The conventional denture approach for edentulous mandibles can be significantly enhanced by incorporating two implants. Abundant evidence supports the superiority of a two-implant supported overdenture as the preferred treatment option. Particularly in elderly patients, attachment systems that streamline prosthesis placement and removal, while ensuring hygiene, prove invaluable. Among these, axial attachments stand out for their simplified realization techniques, ease of complication management, and cost-effectiveness. This article delineates the features and applications of the Locator attachment, a prominent axial attachment type, through a systematic, step-by-step guide.
Table of Contents
ToggleIntroduction
Edentulous individuals frequently encounter challenges with conventional dentures, including discomfort during chewing and inadequate stability and retention. Studies have demonstrated that overdentures significantly enhance the quality of life and psychological well-being of edentulous patients. They offer improved chewing ability and greater satisfaction compared to conventional complete dentures. Moreover, overdentures are associated with reduced clinical time and financial expenses. Multiple clinical studies have reported favorable outcomes for overdenture prostheses in terms of implant survival and preservation of the residual bony ridge.
Removable implant-retained overdentures offer several advantages over fixed implant prostheses, including better access for oral hygiene, easier modification of the prosthesis base, and improved esthetics. The consensus supports the use of two implants in the interforaminal region of the mandible, either splinted by a bar or placed individually, as the preferred treatment option. The McGill consensus statement advocates for the two-implant overdenture as the primary choice for the edentulous mandible.
Choosing the most suitable attachment for implant overdentures is crucial to ensure even distribution of stress and optimal function. Over time, clinicians have shifted towards axial attachments due to their simplified techniques, easier complication management, and lower cost, especially for patients with limited manual dexterity and motivation for rigorous hygiene.
The Locator attachment, introduced in 2001 by Zest Anchors, has become widely used in clinical practice. It offers self-aligning properties, dual retention in various colors, and vertical height options. The Locator attachment is resilient, retentive, and durable, with built-in angulation compensation. Repair and replacement are quick and straightforward, and existing dentures can be incorporated into the new prosthesis.
This paper aims to provide a comprehensive overview of the characteristics, indications, contraindications, and procedural techniques associated with the Locator attachment.
Materials and Methods
A comprehensive systematic search of English dental literature was conducted, employing key terms such as “overdenture,” “locator,” “abutment (patrix),” “titanium cap,” “copes of nylon,” and “white block-out spacer.” Articles published in peer-reviewed English journals between 1998 and 2012 were identified through searches of the MEDLINE database, supplemented by manual searches of relevant textbooks and annual publications.
Of the articles retrieved, nine discussed the advantages of overdentures, while ten focused on the Locator attachment. Additionally, ten articles addressed complications associated with the Locator attachment system. To support factual statements, additional references were included.
Indications and Contraindications
The primary indications for implant-supported overdentures include financial considerations, anatomical challenges, cosmetic concerns, phonetic issues, hygienic needs, and jaw defects. Conversely, unfavorable morphology represents the sole contraindication for implant-supported overdentures.
In elderly patients, attachment systems facilitating easy placement and removal of prostheses, along with hygienic maintenance, are preferred. The Locator implant attachment system is specifically designed for use with overdentures or partial dentures supported by endosseous implants in the mandible or maxilla. Its low-profile design makes it suitable for cases with limited inter-arch space, and it can accommodate mal-aligned implants due to its reduced attachment height. However, the Locator is not suitable for situations requiring a completely rigid connection, nor is it recommended for use with a single implant exhibiting an axis divergence greater than 20 degrees.
Characteristics
The Locator attachment requires a minimum vertical space of 8.5 mm from the osseous level to the superior surface of the acrylic resin. This measurement is based on the following components:
- 1.8 mm from the osseous level to the implant shoulder
- 1.5 mm for the shortest abutment (including the bevel)
- 3.2 mm for the attachment and processing patrix
- 2 mm of acrylic resin above the attachment.
The minimum horizontal space required is 9.0 mm, with 5.0 mm width for the attachment and an additional 2.0 mm of acrylic resin on each side for adequate bulk and strength.
