Oral nerve damage is a serious condition that affects the sensory and motor functions of the mouth, lips, tongue, and surrounding tissues. The oral cavity is richly innervated by several cranial nerves, and any damage to these nerves can lead to pain, numbness, loss of function, or altered sensation. This article explores the causes, symptoms, diagnosis, and treatment options for oral nerve damage, along with preventive measures and long-term implications.
Table of Contents
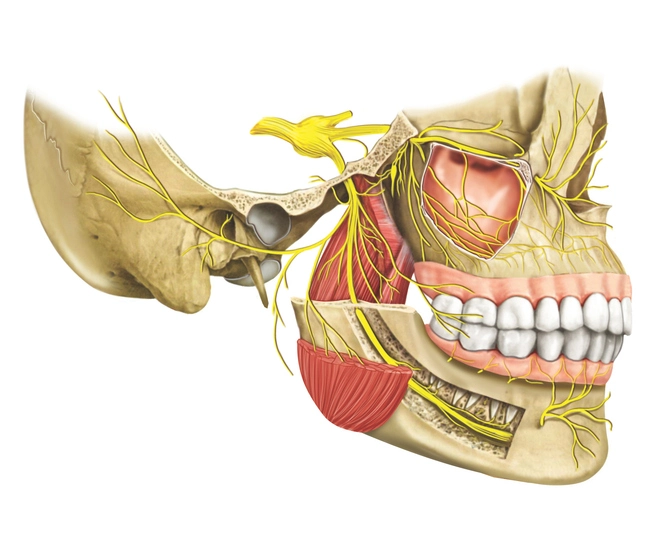
ToggleAnatomy of Oral Nerves
The oral cavity is innervated by a complex network of cranial nerves that control sensation, movement, and autonomic functions. Understanding these oral nerves is crucial in diagnosing and managing nerve-related oral conditions.
Trigeminal Nerve (Cranial Nerve V)
The trigeminal nerve is the largest cranial nerve and the primary nerve responsible for sensation in the oral and facial regions. It has three main branches:
- Ophthalmic Division (V1): Supplies sensation to the forehead, upper eyelid, and part of the nose but does not directly influence oral structures.
- Maxillary Division (V2): Provides sensory innervation to the upper jaw, including the upper teeth, maxillary sinus, nasal cavity, and the hard and soft palate.
- Mandibular Division (V3): This is the only mixed (sensory and motor) division, supplying sensory input to the lower teeth, lower lip, chin, and tongue. It also controls the muscles involved in mastication (chewing), including the masseter, temporalis, and pterygoid muscles.
- Inferior Alveolar Nerve: A key branch of the mandibular nerve that runs through the mandibular canal, supplying sensation to the lower teeth and emerging as the mental nerve to innervate the lower lip and chin.
- Lingual Nerve: Provides sensation to the anterior two-thirds of the tongue and floor of the mouth, crucial for taste and tactile perception.
Facial Nerve (Cranial Nerve VII)
The facial nerve primarily controls facial expression but also has an essential role in oral functions:
- Supplies motor control to the buccinator muscle, which helps keep food between the teeth during chewing.
- Carries taste sensations from the anterior two-thirds of the tongue via the chorda tympani branch.
- Plays a role in salivary gland function by innervating the submandibular and sublingual glands.
Glossopharyngeal Nerve (Cranial Nerve IX)
The glossopharyngeal nerve has both sensory and motor components:
- Provides sensory input to the posterior one-third of the tongue, including taste and general sensation.
- Innervates the oropharynx and tonsils, playing a role in swallowing and gag reflex.
- Contributes to the autonomic regulation of the parotid salivary gland.
Hypoglossal Nerve (Cranial Nerve XII)
The hypoglossal nerve is solely responsible for motor control of the tongue muscles, including the genioglossus, hyoglossus, and styloglossus muscles. These muscles are essential for speech, chewing, and swallowing.
Other Contributing Nerves
- Vagus Nerve (Cranial Nerve X): Plays a role in swallowing and speech by innervating the muscles of the soft palate, pharynx, and larynx.
- Accessory Nerve (Cranial Nerve XI): Assists in some movements of the soft palate and pharynx.
Causes of Oral Nerve Damage
Oral nerve damage can occur due to various reasons, including:
- Dental Procedures
- Trauma and Injuries
- Oral Surgeries
- Neurological Disorders
- Infections and Diseases
Dental Procedures
- Tooth Extractions: Particularly with wisdom teeth removal, where the inferior alveolar nerve (IAN) or lingual nerve can be damaged.
