Maxillofacial trauma poses a major challenge in emergency and reconstructive medicine. The maxilla, being a central structure in the midface, plays a pivotal role in facial aesthetics, occlusion, speech, and mastication. Maxillary fractures not only affect the structural integrity of the face but also compromise the function of adjacent anatomical structures, including the orbit, nasal cavity, and oral cavity. Prompt recognition and appropriate intervention are critical to minimize long-term morbidity.
Table of Contents
ToggleAnatomy of the Maxilla
Understanding the complex anatomy of the maxilla is crucial for accurate diagnosis and effective treatment of fractures.
Structural Overview
The maxilla is a paired bone that forms the central part of the facial skeleton. Each maxillary bone comprises the following parts:
- Body of the Maxilla: Contains the maxillary sinus.
- Frontal Process: Articulates with the frontal bone.
- Zygomatic Process: Connects to the zygomatic bone.
- Alveolar Process: Houses the upper teeth.
- Palatine Process: Forms the anterior three-quarters of the hard palate.
Articulations and Functional Significance
The maxilla articulates with nine other bones and plays an essential role in:
- Supporting the orbit.
- Forming part of the nasal cavity and palate.
- Maintaining the dental arch.
- Contributing to facial contour and expression.
Etiology and Mechanism of Injury
Maxillary fractures are typically associated with high-energy trauma due to the anatomical location of the maxilla in the central midface. The causes vary depending on demographics, socioeconomic factors, geographic regions, and population behaviors.
Epidemiological Context
Maxillary fractures account for approximately 6–25% of all facial fractures, depending on the setting. In polytrauma patients, particularly those with road traffic injuries or craniofacial trauma, maxillary fractures are often part of a broader pattern of skeletal injury. They frequently co-occur with nasal, orbital, zygomatic, and mandibular fractures, increasing diagnostic complexity and treatment urgency.
Demographic Trends:
- Gender: Males are affected more frequently than females, with a male-to-female ratio ranging from 3:1 to 8:1, attributed to greater involvement in high-risk activities and occupations.
- Age: Most common in individuals aged 20–40 years.
- Socioeconomic Status: Low- to middle-income populations show a higher incidence due to poor road safety standards and limited access to protective equipment.
Common Causes of Maxillary Fractures
1. Motor Vehicle Collisions (MVCs)
- Most prevalent global cause of midfacial trauma.
- High-velocity impact, particularly without the use of seat belts or airbags, can transmit significant force to the midface.
- Common in both drivers and passengers, especially when the face strikes the steering wheel, dashboard, or windshield.
- May result in complex Le Fort II or III fractures depending on the direction and magnitude of force.
2. Interpersonal Violence (Assault)
- Second most common cause, especially in urban settings and among young adult males.
- Common mechanisms include punches, blunt objects (e.g., baseball bats), or weapons.
- Usually results in unilateral or localized fractures, such as alveolar ridge fractures or isolated maxillary sinus wall damage.
- Frequently involves soft tissue injuries, complicating clinical evaluation.
3. Falls
- Elderly individuals are especially at risk due to impaired balance and decreased bone density.
- Children and infants may sustain maxillary fractures from falling off beds, furniture, or while learning to walk.
- Falls in younger individuals often lead to Le Fort I or alveolar fractures, while more complex patterns are seen in elderly patients due to osteoporosis.
4. Sports Injuries
- Contact sports such as boxing, rugby, football (soccer), hockey, and mixed martial arts often involve facial impacts.
- Non-contact sports like cycling, skateboarding, and skiing can also lead to trauma if protective gear is not worn.
- Maxillary fractures in these cases are usually isolated but may be accompanied by orbital floor (“blowout”) fractures.
5. Occupational and Industrial Accidents
- Particularly common in construction, factory, or agriculture workers where exposure to falling tools or machinery is high.
- Resultant fractures may be part of a comminuted or panfacial trauma pattern.
6. Gunshot and Blast Injuries
- Rare but devastating causes of maxillary fractures.
- Typically produce grossly comminuted fractures with severe soft tissue destruction.
- Often require multistage surgical reconstruction and have a high complication rate.
7. Iatrogenic and Post-Surgical Trauma
- Dental extractions, particularly of upper molars, may occasionally result in fractures of the alveolar ridge or disruption of the maxillary sinus floor.
- Orthognathic or sinus surgery carries a small risk of inadvertent fracture extension, especially in cases with pre-existing bone pathology.
Mechanism of Injury
The nature of the impacting force—its direction, magnitude, and point of contact—largely determines the type and severity of the maxillary fracture.
Direction of Force
- Anterior-posterior force (e.g., frontal collision): Often leads to Le Fort II or III fractures, affecting nasal, orbital, and zygomatic regions.
- Inferior-superior force (e.g., upward punch or fall on chin): May result in Le Fort I fractures or involve both maxilla and mandible.
- Lateral force (e.g., side impact in sports or accidents): Commonly causes zygomaticomaxillary complex (ZMC) or orbital rim fractures.
Force Magnitude
- Low-energy trauma: May result in simple, non-displaced alveolar or sinus wall fractures.
- High-energy trauma: Typically causes displaced, comminuted, or bilateral fractures with a higher risk of neurovascular and orbital injuries.
Bone Density and Resistance
- In young adults, the dense bone structure offers more resistance, requiring higher force for fractures to occur.