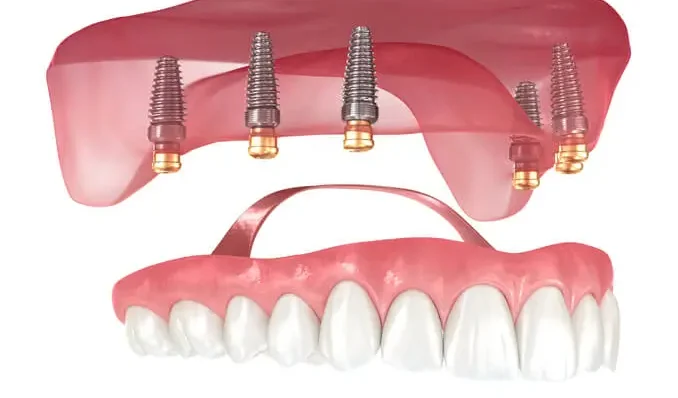
The components of the Locator attachment include:
- A titanium-coated abutment (matrix) compatible with various systems, directly screwed onto the implant.
- Titanium Cap to embed in the resin of the prosthetic base.
- Various copes of nylon:
- Black processing male in polyethylene for direct placement or laboratory use, without resilience.
- Clear replacement male for strong retention (5 lbs) with angulations of 0 to 10 degrees.
- Pink nylon male for less retention (3 lbs) with angulations of 0 to 10 degrees.
- Blue nylon male for extra light retention (1.5 lbs) with angulations of 0 to 10 degrees.
- Green nylon male for angulations of 20 degrees with strong retention.
- Red nylon male for accommodating divergent implants up to 20 degrees (40 degrees between implants) with extra light retention (1.5 lbs).
- Orange nylon male for light retention.
- The new LOCATOR (gray) zero (0) retention nylon replacement male offers a long-term solution for reducing denture retention.
Advantages of the Locator Attachment
- Compatibility with a wide range of implant systems.
- Low profile design, with heights ranging from 3.17 mm for external hexagon implants to 2.5 mm for internal connection systems.
- Variable transmucosal height of the abutment, ranging from 1 to 4 mm, 1 to 5 mm, or 1 to 6 mm, depending on the implant system used, ensuring favorable biomechanical conditions.
- Dual retention mechanism, with both internal and external retention for conventional transparent, pink, and blue males, ensuring longer-lasting performance.
- Long-lasting durability, demonstrated by in vitro insertion-desinsertion testing of 60,000 cycles without alteration.
- Non-rigid connection to the implant, allowing rotational movement to absorb forces without loss of retention.
- Self-locating design facilitates easy seating of the overdenture for patients, eliminating the need for precise alignment of attachment components.
- Simple solutions for managing implant divergence of up to 40 degrees.
- Single tool with three functions for all clinical and laboratory sequences.
Technique
The attachment can be incorporated into the denture either chairside or in the laboratory.
a. Chairside Technique
Chairside “pick up” offers the advantage of creating the attachment in a passive, loaded environment, ensuring complete seating of the denture on the underlying tissues. Although more demanding, this technique allows for the incorporation of attachments into an existing denture.
- Blocking out the rings to prevent acrylic material from flowing into undercuts, with special attention given to blocking out any additional undercut areas.
- Placement of housings to verify full seating of the final prosthesis without interference from attachments or housings.
- Preparation of the final prosthesis for incorporation of the housings.
- Placement of “vent holes” in the attachment area to allow excess material to escape and prevent complete seating on the tissues.
- Viewing of the black processing males, which are secured in place with acrylic while the patient maintains a medium biting force in centric.
Any voids around the housings are filled extraorally, and black processing males are replaced by final retentive inserts with various amounts of retention.
b. Laboratory Processing
Laboratory attachment incorporation is less technique-sensitive but does not consider the level of mucocompression necessary for full seating on the tissues. It is recommended that attachment curing in the base plate be done prior to denture processing at try-in or set-up appointments to evaluate full seating on the tissues and minimize distortion caused by bulk acrylic curing. This allows for evaluation and correction of attachment position before the delivery appointment.
