation. Teeth with calcified pulps also pose diagnostic challenges, as they may not respond to sensitivity testing.
Effect of Age
As teeth age, the pulp chamber reduces in size due to the continuous deposition of secondary dentin. Older teeth may have calcified pulps, making them less responsive to vitality tests, even though the pulp tissue may still be viable.
Dental Restorations
Teeth with extensive restorations, crowns, or root canals may interfere with the electrical and thermal conductivity of the pulp, affecting the accuracy of sensitivity tests.
Traumatized Teeth
Teeth that have recently experienced trauma may not respond to vitality tests due to temporary damage to the nerve fibers, even if the pulp is still vital. In such cases, a period of observation is often recommended before repeating the vitality test.
Interpretation of Test Results
When interpreting the results of vitality tests, clinicians must consider multiple factors, including the patient’s history, clinical examination, and radiographic findings. A combination of tests is often more reliable than relying on a single test. For example, if a cold test produces a positive response and radiographic examination reveals no periapical pathology, the tooth can generally be considered vital. Conversely, a negative response to multiple tests, along with radiographic evidence of bone loss or other pathology, strongly suggests pulp necrosis.
The results of vitality testing are usually classified into the following categories:
- Normal Response
- Hypersensitivity
- Delayed or Prolonged Response
- No Response
Normal Response
The tooth responds to stimuli with a brief sensation, indicating a healthy pulp.
Hypersensitivity
The tooth responds with exaggerated pain that lingers, suggesting pulpitis, which may be reversible or irreversible depending on the severity and duration of symptoms.
Delayed or Prolonged Response
A tooth that shows delayed or prolonged sensitivity to cold or heat may be indicative of irreversible pulpitis, requiring intervention such as root canal therapy.
No Response
The absence of any response to thermal or electrical stimuli usually indicates pulp necrosis or a non-vital tooth. However, this result must be corroborated with other findings to rule out factors like calcified pulp chambers.
Clinical Implications of Vitality Testing
Vitality testing plays a significant role in determining the appropriate treatment for various dental conditions. The results of these tests guide clinicians in deciding between conservative treatments, such as pulp capping or pulpotomy, versus more invasive procedures, like root canal therapy or tooth extraction.
Root Canal Therapy
When a tooth is determined to have irreversible pulpitis or necrosis, root canal therapy is the standard treatment. This procedure involves removing the diseased pulp, cleaning and shaping the root canals, and sealing the tooth to prevent reinfection. Vitality testing helps confirm the need for root canal treatment by demonstrating that the pulp is non-vital and cannot be salvaged.
Pulp Capping and Pulpotomy
In cases where the pulp is inflamed but not necrotic, conservative treatments like pulp capping or pulpotomy may be performed to preserve pulp vitality. These procedures are typically used in young patients with developing teeth, where maintaining a vital pulp is critical for the continued growth and development of the tooth. Vitality tests are essential in determining the health of the pulp and the likelihood of success with these treatments.
- Pulp Capping: This procedure is used when the pulp is exposed or nearly exposed due to decay or trauma. A protective material, such as calcium hydroxide or mineral trioxide aggregate (MTA), is applied to promote healing and preserve the pulp’s vitality.
- Pulpotomy: In this procedure, the coronal portion of the pulp is removed while the remaining pulp in the root canal is left intact. This is often used in pediatric dentistry for the treatment of primary teeth or immature permanent teeth with pulpitis.
Tooth Extraction
If vitality tests indicate that the tooth is non-vital and root canal therapy is not feasible or indicated, extraction may be necessary. This is particularly common in cases of severe infection, extensive decay, or fractures that compromise the tooth’s structural integrity.
Endodontic Retreatment
In some cases, teeth that have previously undergone root canal therapy may show signs of pathology, such as periapical lesions or persistent symptoms. Vitality testing in such cases, combined with radiographic evidence, helps determine whether endodontic retreatment or surgical intervention is needed.
Recent Advances in Vitality Testing
Technological advancements have introduced more precise and less invasive methods for evaluating tooth vitality. These innovations aim to improve diagnostic accuracy and reduce patient discomfort.