- In older adults or children, relatively weaker or developing bone makes them more susceptible even to low-force impacts.
Pathological Fractures
Though rare, pathological conditions can predispose the maxilla to fractures even under minor trauma.
Osteomyelitis or Chronic Infections
Chronic sinus infections, especially in immunocompromised patients, can weaken bony walls.
Tumors or Cysts
Benign and malignant lesions, such as odontogenic cysts, ameloblastomas, or metastatic lesions, can compromise structural integrity.
Osteoporosis and Systemic Disorders
Metabolic bone diseases, including Paget’s disease or osteogenesis imperfecta, can increase fracture risk.
Classification of Maxillary Fractures
Accurate classification of maxillary fractures is crucial for clinical communication, treatment planning, and prognosis. Because the maxilla is centrally located in the facial skeleton and articulates with several other bones, fractures often extend into adjacent anatomical structures, making classification both complex and essential. Various systems have been developed over the years to classify these injuries based on anatomical, radiological, and clinical criteria.
Historical Perspective
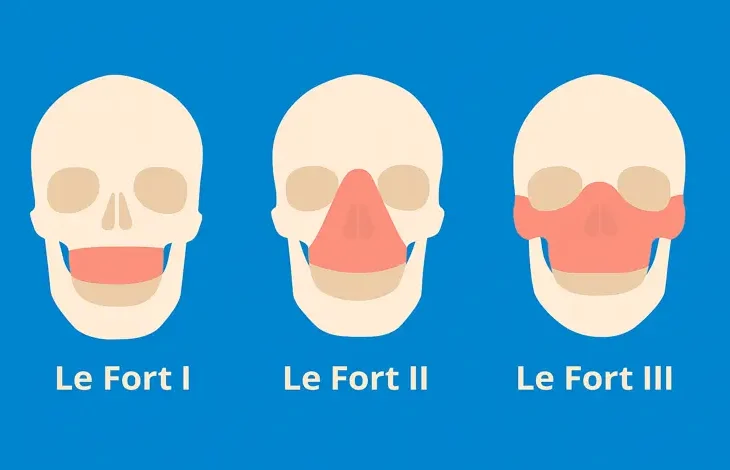
The most widely accepted system for classifying midfacial fractures, particularly maxillary injuries, is the Le Fort classification, named after the French surgeon René Le Fort, who in 1901 conducted experimental trauma studies on cadaver skulls. By applying controlled blunt forces at various angles and intensities, he observed predictable fracture patterns in the midface, which he categorized into three types. Despite being over a century old, this classification remains a cornerstone in maxillofacial trauma management.
However, real-life trauma is rarely as orderly as experimental conditions, and fractures often occur in mixed or atypical patterns. Therefore, in addition to Le Fort types, modern classification incorporates isolated, complex, and combined fracture types, especially as identified by computed tomography (CT) imaging.
Le Fort Classification
The Le Fort system is based on fracture patterns that separate portions of the midface from the skull base. These are horizontal or pyramidal fractures occurring at various levels. Each type is characterized by its plane of fracture, the bones involved, and the direction of traumatic force.
Le Fort I (Horizontal or Low Transverse Fracture)
Fracture Pattern: Horizontal separation of the maxilla from the pterygoid plates and nasal septum. The fracture line typically passes through:
Maxillary sinuses (posterior and anterior walls)
Lower part of the nasal septum
Pterygoid plates of the sphenoid bone
Alveolar ridge (above the apices of the teeth)
Clinical Features:
Mobility of the hard palate and upper teeth (floating palate).
Malocclusion.
Epistaxis and swelling of the upper lip.
Ecchymosis in the buccal sulcus.
Step deformity at the nasal floor.
Mechanism: Typically results from a blow to the lower maxilla (e.g., punch or blunt object hitting above the upper lip).
Le Fort II (Pyramidal Fracture)
Fracture Pattern: Pyramidal-shaped fracture that detaches the central midface. The fracture extends through:
Nasal bridge
Inferior orbital rim and floor
Maxillary sinus walls
Lacrimal bones
Zygomaticomaxillary suture
Pterygoid plates
Clinical Features:
Central midface mobility (floating maxilla).
Bilateral periorbital ecchymosis.
Infraorbital nerve anesthesia (cheek and upper lip).
Nasal deformity, epistaxis.
Enophthalmos or diplopia if the orbit is involved.
Mechanism: Caused by a blow to the midface, such as hitting the dashboard during a vehicle collision.
Le Fort III (Craniofacial Disjunction)
Fracture Pattern: Complete separation of the midface from the skull base. The fracture line involves:
Nasofrontal suture
Ethmoid bones
Orbits (medial and lateral walls)
Zygomatic arches
Pterygoid plates
Clinical Features:
Entire face moves as a unit when tested.
Severe facial flattening or elongation.
CSF rhinorrhea (from skull base breach).
Ocular dystopia, diplopia, or blindness.
Airway compromise.
Mechanism: High-velocity trauma to the upper face, such as major vehicle crashes or falls from significant heights.
Limitations of the Le Fort System
While widely used, the Le Fort classification has limitations:
- Many fractures do not follow classical Le Fort patterns, especially in real-life trauma.
- Unilateral fractures or combinations of types are common.
- It does not describe the degree of comminution, displacement, or associated soft tissue injuries.
