Human oral cavity is a complex structure, essential not only for functions like speaking, chewing, and swallowing but also as a sensory gateway. This complexity is maintained by a network of oral nerves that connect the mouth to the brain, facilitating motor functions, sensory perception, and reflexes. In this article, we delve deep into the oral nerves, exploring their anatomy, functions, and clinical significance.
Table of Contents
ToggleOverview of the Oral Nerve System
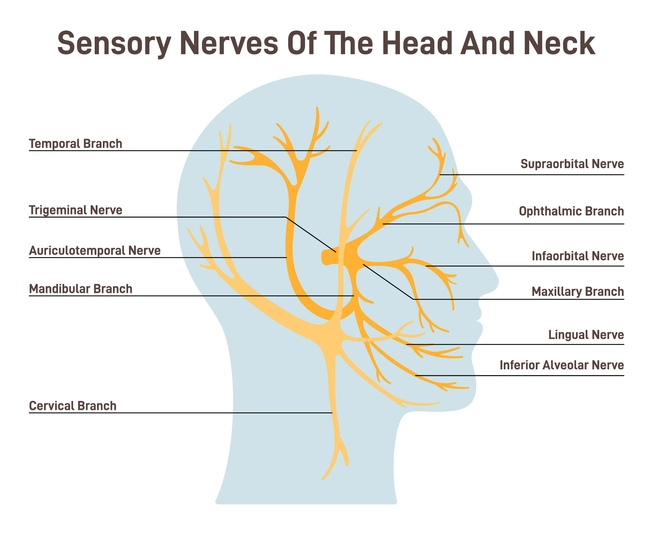
Oral nerves are branches of the cranial nerves, primarily the trigeminal nerve (cranial nerve V), but also involve contributions from the facial nerve (cranial nerve VII), glossopharyngeal nerve (cranial nerve IX), and vagus nerve (cranial nerve X). Additionally, motor control is provided by the hypoglossal nerve (cranial nerve XII). These nerves are integral to sensory and motor control of the oral structures such as the tongue, teeth, palate, and mucosa.
Trigeminal Nerve (Cranial Nerve V)
The trigeminal nerve is the largest cranial nerve and has three main divisions: ophthalmic (V1), maxillary (V2), and mandibular (V3). Of these, the maxillary and mandibular divisions are directly involved in oral functions.
Maxillary Division (V2)
The maxillary nerve exits the skull through the foramen rotundum and branches further.
Oral Contributions:
- Infraorbital Nerve: Provides sensation to the upper lip, cheek, and nose.
- Superior Alveolar Nerves: Divided into anterior, middle, and posterior branches, these nerves innervate the maxillary teeth and the associated gingiva.
- Greater and Lesser Palatine Nerves: Supply the hard and soft palate. Nasopalatine Nerve: Provides sensation to the anterior hard palate and the incisive papilla.
Mandibular Division (V3)
The mandibular nerve exits the skull through the foramen ovale.
Oral Contributions:
- Inferior Alveolar Nerve: Travels through the mandibular canal, innervating the lower teeth before emerging as the mental nerve to supply the lower lip and chin.
- Lingual Nerve: Provides general sensation to the anterior two-thirds of the tongue, the floor of the mouth, and the mandibular gingiva.
- Buccal Nerve: Supplies the cheek mucosa and gingiva adjacent to the molars.
- Auriculotemporal Nerve: Contributes minorly to oral structures but is essential for pain referral in cases like temporomandibular joint disorders.
Functions:
Sensory: Perception of touch, pain, pressure, and temperature in the oral cavity.
Clinical Relevance:
- Trigeminal Neuralgia: A chronic pain condition often involving V2 and V3.
- Dental Anesthesia: Inferior alveolar and infraorbital nerve blocks are common in dentistry.
Facial Nerve (Cranial Nerve VII)
The facial nerve is primarily a motor nerve but has crucial sensory and parasympathetic components.
Chorda Tympani Nerve
Function: Carries taste sensation from the anterior two-thirds of the tongue and parasympathetic fibers to the submandibular and sublingual glands.
Pathway: Joins the lingual nerve of the mandibular division of the trigeminal nerve.
Motor Branches
Control muscles of facial expression, including the orbicularis oris, which aids in lip movements during speech and eating.
Functions
- Sensory: Taste perception.
- Motor: Facilitation of oral movements and saliva secretion.
Clinical Relevance
- Bell’s Palsy: A condition where facial nerve dysfunction can cause partial or complete paralysis, affecting oral functions like speech and mastication.
- Glossodynia: Altered taste sensation due to chorda tympani dysfunction.
Glossopharyngeal Nerve (Cranial Nerve IX)
The glossopharyngeal nerve is a mixed nerve with motor, sensory, and autonomic components.
Oral Contributions:
- Sensory: Provides general and taste sensation to the posterior one-third of the tongue.