Blocking out undercuts to prevent acrylic flow, ensuring denture removal prevention, and enabling full seating on tissues without interference with attachments are key concerns. Incorporation of a metal framework or lingual reinforcing bar may be necessary to prevent appliance fracture due to minimal acrylic thickness or excessive occlusal forces. However, this entails additional cost and laboratory procedures. In cases of high potential appliance fracture, such as extreme occlusal forces, a metal frame can resist flexure and potential fracture. Providing open space in the framework for attachment incorporation is crucial for laboratory processing.
Complications
The attachment system does not seem to significantly influence implant success rates, with factors such as bone quality, quantity, and arch morphology playing more crucial roles. Sirmahan’s prospective randomized clinical study from 2004 to 2009 found that the Locator system exhibited a higher maintenance rate than ball attachments, with no complications in postinsertion maintenance or implants. Compared to ball and bar designs, the Locator attachment demonstrated fewer complications in clinical practice.
While Locator attachments function reasonably well, long-term evaluations are lacking, which could provide valuable guidance for clinicians in attachment system selection and overdenture design.
Attachment adjustment is reported as the most frequent complication in implant overdentures. Locator attachments offer superior retention and stability compared to Nobel Biocare Ball connectors, but retentive values decrease significantly after multiple pulls. Simulated mastication can reduce Locator attachment retention to 40% of baseline values, particularly affecting nylon capsules.
Increased implant angulation from 0 to 30 degrees leads to reduced retentive force, premature wear of metal components, and increased maintenance. Resilient attachments may lead to denture rotation, potentially causing discomfort and compromising chewing efficiency, especially with anterior teeth. The location of mandibular anterior denture teeth significantly influences rotation movement, with longer dentures decreasing the risk of rotation.
Conclusion
Patients express higher satisfaction levels with implant-retained overdentures compared to conventional complete dentures. Locator attachments demonstrate superiority over ball and bar systems in terms of complication rates in clinical practice. They offer resilience, retention, durability, and built-in angulation compensation, with quick and easy repair and replacement processes.
While Locator attachments perform well in the short term, long-term evaluations are essential for comprehensive assessment.
References
- Batenburg R.H.K., Meijer H., Raghoebar G., Vissink A. Treatment concept for mandibular overdentures supported by endosseous implants: A literature review. Oral Maxillofac Implants. 1998; 13:539-545.
- Assuncao W.G. Comparison between complete denture and implant-retained overdenture: effect of different mucosa thickness and resiliency on stress distribution. Gerodontology. 2009; 26:273–281.
- Balaguer J., Garcia B., Penarrocha M., Peñarrocha M. Satisfaction of patients fitted with implant–retained overdentures. Med Oral Patol Cir Buccal. 2011;16(2):e204-9.
- Vercruyssen M. Long-term, retrospective evaluation (implant and patient-centered outcome) of the two-implants-supported overdenture in the mandible. Part 1: survival rate. Clin Oral Impl Res. 2010;21:357–365.
- Pasciuta M., Grossmann Y., Finger I. A prosthetic solution to restoring the edentulous mandible with limited interarch using an implant-tissue-supported overdenture: a clinical report. J Prosthet Dent. 2005; 93:116-20.
- Lee C.K., Agar J.R. Surgical and prosthetic planning for a two-implant–retained mandibular overdenture: A clinical report. J Prosthet Dent. 2006;95:102-5.
- Hobkirk J. Prosthetic treatment time and satisfaction of edentulous patients treated with conventional or implant-supported complete mandibular dentures: a case-control study (part 1). Int J Prosthodont. 2008;21:489-495.
- Tokuhisa M. In vitro study of a mandibular implant overdenture retained with ball, magnet, or bar attachments: Comparison of load transfer and denture stability. Int J Prosthodont. 2003;16:128–134.
- Andreiotelli M., Att W., Strub J.R. Prosthodontic complications with implant overdentures: A systematic literature review. Int J Prosthodont. 2010;23:195–203.
- Liddelow G., Henry P. A prospective study of immediately loaded single implant-retained mandibular overdentures: preliminary results. J Prosthet Dent. 2007;97:126-137.