- It excludes alveolar fractures and isolated orbital or sinus wall fractures.
Modern imaging (especially multislice CT with 3D reconstruction) often reveals fracture lines that don’t neatly conform to Le Fort categories. As such, additional classifications and terminology are used.
Other Types of Maxillary Fractures
Isolated Maxillary Wall Fractures
Involve a single wall or process of the maxilla:
Anterior wall
Posterior wall
Lateral wall
Floor (roof of maxillary sinus)
These fractures are typically the result of lower-energy trauma and are often seen with orbital floor fractures or dental injuries.
May present with localized tenderness, swelling, or crepitus.
Alveolar Ridge Fractures
Limited to the alveolar process, often involving the teeth and surrounding bone.
Typically occur due to:
Sports injuries
Falls
Complicated dental extractions
Clinical signs:
Loose teeth or tooth segments
Malocclusion
Bleeding and pain in the gingiva
Disruption of the dental arch
May require splinting, dental fixation, or surgical stabilization.
Zygomaticomaxillary Complex (ZMC) Fractures
Involve the lateral midface, including:
Zygomatic arch
Infraorbital rim and floor
Zygomaticomaxillary suture
Frontal process of the zygoma
Sometimes called tripod fractures (though anatomically it involves four points).
Frequently associated with Le Fort III or orbital floor fractures.
Clinical features:
Flattened cheekbone
Diplopia
Infraorbital nerve anesthesia
Trismus (due to involvement of the coronoid process of mandible)
Comminuted or Panfacial Fractures
High-impact trauma, such as blast injuries or high-speed collisions, may lead to:
Multiple overlapping fracture patterns
Loss of bony continuity
Severe soft tissue avulsion
Require multistage surgical reconstruction and careful airway and nutritional management.
CT-Based Modern Classifications
With the advent of high-resolution CT imaging, some authors propose CT-based systems that:
- Document exact fracture lines.
- Classify based on bone involvement, displacement, and comminution.
- Provide 3D mapping of fracture components.
While no single standardized CT-based classification has replaced Le Fort types, CT imaging is now universally used to supplement and refine diagnosis, especially in atypical or mixed injuries.
AO CMF (AO Foundation CranioMaxillofacial) Classification
A modern, detailed, and hierarchical classification system used in academic and surgical settings. It is part of the AO Foundation’s global trauma classification protocols.
- Divides the midface into specific anatomical zones.
- Describes fracture morphology, location, and severity.
- More comprehensive and suitable for complex or panfacial trauma.
- Useful in surgical planning, research, and documentation.
Clinical Relevance of Classification
Why classification matters:
- Guides treatment: Whether open reduction is necessary and which surgical approaches to use.
- Predicts complications: Le Fort III injuries require skull base evaluation, potential CSF leak management.
- Facilitates communication: Between surgeons, radiologists, and emergency teams.
- Supports legal and forensic analysis: Especially in cases of assault, abuse, or trauma litigation.
Summary Table of Maxillary Fracture Types
| Type | Fracture Line Involves | Common Signs | Usual Cause |
|---|---|---|---|
| Le Fort I | Maxillary sinus, alveolar ridge | Mobile palate, malocclusion | Blow to lower midface |
| Le Fort II | Nasal bridge, orbital rim, zygoma | Pyramidal mobility, infraorbital numbness | Frontal impact |
| Le Fort III | Orbit, zygomatic arch, skull base | Craniofacial disjunction, CSF leak | High-energy trauma |
| Alveolar | Dental alveolus | Loose teeth, bleeding | Sports, dental trauma |
| Isolated Wall | One sinus or wall | Local swelling, tenderness | Low-energy impact |
| ZMC | Cheekbone, orbital floor | Flattening, diplopia | Assaults, MVCs |
| Comminuted | Multiple facial bones | Severe disfigurement | Blast, industrial injury |
Clinical Presentation and Evaluation
Accurate clinical assessment of a suspected maxillary fracture is critical to ensure proper diagnosis, avoid missed injuries, and guide imaging and treatment strategies. Due to the maxilla’s central anatomical location and its connections to the orbit, nasal cavity, and cranial base, maxillary fractures can manifest through a wide spectrum of signs and symptoms.
A thorough clinical evaluation should include a detailed history, meticulous physical examination, and an assessment for associated injuries that may alter management priorities, especially in trauma settings. Additionally, coordination with specialties such as ophthalmology, neurosurgery, ENT, and dentistry is often required.
History Taking
A structured and detailed history provides the foundation for diagnosis.
Mechanism of Injury
- Clarify how the trauma occurred—high-speed MVC, fall, assault, sports injury, industrial accident, etc.
- Determine the direction and force of impact.
- A high-energy mechanism suggests a greater likelihood of complex or multiple fractures.
Timing of Injury
Helps assess swelling progression, risk of infection, or delayed complications.
Associated Symptoms
Ask targeted questions to uncover symptoms of complications or concurrent injuries:
- Nasal obstruction or deformity
- Epistaxis (nosebleed)
- Facial numbness (especially under the eyes or upper lip—suggesting infraorbital nerve involvement)
- Double vision (diplopia) or blurred vision
- Tooth mobility, loss, or bite disturbance
- Jaw stiffness or difficulty opening mouth (trismus)
- Hearing changes (suggestive of middle ear involvement)
- CSF rhinorrhea (suggesting skull base involvement)
- Headache, loss of consciousness, or neurological symptoms (pointing to brain injury)
Past Medical History
- Recent dental procedures?