- Root Canal Treatment: Improper instrumentation or excessive filling material can lead to nerve compression or trauma.
- Dental Implants: Incorrect implant placement can impinge on the inferior alveolar nerve, leading to paresthesia (numbness or tingling).
- Orthodontic Treatment: Excessive pressure on teeth can lead to nerve compression.
Trauma and Injuries
- Facial Trauma: Accidents, sports injuries, or surgical procedures can cause direct nerve injury.
- Burns or Chemical Exposure: Hot foods, acids, or alkaline substances can damage nerve endings in the oral mucosa.
- Bite Injuries: Self-inflicted or accidental biting of the tongue or lips can cause nerve damage.
Oral Surgeries
- Jaw Surgeries: Procedures such as orthognathic surgery can inadvertently affect nerve pathways.
- Biopsy or Tumor Removal: Surgical interventions in the oral cavity can impact local nerve structures.
Neurological Disorders
- Trigeminal Neuralgia: A chronic pain condition affecting the trigeminal nerve (trigeminal neuralgia), leading to severe facial pain.
- Multiple Sclerosis (MS): Demyelination of nerves can lead to oral and facial numbness.
- Diabetes-Related Neuropathy: High blood sugar levels can contribute to nerve degeneration, including oral nerves.
Infections and Diseases
- Viral Infections: Herpes simplex virus (HSV) or varicella-zoster virus (shingles) can affect oral nerves.
- Bacterial Infections: Abscesses, osteomyelitis, or severe periodontal disease can contribute to nerve damage.
- Oral Cancer: Tumors growing in or around nerves (oral cancer) can cause compression and loss of function.
Symptoms of Oral Nerve Damage
Symptoms vary depending on the severity and location of the damage but can include:
- Numbness (Paresthesia): Loss of sensation in the affected area.
- Tingling or Burning Sensation: Often described as “pins and needles.”
- Pain or Neuralgia: Sharp, shooting pain along the nerve distribution.
- Altered Taste Perception: Affected taste buds due to nerve damage.
- Muscle Weakness or Paralysis: Difficulty in speaking, chewing, or moving the tongue.
- Excessive Salivation or Dry Mouth: Disruption in autonomic nerve function.
Diagnosis of Oral Nerve Damage
Proper diagnosis is crucial for effective management. A healthcare provider may use the following diagnostic tools:
- Clinical Examination: Assessment of sensation, motor function, and pain response in the affected area. Checking for asymmetry or muscle weakness in the face or tongue.
- Electromyography (EMG): Measures electrical activity in muscles to detect nerve dysfunction.
- Quantitative Sensory Testing (QST): Evaluates sensory thresholds to assess nerve function.
- MRI or CT Scans: Helps identify structural abnormalities, tumors, or nerve compression.
- Nerve Biopsy: In rare cases, a biopsy may be performed to evaluate nerve tissue pathology.
Treatment Options
Treatment depends on the underlying cause and severity of nerve damage.
Medications
- Pain Relievers: NSAIDs or opioids for severe pain.
- Anticonvulsants: Gabapentin or carbamazepine for neuropathic pain.
- Corticosteroids: Reduce inflammation and swelling around nerves.
- Topical Anesthetics: Lidocaine patches or gels for localized pain relief.
Physical Therapy
- Desensitization Therapy: Helps retrain nerves and reduce abnormal sensations.
- Muscle Exercises: For facial muscle rehabilitation.
Surgical Intervention
- Microsurgical Repair: Nerve grafting or direct nerve repair in cases of severe injury.
- Decompression Surgery: Used when nerves are compressed by surrounding structures.
Alternative Therapies
- Acupuncture: May provide pain relief and promote nerve healing.
- Vitamin B12 Supplements: Beneficial for nerve regeneration.
Preventive Measures
To reduce the risk of oral nerve damage, consider the following precautions:
- Choose experienced dental professionals for invasive procedures.
- Follow proper post-operative care after dental or surgical interventions.
- Avoid excessive force or trauma to the oral region.
- Maintain optimal oral hygiene to prevent infections.
Long-Term Implications and Prognosis
Recovery from oral nerve damage varies depending on the cause and severity:
- Mild Cases: Sensation and function may return within weeks to months.