- Motor: Supplies the stylopharyngeus muscle, aiding in swallowing.
- Autonomic: Parasympathetic innervation to the parotid salivary gland via the otic ganglion.
Functions:
- Taste: Mediates the bitter taste from the posterior tongue.
- Sensory: Perceives temperature, pain, and touch in the posterior oral cavity.
- Motor: Coordinates swallowing.
Clinical Relevance:
- Glossopharyngeal Neuralgia: Sharp pain in the posterior tongue, throat, and ear.
- Dysphagia: Difficulty swallowing, often due to nerve dysfunction.
Vagus Nerve (Cranial Nerve X)
The vagus nerve has an extensive distribution, including significant roles in the oral cavity and pharynx.
Oral Contributions:
- Sensory: Supplies the pharynx, larynx, and parts of the soft palate.
- Motor: Provides innervation to the palatoglossus muscle, which elevates the posterior tongue.
Functions:
- Sensory: Ensures reflexive actions like gagging and swallowing.
- Motor: Assists in coordinating speech and swallowing movements.
Clinical Relevance:
- Vagus Nerve Injury: Results in uvular deviation and impaired swallowing.
- Dysarthria: Speech difficulties due to impaired motor control.
Hypoglossal Nerve (Cranial Nerve XII)
The hypoglossal nerve is the primary motor nerve for the tongue.
Oral Contributions:
- Innervates all intrinsic and extrinsic muscles of the tongue except for the palatoglossus (vagus nerve).
- Allows for complex tongue movements essential for speech, chewing, and swallowing.
Functions:
Motor: Controls tongue position, shaping, and movements.
Clinical Relevance:
Hypoglossal Nerve Palsy: Causes tongue deviation toward the affected side and atrophy, impairing speech and swallowing.
Lesser-Known Nerves with Oral Contributions
- Nerve to Mylohyoid (Branch of Mandibular Nerve)
- Sympathetic Nerves
- Parasympathetic Components
Nerve to Mylohyoid (Branch of Mandibular Nerve)
Innervates the mylohyoid and anterior belly of the digastric muscles, contributing to oral floor movements and mastication.
Sympathetic Nerves
Regulate blood flow and salivary gland activity, influencing oral health.
Parasympathetic Components
Control secretion from salivary glands, aiding in lubrication and digestion.
Clinical Importance of Oral Nerves
The intricate network of oral nerves makes them a focus in clinical diagnoses and treatments:
- Dental Procedures: Knowledge of nerve pathways is crucial for effective local anesthesia.
- Oral Pathologies: Conditions like burning mouth syndrome, neuralgias, and referred pain highlight the importance of oral nerve health.
- Speech Therapy: Damage to hypoglossal or facial nerves can impair speech articulation.
- Rehabilitative Medicine: Post trauma or post surgical rehabilitation often involves retraining oral nerve functions.
Frequently Asked Questions (FAQs)
Why do my teeth hurt when I have a sinus infection?
The maxillary sinus is located near the superior alveolar nerves (V2 branch of CN V), which supply the upper teeth. Sinus inflammation can put pressure on these nerves, causing referred pain in the teeth.
What nerve is responsible for the gag reflex?
The glossopharyngeal nerve (CN IX) is responsible for the sensory aspect, while the vagus nerve (CN X) controls the motor aspect of the gag reflex.
What causes facial numbness or tingling?
Facial numbness can result from trigeminal nerve dysfunction (CN V), often due to:
- Trigeminal neuralgia.
- Dental anesthesia.
- Multiple sclerosis or nerve compression.
Which nerve is blocked for wisdom tooth extraction?
The inferior alveolar nerve (a branch of V3, CN V) is typically blocked for lower wisdom tooth extractions.
Can nerve damage affect taste?
Yes. Damage to:
- Chorda tympani nerve (CN VII) affects the anterior two-thirds of the tongue.
- Glossopharyngeal nerve (CN IX) affects the posterior one-third of the tongue.
How does the hypoglossal nerve affect speech?
The hypoglossal nerve (CN XII) controls tongue movements, which are essential for articulating words. Damage can result in slurred speech (dysarthria).
Why do I feel tingling in my tongue after dental work?
This is often due to temporary irritation or damage to the lingual nerve (a branch of CN V3), which can occur during anesthesia or extractions.
What is the most painful nerve condition affecting the face?
Trigeminal Neuralgia is considered one of the most painful conditions, causing sharp, electric-shock-like pain in areas supplied by CN V.
Conclusion
The oral nerves are vital components of cranial nerve anatomy, underpinning the sensory, motor, and autonomic functions of the oral cavity. Their contributions extend beyond routine oral activities to critical roles in communication and reflex actions. A deeper understanding of these nerves not only enhances clinical practices in dentistry, otolaryngology, and neurology but also underscores the elegance of human anatomy. By appreciating the detailed workings of oral nerves, practitioners can diagnose, manage, and treat related disorders with precision and care.