- History of sinus infections?
- Osteoporosis or bone disorders?
- Use of anticoagulants or bleeding disorders?
General Trauma Evaluation
In high-impact trauma, a maxillary fracture may be just one component of a broader pattern of injury. Begin with a primary trauma survey using the ATLS (Advanced Trauma Life Support) protocol:
- Airway with cervical spine protection
- Breathing
- Circulation
- Disability (neurologic assessment)
- Exposure (full body exam)
Severe Le Fort III fractures may cause airway compromise due to posterior displacement of the midface. Maintain a high index of suspicion for intracranial injuries.
Facial Inspection
Visually assess the patient from all angles:
Look for facial asymmetry, flattening, or contour deformities.
Assess for ecchymosis:
Periorbital (“raccoon eyes”) in Le Fort II/III.
Subconjunctival hemorrhage without posterior limit—suggests orbital wall involvement.
Nasal deviation or depression.
Midface elongation or widening (especially in Le Fort III).
Open wounds, lacerations, or exposed bone.
Facial swelling—more pronounced in the maxillary region.
Bruising of the buccal sulcus may suggest Le Fort I fracture.
Palpation and Functional Tests
Carefully palpate the bony landmarks of the face, noting:
Step-offs: Irregularities in contour over orbital rim, zygoma, or infraorbital margin.
Crepitus: Crackling due to subcutaneous air—suggests sinus wall breach.
Mobility of bone segments:
Gently grasp the maxillary arch and attempt to move it—mobility suggests Le Fort fracture.
In Le Fort I, only the dental arch and hard palate move.
In Le Fort II, the central midface moves.
In Le Fort III, the entire face shifts—craniofacial disjunction.
Pain on palpation of the infraorbital rim or zygomatic arch.
Intraoral Examination
Essential for identifying fractures that affect the alveolar process, palate, or dental arch.
- Ecchymosis of the upper buccal sulcus—highly suggestive of Le Fort I.
- Palatal lacerations, splits, or hematomas.
- Tooth mobility or avulsion.
- Occlusal changes: Ask patient to bite—malocclusion is a critical finding.
- Open bite (inability to bring anterior teeth together) is common in maxillary fractures.
- Palpation of alveolar bone may reveal mobility or step deformities.
Ophthalmologic Assessment
The orbits are frequently involved in Le Fort II and III fractures. Rapid identification of ocular injuries is critical.
- Visual acuity (Snellen chart or quick bedside test)
- Pupillary responses (check for afferent pupillary defect—may indicate optic nerve injury)
- Diplopia (especially on upward gaze—suggests orbital floor or muscle entrapment)
- Enophthalmos or proptosis
- Restricted eye movement (check all 6 cardinal directions)
- Subconjunctival hemorrhage
- Palpable step-off of orbital rim
- Loss of infraorbital sensation (due to infraorbital nerve injury)
Nasal and Sinus Evaluation
Epistaxis is common but must be differentiated from more serious bleeding (e.g., posterior nasal bleeding or arterial injury).
Septal hematoma should be drained to prevent cartilage necrosis.
Check for:
Deviation of nasal septum
Crepitus or nasal dorsum mobility
CSF rhinorrhea (clear fluid from nose, often with “halo” sign on gauze)
Obstruction of nasal passages
Anterior or posterior sinus tenderness
Neurological Examination
- Infraorbital nerve (V2): sensation in midface, upper lip, and anterior cheek.
- Supratrochlear/supraorbital nerves (V1): forehead and upper eyelid.
- Facial nerve (VII): assess motor function of the face.
- Any cranial nerve deficits may indicate deeper skull base or intracranial involvement.
Evaluate for:
- Confusion, disorientation (may indicate concussion or brain injury)
- Loss of consciousness
- Seizures
- Posturing (sign of increased intracranial pressure)
Ear and Auditory Assessment
Fractures of the maxilla may affect structures connected to the ear.
- Hemotympanum (blood behind eardrum)
- Otorrhea (CSF leak from ear)
- Hearing loss
- Battle’s sign (ecchymosis behind the ear) in skull base fractures
Special Tests and Signs
- “Guerin’s Sign”: Bruising in the greater palatine area—indicative of Le Fort I.
- “Dish-face deformity”: Flattened midface seen in Le Fort II/III.
- “Tug test”: Gently pull the maxilla and assess for mobility.
- “Halo sign”: Used to detect CSF leakage—blood-tinged fluid on gauze develops a clear ring around the red center.
Clinical Pitfalls and Challenges
- Swelling may mask fracture mobility—repeat exam 24–48 hours later if uncertain.
- Conscious, uncooperative, or intubated patients make assessment difficult.
- Polytrauma may distract from facial injuries.
- Orbital symptoms may be subtle—require early ophthalmologic input.