Ultrasound Doppler Flowmetry
Similar to Laser Doppler Flowmetry, ultrasound Doppler flowmetry measures blood flow in the tooth’s pulp. This technique uses ultrasound waves to detect movement within the pulp’s vasculature. Although not yet widely available in dental clinics, it holds promise as an alternative to LDF, particularly in its ability to overcome some of the limitations of laser-based systems.
Thermography
Thermography is a novel approach that uses infrared technology to measure temperature changes in the tooth surface. This method detects the thermal response of the tooth to environmental changes, providing insights into pulp vitality. Though still experimental, thermography offers the potential for non-contact, non-invasive testing, which could be particularly useful in pediatric or special-needs populations.
Molecular Markers
Research is ongoing into the use of molecular markers to assess pulp health. These markers, found in the blood flow or the pulp itself, could offer a more precise method of determining the vitality of the pulp by identifying specific biochemical changes associated with inflammation, necrosis, or healing.
Frequently Asked Questions (FAQs)
What is vitality testing on teeth?
Vitality testing assesses the health of a tooth’s pulp to determine whether it is alive and functioning properly. This is crucial for diagnosing potential pulp diseases, infections, or trauma that may require treatment such as root canal therapy or extraction.
How to measure vitality of a tooth?
Vitality of a tooth is measured using various tests, including thermal tests (cold and heat), electric pulp testing, and laser Doppler flowmetry. Cold testing involves applying a cold stimulus to the tooth to check for a response, while heat testing evaluates delayed or exaggerated responses. Electric pulp testing sends a small electrical current to determine nerve activity. Laser Doppler flowmetry and pulse oximetry assess blood flow, providing a more reliable indicator of true vitality.
What is the difference between vitality and sensibility testing?
Vitality testing evaluates the actual blood flow and health of the pulp, which directly indicates whether the pulp tissue is alive. In contrast, sensibility testing assesses the nerve response to stimuli (such as cold, heat, or electric pulses), which can sometimes give false-positive results if nerve fibers are still responsive despite the pulp being necrotic or inflamed.
What is the most reliable tooth vitality test?
Laser Doppler flowmetry and pulse oximetry are considered the most reliable methods for assessing true pulp vitality, as they measure blood flow rather than nerve response. Unlike traditional thermal or electric pulp testing, these methods provide a direct assessment of whether oxygenated blood is circulating within the pulp tissue.
How is vitality calculated?
Vitality is not directly calculated through a numerical score but is assessed through a combination of clinical tests that evaluate pulp blood flow and nerve response. These assessments help dentists determine whether a tooth is healthy, inflamed, or necrotic.
What is the best test for vitality of a crowned tooth?
The best test for a crowned tooth is laser Doppler flowmetry or pulse oximetry, as traditional thermal and electric pulp tests may be less effective due to the insulating material of the crown. If these advanced methods are unavailable, other techniques like selective anesthesia or radiographic evaluation may provide supplementary information about the tooth’s condition.
What is a vitality test for primary teeth?
Vitality tests for primary teeth typically include thermal testing, electric pulp testing (though less commonly used due to unreliable results in children), and pulse oximetry. Because primary teeth have a different pulp structure and response compared to permanent teeth, dentists may also rely on clinical examination, radiographs, and signs of infection when assessing their vitality.
How many vitality points do you need for a dental check-up?
There is no specific “vitality points” system for dental check-ups. Instead, dentists use clinical tests to assess pulp health and determine if treatment is needed. The assessment considers factors like pain response, radiographic findings, and clinical symptoms to diagnose and manage dental conditions effectively.
Conclusion
Tooth vitality is a critical factor in maintaining oral health, as it ensures that the pulp, the living core of the tooth, remains functional and healthy. Vitality testing is an essential diagnostic tool in dentistry, aiding clinicians in assessing the health of the pulp and guiding treatment decisions. From traditional sensitivity tests to advanced technologies like Laser Doppler Flowmetry and pulse oximetry, there are a variety of methods available to evaluate tooth vitality.
Despite the limitations of current vitality testing methods, ongoing advancements in technology promise to improve diagnostic accuracy and patient outcomes. By understanding and applying vitality tests effectively, dental professionals can offer targeted, effective treatments that preserve tooth structure, promote oral health, and enhance the patient’s overall well-being.