- Moderate Cases: May take several months to a year for partial or full recovery.
- Severe Cases: Permanent nerve damage may lead to chronic pain, numbness, or functional impairment.
Frequently Asked Questions (FAQs)
What are the symptoms of nerve damage in the mouth?
Symptoms of nerve damage in the mouth may include numbness, tingling, burning sensations, pain, or loss of taste. Some individuals may also experience a heightened sensitivity to temperature or pressure, making eating and drinking uncomfortable. In severe cases, difficulty speaking or chewing may also occur.
Can dental nerve damage be cured?
In some cases, dental nerve damage can heal on its own over time, especially if the injury is minor. The body’s natural healing process can regenerate nerves, but this can take weeks to months. However, severe cases may require medical intervention such as medication (e.g., pain relievers, anti-inflammatory drugs, or nerve stabilizing medications), physical therapy, or surgery. In certain cases where nerve damage is irreversible, long-term pain management strategies may be necessary.
Can you sue a dentist for nerve damage in the UK?
Yes, if a dentist’s negligence caused the nerve damage, you may be able to file a dental negligence claim in the UK. To succeed in a claim, you would need to prove that the dentist breached their duty of care and that this directly resulted in nerve damage. Compensation may cover medical expenses, pain and suffering, and potential loss of earnings. Consulting a legal professional specializing in dental negligence can help you understand your rights and options.
What are the 7 signs of inferior alveolar nerve damage?
The seven signs include:
- Numbness or tingling in the lower lip and chin – This is often one of the first symptoms of nerve damage.
- Pain or burning sensation – Some individuals experience persistent pain or a burning feeling in the affected area.
- Difficulty speaking – If the nerve damage affects movement or sensation, forming words properly can become challenging.
- Trouble chewing food – Reduced sensation or discomfort in the jaw can make chewing difficult.
- Altered taste perception – Damage to the nerve may lead to changes in how flavors are perceived.
- Unusual sensations in the gums or teeth – Some people report tingling, electric shock-like feelings, or increased sensitivity.
- Loss of sensation in the affected area – In severe cases, there may be complete numbness in the lips, chin, or gums.
Can a dentist tell if you have nerve damage?
Yes, a dentist can assess nerve damage through clinical evaluation and diagnostic tests. They may ask about your symptoms, check for changes in sensation, and use imaging techniques like X-rays or CBCT scans to identify any structural damage. In some cases, nerve conduction studies or referrals to a specialist (such as a neurologist or oral surgeon) may be necessary to determine the extent of the damage.
How do you get rid of nerve pain in your mouth?
Treatment options depend on the severity of the nerve pain and the underlying cause. Common approaches include:
- Pain relievers such as ibuprofen or acetaminophen for mild discomfort.
- Anti-inflammatory medications to reduce swelling that may be pressing on the nerve.
- Nerve-stabilizing drugs like gabapentin or pregabalin, which are often used for neuropathic pain.
- Topical anesthetics such as lidocaine gels or rinses to provide temporary relief.
- Physical therapy or acupuncture to promote nerve healing and pain relief.
- Surgical intervention in cases where there is significant nerve damage that does not heal naturally.
How long does nerve damage in the mouth take to heal?
Healing time varies depending on the severity of the damage. Minor nerve injuries can heal within a few weeks to months as the nerve regenerates. Moderate nerve damage may take several months to a year, while severe or complete nerve injuries could take years or be permanent. Early diagnosis and appropriate treatment can improve the chances of recovery.
How to test for dental nerve damage?
Testing for dental nerve damage may involve:
- Physical examination to check for numbness, tingling, or pain response.
- Sensitivity tests using cold, heat, or electrical stimulation to assess nerve function.
- X-rays or CBCT scans to check for structural damage or impingement on the nerves.
- Nerve conduction studies to evaluate how well the nerves are transmitting signals.
- Clinical observations where the dentist or specialist assesses speech, chewing function, and muscle control.
What does a damaged tooth nerve feel like?
A damaged tooth nerve may cause sharp, throbbing pain, sensitivity to hot or cold temperatures, tingling, or a dull ache in the affected area. Some individuals describe it as an electric shock-like sensation when the nerve is triggered. If the nerve is completely dead, the pain may subside, but the tooth may become discolored due to lack of blood supply, which could indicate the need for treatment such as a root canal.