Summary of Key Clinical Features by Le Fort Type
| Feature | Le Fort I | Le Fort II | Le Fort III |
|---|---|---|---|
| Maxillary mobility | Floating palate | Floating midface | Entire facial skeleton mobile |
| Occlusion | Malocclusion | Malocclusion | Severe malocclusion |
| Orbital involvement | No | Yes | Yes (extensive) |
| Infraorbital numbness | Sometimes | Common | Very common |
| CSF rhinorrhea | Rare | Possible | Common |
| Facial flattening | Mild | Moderate | Severe (“dish-face”) |
| Nasal symptoms | Minor | Prominent | Major |
| Ocular symptoms | Unlikely | Possible | Common (diplopia, vision loss) |
Diagnostic Imaging
Imaging is an indispensable component in the diagnosis and management of maxillary fractures. Given the complex three-dimensional anatomy of the midface and the variability in fracture patterns, high-quality imaging provides critical information that cannot be reliably obtained through physical examination alone.
A tailored imaging approach helps:
- Confirm the presence and extent of fracture.
- Classify the type of injury.
- Identify associated fractures and complications (e.g., orbital blowout, CSF leaks, dental injury).
- Guide surgical planning and fixation.
- Monitor healing or detect postoperative complications.
Principles of Imaging in Maxillofacial Trauma
When evaluating a patient with suspected maxillary fracture, imaging decisions should be guided by:
- Mechanism and severity of trauma
- Clinical signs and symptoms (e.g., facial mobility, visual changes, malocclusion)
- Need for surgical planning
- Availability of imaging technology
Imaging should cover the entire midface, and in cases of high-energy trauma, should extend to the skull base, orbits, mandible, and cervical spine.
Plain Radiographs (Conventional X-rays)
Although less commonly used today, plain radiographs still play a role in:
- Initial screening in limited-resource settings
- Follow-up imaging
- Dental and alveolar process fractures
Common Radiographic Views
| View | Purpose | Structures Visualized |
|---|---|---|
| Waters’ view (occipitomental) | Best for maxillary sinuses, orbital rims, zygoma | Maxilla, orbits, nasal cavity |
| Caldwell view (occipitofrontal) | Evaluates frontal sinuses and orbits | Ethmoid and frontal sinuses |
| Lateral skull | General overview | Cranial vault, maxilla (limited) |
| Submentovertex (SMV) view | Assesses zygomatic arches | Zygomatic arch, skull base |
| Panoramic (OPG) | Focuses on dental arch and alveolus | Teeth, alveolar processes, mandible |
Limitations of Plain Radiographs:
- Low sensitivity for detecting subtle or complex fractures.
- Poor evaluation of posterior structures, orbit, or skull base.
- Superimposition of anatomical landmarks can obscure fracture lines.
Computed Tomography (CT)
CT scanning is the gold standard for diagnosing maxillary fractures. It provides excellent detail of bony anatomy, allows multiplanar reconstruction, and is essential in surgical planning.
Indications for CT in Maxillary Trauma
- Suspected Le Fort, ZMC, or orbital fractures
- Polytrauma or unconscious patient
- Evidence of oculofacial trauma (diplopia, vision loss, periorbital swelling)
- Suspected cranial base injury (CSF rhinorrhea)
- High-velocity or penetrating trauma
- Preoperative planning
CT Protocol
- Thin slices (≤1 mm) for fine bone detail
- Axial, coronal, and sagittal planes
- 3D reconstructions for spatial orientation and operative planning
- Bone and soft tissue windows
- In some cases, contrast-enhanced CT may be used to assess vascular injuries or soft tissue involvement.
Advantages of CT:
Detects both displaced and non-displaced fractures
Identifies comminution, bone loss, and exact fracture lines
Highlights associated injuries to:
Orbit (blowout fractures, muscle entrapment)
Paranasal sinuses
Zygomatic arch and nasal bones
Pterygoid plates and skull base
Detects air-fluid levels in sinuses or subcutaneous emphysema
Assesses premaxillary and alveolar fractures
Common CT Findings in Maxillary Fractures:
- Disruption of maxillary sinus walls (anterior, posterior, medial)
- Infraorbital rim step-off
- Pterygoid plate fracture (key feature in Le Fort injuries)
- Orbital floor defects with herniation of fat or muscles
- Midface widening or rotation
Cone-Beam Computed Tomography (CBCT)
CBCT is increasingly used in dentomaxillofacial imaging, especially for:
- Alveolar and dental fractures
- Orthognathic surgery planning
- Postoperative evaluation
Advantages:
- Lower radiation dose than traditional CT
- Excellent spatial resolution for bony structures
- Compact, clinic-friendly units
Limitations:
- Limited soft tissue detail
- May not detect associated orbital or skull base injuries
- Not suitable for polytrauma evaluation
Magnetic Resonance Imaging (MRI)
MRI is not routinely used for primary diagnosis of maxillary fractures but is valuable in specific scenarios.
Indications:
- Suspected soft tissue or neural injuries
- Evaluation of extraocular muscle entrapment
- Orbital apex syndrome
- Optic nerve damage or globe rupture
- Assessment of chronic osteomyelitis or tumor-related fractures
Strengths:
- Superior soft tissue contrast
- No ionizing radiation
Limitations:
- Time-consuming
- Poor bony detail
- Susceptible to motion artifacts
- Not always available in emergency settings
Additional Imaging Modalities
Ultrasound
- Useful as a bedside tool for detecting orbital rim fractures or foreign bodies.
- Operator-dependent and limited to superficial structures.