- De Jong M.H.M. Posterior mandibular residual ridge resorption in patients with overdentures supported by two or four endosseous implants in a 10-year prospective comparative study. Int J Oral Maxillofac Implants. 2010;25:1168–1174.
- Cheng A.C. Prosthodontic management of edentulous patient with limited oral access using implant-supported prostheses: a clinical report. J Prosthet Dent. 2006;96:1-6.
- Alsabeeha N. Attachment systems for mandibular single-implant overdentures: An in vitro retention force investigation on different designs. Int J Prosthodont. 2010;23:160–166.
- Rutkunas V. Influence of attachment wear on retention of mandibular overdenture. J Oral Rehabil. 2007;34:41–51.
- Rentsch-Kollar A. Mandibular implant overdentures followed for over 10 years: patient compliance and prosthetic maintenance. Int J Prosthodont. 2010;23:91–98.
- Cune M. Mandibular overdentures retained by two implants: 10-year results from a crossover clinical trial comparing ball-socket and bar-clip attachments. Int J Prosthodont. 2010;23:310–317.
- Sunyoung Ma. Marginal bone loss with mandibular two-implant overdentures using different loading protocols: A systematic literature review. Int J Prosthodont. 2010;23:117–126.
- Chung K-H. Retention characteristics of attachment systems for implant overdentures. J Prosthodont. 2004;13:221-226.
- Evtimovska E. The change in retentive values of Locator attachments and Hader clips over time. J Prosthodontics. 2009;18:479–483.
- Sadowsky S. Treatment considerations for maxillary implant overdentures: a systematic review. J Prosthet Dent. 2007;97:340–348.
- Schittly J., Russe P., Hafian H. Prothese amovibles stabilisees sur implants. Indications et modes d’utilisation de l’attachement Locator®. Les cahiers de prothese. 2008;142:33-46.
- Mericske-Stern R. Prosthetic considerations. Australian Dental Journal. 2008;53:49-59.
- Cakarer S. Complications associated with the ball, bar and Locator attachments for implant-supported overdentures. Med Oral Patol Oral Cir Bucal. 2011;16(7):e953-9.
- Engquist B. Advanced Osseointegration Surgery – Quintessenz Verlag, Berlin Overdentures. Chapter 19, p. 233-247.
- Locator implant attachment system. Publication of Zest Anchors corporation on the manufacturer website. Available at www.zestanchors.com.
- Abi Nader S., De Souzan R.F., Fortin D., De Koninck L., Fromentin O., Albuquerque Junior R.F. Effect of simulated masticatory loading on the retention of stud attachments for implant overdentures. J Oral Rehabil. 2011;38(3):157-64.
- Gulizio M.P., Agar J., Kelly J.R., Taylor T.D. Effect of implant angulation upon retention of overdenture attachments. J Prosthodont. 2005;14(1):3-11.
- Kimoto S. Rotational movements of mandibular two-implant overdentures. Clin Oral Impl Res. 2009;20:838–843.
- Kleis W.K., Kämmerer P.W., Hartmann S., Al-Nawas B., Wagner W. A comparison of three different attachment systems for mandibular two-implant overdentures: One-year report. Clin Implant Dent Relat Res. 2010;12(3):209-218.
- Goodacre C.J., Bernal G., Rungcharassaeng K., Kan J.Y. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003;90:121-132.
- Sadig W. A comparative in vitro study on the retention and stability of implant-supported overdentures. Quintessence Int. 2009;40(4):313-9.
- Ortegón S.M., Agar J.R., Taylor T.D., Perdikis D. Retention forces of spherical attachments as a function of implant and matrix angulation in mandibular overdentures: an in vitro study. J Prosthet Dent. 2009;101(4):231-8.
- Thomason J.M., Kelly S.A.M., Bendkowski A., Ellis J.S. Two implant-retained overdentures: A review of the literature supporting the McGill and York consensus statements. J Dent. 2012;40:22–34.
by Dr. Maha Ghotmi, Dr. Loubab Homsy, Dr. Elie Daou