Tooth eruption is a fascinating process that marks significant milestones in human development. It is a complex physiological phenomenon governed by a myriad of factors, including genetics, hormonal regulation, and cellular interactions. In this article, we delve into the intricate mechanisms behind tooth eruption, exploring the stages, key players, and the underlying biology that orchestrates this fundamental aspect of oral health.
Table of Contents
ToggleStages of Tooth Eruption
To understand tooth eruption, it’s essential to comprehend the stages through which teeth emerge into the oral cavity. The process typically begins during prenatal development, with the formation of tooth buds. These buds, composed of specialized cells derived from the dental lamina, eventually give rise to the primary dentition, also known as deciduous or baby teeth.
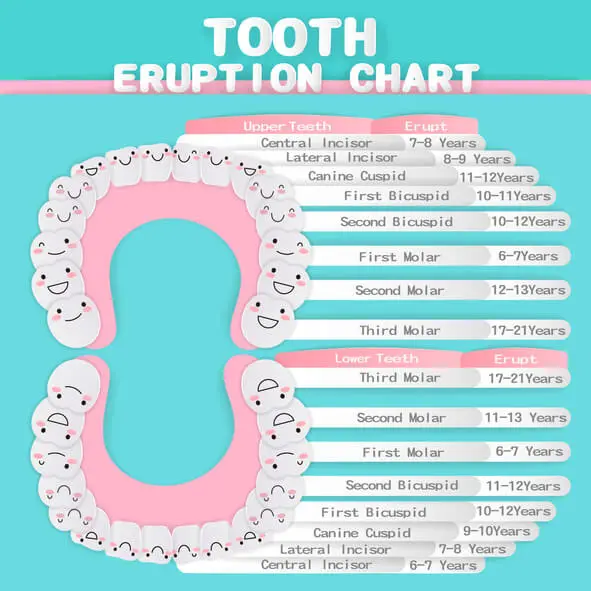
The eruption of primary teeth occurs in a specific sequence, starting with the lower central incisors, followed by the upper central incisors, lateral incisors, first molars, canines, and finally, the second molars. This sequence is crucial for maintaining proper occlusion and facilitating the transition to the permanent dentition.
Following the eruption of primary teeth, a period of mixed dentition ensues, during which both primary and permanent teeth coexist in the oral cavity. The eruption of permanent teeth begins around the age of six and continues into adolescence and early adulthood, culminating in the emergence of the third molars, commonly known as wisdom teeth.
Key Players in Tooth Eruption
Several cellular and molecular factors govern the process of tooth eruption, orchestrating the sequential movement of teeth from their developmental crypts to their functional positions within the dental arch. These key players include:
- Osteoclasts
- Fibroblasts
- Odontoblasts
- Epithelial cells
- Signaling molecules
Osteoclasts
Specialized bone-resorbing cells responsible for creating pathways in the alveolar bone to facilitate tooth movement.
Fibroblasts
Connective tissue cells that play a role in the remodeling of the periodontal ligament, a crucial structure that anchors teeth to the surrounding bone.
Odontoblasts
Cells within the dental pulp responsible for the formation of dentin, the hard tissue that constitutes the bulk of the tooth structure.
Epithelial cells
These cells form the epithelial root sheath, a structure that guides the eruption pathway of developing teeth.
Signaling molecules
Various growth factors, cytokines, and hormones regulate the activity of cells involved in tooth eruption, ensuring coordinated and controlled movement of teeth.
Mechanisms of Tooth Eruption
The process of tooth eruption involves a series of coordinated events orchestrated by the interplay of cellular and molecular mechanisms. While the exact sequence of events may vary slightly between primary and permanent dentition, the underlying principles remain largely conserved.
- Pre-eruptive phase
- Eruptive phase
- Post-eruptive phase
Pre-eruptive phase
Prior to eruption, teeth undergo a phase of root development and elongation within the alveolar bone. During this phase, the dental follicle, a specialized connective tissue surrounding the developing tooth, undergoes differentiation to form the periodontal ligament, cementum, and alveolar bone.
Eruptive phase
As the tooth approaches its functional position, osteoclasts are recruited to resorb bone in the path of eruption, creating a tunnel through which the tooth can emerge. Concurrently, fibroblasts within the periodontal ligament remodel the surrounding tissues to accommodate the advancing tooth.
Post-eruptive phase
Once the tooth has erupted into the oral cavity, the surrounding tissues undergo further remodeling to stabilize the tooth in its functional position. This process involves the deposition of new bone and cementum, as well as the maturation of the periodontal ligament fibers.
Regulation of Tooth Eruption
The timing and sequence of tooth eruption are tightly regulated by a complex interplay of genetic, hormonal, and environmental factors. Several signaling pathways, including the Wnt, BMP, and FGF pathways, have been implicated in the regulation of tooth development and eruption.
Hormones such as parathyroid hormone (PTH), thyroid hormone, and growth hormone play important roles in coordinating the activities of cells involved in tooth eruption. Disruptions in hormonal signaling or genetic mutations can lead to abnormalities in tooth eruption, such as delayed or ectopic eruption, which may necessitate intervention by dental professionals.
Clinical Implications
Understanding the physiology of tooth eruption is crucial for dental practitioners in diagnosing and managing various developmental anomalies and orthodontic conditions. Delayed eruption, impaction, and ectopic eruption are among the common challenges encountered in clinical practice, often requiring timely intervention to prevent complications and preserve oral health.
In cases where tooth eruption is impeded or aberrant, treatment options may include orthodontic interventions, surgical exposure and traction, or extraction followed by prosthetic replacement. Early detection and intervention are paramount to ensure optimal outcomes and prevent long-term sequelae.
Conclusion
Tooth eruption is a marvel of biological engineering, governed by a sophisticated interplay of cellular and molecular mechanisms. From the formation of tooth buds in prenatal development to the emergence of the final complement of permanent teeth in adolescence, the process of tooth eruption is a testament to the intricacies of human development.
By unraveling the mysteries of tooth eruption physiology, researchers and clinicians alike can gain valuable insights into the pathogenesis of developmental anomalies and refine treatment strategies to optimize oral health outcomes. As our understanding of tooth eruption continues to evolve, so too will our ability to unlock its full therapeutic potential and enhance the quality of dental care for generations to come.