Nuclear Medicine (Bone Scans)
Rarely used, but may help in detecting:
Non-union
Chronic infection
Occult fractures not visible on CT
Angiography (CT Angiogram or Conventional)
Reserved for suspected vascular injuries:
Internal maxillary artery bleed
Pseudoaneurysm
Arteriovenous fistula
May be required in massive epistaxis or expanding hematoma
Special Considerations in Imaging
Pediatric Patients
- Use low-dose protocols to minimize radiation.
- Be alert for greenstick fractures or subtle growth plate injuries.
- CBCT may be preferable for dentoalveolar trauma.
Elderly Patients
- Bone density is often lower—non-displaced fractures may be missed.
- Include full-face imaging to exclude associated fractures.
Polytrauma Patients
Use whole-body CT (pan-scan) including:
Head
Cervical spine
Chest/abdomen/pelvis
Look for synchronous cranial, spinal, or thoracic injuries
Summary of Imaging Modalities
| Modality | Best for | Limitations |
|---|---|---|
| Plain X-ray | Quick screening, dental fractures | Poor detail, overlapping structures |
| CT scan | Gold standard for facial fractures | Radiation exposure |
| CBCT | Dental/alveolar detail, low dose | Poor soft tissue assessment |
| MRI | Neural/soft tissue evaluation | Not for acute bony injuries |
| Ultrasound | Quick, bedside use | Limited penetration |
| Angiography | Vascular trauma | Invasive, requires expertise |
Imaging in Surgical Planning
Modern surgery for maxillary fractures benefits greatly from preoperative 3D planning using CT data:
- Virtual simulations help assess bone loss and displacement.
- Custom titanium plates or 3D-printed implants can be fabricated.
- Surgical guides improve precision and outcomes.
- Postoperative imaging is used to confirm hardware placement and alignment restoration.
Management of Maxillary Fractures
The management of maxillary fractures requires a comprehensive, stepwise, and often multidisciplinary approach. The goals of treatment include:
- Restoring the structural integrity of the facial skeleton.
- Re-establishing functional occlusion.
- Preserving or restoring facial aesthetics.
- Ensuring normal airway, mastication, vision, and speech.
- Preventing early and late complications.
Treatment depends on multiple factors:
- Type and classification of fracture
- Displacement and comminution
- Involvement of adjacent structures (orbit, nasal cavity, skull base)
- Associated injuries (cranial, cervical, dental, orbital, etc.)
- Patient’s age, general health, and comorbidities
Principles of Management
The foundational principles in the treatment of maxillary fractures include:
- Reduction: Realignment of fractured bone segments into their original anatomical positions.
- Fixation: Stabilization of the fracture using internal or external devices to maintain reduction during healing.
- Immobilization: Restriction of movement to allow proper healing (especially important in dentoalveolar fractures).
- Rehabilitation: Restoration of function through physical therapy, dental reconstruction, speech therapy, etc.
Initial Stabilization and Emergency Management
In the acute trauma setting, the first priority is the ABC approach (Airway, Breathing, Circulation).
1. Airway Management
Maxillary fractures, especially Le Fort II and III, may result in posterior displacement of the midface, leading to airway obstruction.
Early intubation or tracheostomy may be required in:
Severe midface collapse
Profuse nasal/oral bleeding
Impending airway compromise
2. Hemorrhage Control
- Nasal and oral bleeding is common.
- Apply anterior and posterior nasal packing or balloon tamponade.
- If persistent, consider arterial ligation or embolization of the internal maxillary artery.
3. Cervical Spine Precautions
- Always assume cervical spine injury in high-velocity trauma.
- Keep the neck immobilized until ruled out with imaging.
4. Nutritional Support
Patients with restricted oral intake may require:
- Nasogastric tube feeding
- Parenteral nutrition
- Dietician referral postoperatively
Definitive Management
Once the patient is stabilized, definitive management should be initiated as early as feasible—ideally within the first 7–10 days post-injury, before fibrous union begins.
Surgical Management
Surgery is the mainstay of treatment for most displaced or complex maxillary fractures.
Indications for Surgery
- Displaced Le Fort I, II, or III fractures
- Malocclusion due to fracture
- Orbital floor involvement (blowout fracture)
- CSF leak from skull base involvement
- Comminuted fractures requiring rigid fixation
- Significant esthetic deformity
- Dental arch instability or palatal split
Timing of Surgery
- Ideally performed within 72 hours to 7 days.
- Earlier intervention facilitates easier reduction and better outcomes.
- In polytrauma patients, surgery may be delayed for medical stabilization.
Open Reduction and Internal Fixation (ORIF)
Uses titanium plates and screws to stabilize fracture segments.
Follows the principle of buttress reconstruction, restoring the facial skeleton’s load-bearing architecture:
Vertical buttresses: Nasomaxillary, zygomaticomaxillary, pterygomaxillary
Horizontal buttresses: Frontal bar, infraorbital rim, alveolar ridge
Surgical Approaches
| Approach | Access To | Comments |
|---|---|---|
| Intraoral (vestibular) | Alveolar ridge, Le Fort I | Minimal scarring, good for anterior access |
| Subciliary/transconjunctival | Infraorbital rim, orbital floor | Used in Le Fort II/III, often with canthotomy |
| Coronal flap | Zygomatic arches, frontal bone | Extensive access, useful in Le Fort III |
| Midfacial degloving | Entire midface | Scarless approach, used in panfacial trauma |
| Gillies temporal | Zygomatic arch | Closed reduction of zygoma fractures |
Orbital Floor Reconstruction
Often necessary in Le Fort II/III or blowout fractures.
Materials used:
Titanium mesh
Porous polyethylene (Medpor)
Resorbable plates
Autologous bone grafts (calvarial, iliac)
Maxillomandibular Fixation (MMF)
- Temporary occlusion control using arch bars, screws, elastics, or IMF wires.
- Ensures dental alignment and bite stabilization during healing.
Bone Grafting
Used in:
Segmental loss of bone
Delayed union or non-union
Complex comminuted fractures
Common donor sites: Iliac crest, calvaria, mandibular symphysis
Non-Surgical Management
Some fractures can be managed conservatively, particularly when:
- The fracture is non-displaced.
- Occlusion is unaffected.
- The patient is medically unfit for surgery.
- Pediatric patients with high remodeling potential.
Conservative Measures Include:
- Soft or liquid diet
- Oral hygiene maintenance
- Analgesia and anti-inflammatories
- Antibiotics (especially for sinus-involving fractures)
- Close monitoring with serial imaging
Management by Fracture Type
| Fracture Type | Management Strategy |
|---|---|
| Le Fort I | ORIF via intraoral approach ± MMF |
| Le Fort II | ORIF via intraoral and orbital approach; restore infraorbital rim and orbital floor |
| Le Fort III | ORIF via coronal, intraoral, and orbital approaches; rigid fixation to cranial base |
| Alveolar fracture | Dental splinting or arch bar stabilization; conservative for minor cases |
| Orbital floor (“blowout”) | Immediate repair if entrapment; otherwise within 2 weeks |
| Comminuted fractures | Multi-staged surgery; may require external fixation, grafts, or custom implants |
Postoperative Care
Medications
- Broad-spectrum antibiotics (e.g., amoxicillin-clavulanate)
- Nasal decongestants to reduce sinus edema
- Analgesics and anti-inflammatory drugs
- Steroids to control orbital swelling (e.g., dexamethasone)
Wound Care
- Maintain oral hygiene to prevent infection.
- Irrigation of sinus openings or lacerations as needed.
Diet
- Soft diet for 2–4 weeks to prevent stress on fracture sites.
- Adequate hydration and nutrition are critical for healing.
Follow-Up Imaging
- Postoperative CT scan to confirm alignment and fixation.
- Long-term follow-up to monitor for malunion, nonunion, or sinus complications.
Multidisciplinary Collaboration
Optimal management often involves:
- Maxillofacial surgeons
- Neurosurgeons (for skull base or brain injury)
- Ophthalmologists (for orbital trauma or vision loss)
- ENT specialists (for nasal and sinus reconstruction)
- Dentists or orthodontists (for occlusion and rehabilitation)
- Anesthesiologists and intensivists (for airway and sedation management)
Delayed or Secondary Reconstruction
In cases of:
- Missed fractures
- Failed primary repair
- Late deformities
Surgical revision may involve:
- Osteotomies
- Bone grafting
- Facial implants
- Orthognathic surgery
Postoperative Care and Rehabilitation
Effective postoperative care and rehabilitation are critical components in the overall management of maxillary fractures. While surgical or non-surgical intervention addresses the acute phase, recovery involves restoring full function, aesthetics, and quality of life. Postoperative care aims to ensure optimal healing, prevent complications, manage discomfort, and reestablish normal orofacial activities such as speaking, chewing, and facial expression.
This phase demands multidisciplinary collaboration, close follow-up, and patient engagement to achieve lasting functional and cosmetic outcomes.
Goals of Postoperative Care
- Promote bone and soft tissue healing
- Maintain stable occlusion
- Prevent or treat infection
- Monitor for complications (e.g., sinusitis, malunion)
- Manage pain and swelling
- Facilitate nutritional intake and oral hygiene
- Restore facial function and aesthetics
- Support psychosocial recovery
Immediate Postoperative Period (First 72 Hours)
Pain and Swelling Management
Analgesia:
NSAIDs (e.g., ibuprofen) for inflammation
Paracetamol for baseline pain
Opioids (short-term use only) for severe pain
Cold therapy:
Ice packs applied intermittently for the first 24–48 hours reduce swelling and hematoma formation.
Steroids:
Short courses of corticosteroids (e.g., dexamethasone) may be prescribed to reduce facial edema, especially in cases involving orbital or periorbital swelling.
Head Elevation
Keep the head elevated (30–45°) during rest and sleep to reduce facial edema and venous congestion.
Antibiotic Therapy
Prophylactic antibiotics are commonly prescribed, particularly in:
Fractures involving the sinus cavity
Open or contaminated wounds
Post-surgical implant placements
Common choices include:
Amoxicillin-clavulanate
Clindamycin (for penicillin-allergic patients)
Metronidazole (if anaerobic coverage needed)
Nasal and Sinus Care
- Decongestants (e.g., oxymetazoline nasal spray) may reduce mucosal swelling.
- Saline nasal irrigation helps keep the nasal passages clear.
- Avoid nose blowing for at least 2 weeks to prevent disruption of repair and potential air embolism.
Eye Protection
For orbital involvement, advise:
- Avoiding pressure on the eye.
- Wearing protective eye shields.
- Referral to ophthalmology for ongoing monitoring (especially for diplopia, visual acuity loss, or enophthalmos).
Wound and Suture Care
Intraoral incisions require strict oral hygiene:
- Rinse with chlorhexidine gluconate 0.12% mouthwash twice daily.
- Use soft toothbrushes to clean teeth gently.
Extraoral incisions:
- Keep dry and clean.
- Monitor for signs of infection, dehiscence, or hematoma.
- Sutures typically removed after 5–7 days (non-absorbable types).
Nutrition and Feeding
Diet Modifications
Initial liquid or pureed diet for 1–2 weeks.
Gradual progression to soft diet (mashed potatoes, soft pasta, scrambled eggs).
Avoid:
Hard or crunchy foods (nuts, raw vegetables).
Sticky foods (gum, caramel).
Hot beverages immediately post-surgery.
Nutritional Support
In patients with maxillomandibular fixation (MMF), consider:
- Nutrient-dense liquid supplements (e.g., Ensure, Boost).
- Use of feeding syringes or straws.
- Dietician referral to monitor caloric intake.
Oral Hygiene
Maintaining oral cleanliness is vital to prevent postoperative infections, especially in intraoral or alveolar fractures.
Brush teeth and appliances gently.
Use prescription fluoride toothpaste if prescribed.
Rinse after every meal with warm saline or antiseptic solution.
Dental professionals may assist with:
Cleaning around arch bars or splints.
Providing interdental brushes or water flossers.
Physical Therapy and Functional Recovery
Jaw Mobility Exercises
Begin gentle range-of-motion exercises (under guidance) after fixation removal.
Prevents trismus and improves speech, chewing, and oral hygiene.
May involve:
Passive mouth-opening tools (TheraBite)
Mirror therapy and biofeedback
Regular assessment of interincisal distance
Speech Therapy
Indicated in patients with:
- Velopharyngeal dysfunction post-palatal injury
- Nasal speech or articulation problems
- Involvement of maxillary sinus, hard palate, or zygoma
Postoperative Imaging and Follow-Up
Imaging Protocols
Postoperative CT or panoramic radiographs may be ordered to:
- Confirm alignment and hardware positioning.
- Assess sinus integrity and orbital reconstruction.
- Monitor bone healing or identify complications.
Follow-Up Schedule
- 1 week: Suture removal, wound inspection.
- 2–3 weeks: Assess healing, check occlusion, begin jaw exercises.
- 6–8 weeks: Evaluate bony union, remove arch bars/MMF.
- 3–6 months: Monitor for long-term complications, plan secondary procedures if needed.
Psychological and Social Support
Facial trauma can result in significant psychological distress. Patients may experience:
- Depression, anxiety, or PTSD
- Body image concerns
- Fear of eating, speaking, or socializing
Support options:
- Mental health referral for counseling or cognitive behavioral therapy.
- Peer support groups or trauma recovery programs.
- Reassurance and clear communication from healthcare providers regarding prognosis and expected outcomes.
Common Postoperative Complications and Management
| Complication | Signs/Symptoms | Management |
|---|---|---|
| Infection | Fever, swelling, purulent discharge | Antibiotics, possible drainage |
| Malocclusion | Bite misalignment | Orthodontic correction or surgical revision |
| Nonunion or malunion | Persistent pain, asymmetry, instability | Reoperation, grafting, osteotomy |
| Sinusitis | Nasal obstruction, facial pressure, discharge | Decongestants, antibiotics, ENT referral |
| Oroantral fistula | Nasal regurgitation, air passage into mouth | Surgical closure (buccal or palatal flap) |
| Vision problems | Diplopia, blurred vision, decreased acuity | Ophthalmology referral, orbital revision |
| Trismus | Jaw stiffness, pain with opening | Physiotherapy, muscle relaxants |
Return to Activity and Work
- Light activity may resume within 1–2 weeks post-surgery.
- Avoid contact sports, lifting heavy objects, or straining for 4–6 weeks.
- Driving may resume after discontinuing narcotic pain medications and regaining full vision and alertness.
- Work clearance depends on the occupation (e.g., earlier return for desk jobs vs. manual labor).
Long-Term Considerations and Reconstruction
In cases with residual deformity or functional issues:
- Delayed reconstructive surgery may be considered.
- Dental implants or prosthetics for missing teeth.
- Orthognathic surgery if occlusion remains abnormal.
- Scar revision for visible disfigurement.
Complications of Maxillary Fractures
Despite advances in imaging, surgical techniques, and postoperative care, maxillary fractures carry a significant risk of complications. These can result from the initial trauma, surgical intervention, or delayed healing, and may affect function, aesthetics, or overall health.
Complications can be categorized as:
- Immediate (within 24–72 hours)
- Early (within the first month)
- Late (months to years post-injury)
Early recognition and prompt management are crucial to minimize morbidity and improve long-term outcomes.
Immediate Complications
These occur at the time of injury or during the acute phase of treatment.
Airway Obstruction
Cause: Posterior displacement of fractured maxilla (especially in Le Fort II/III), blood, or soft tissue swelling.
Signs: Stridor, dyspnea, hypoxia, gurgling sounds.
Management:
Immediate airway support (intubation or tracheostomy).
Suctioning and hemostasis.
Elevate head to reduce edema.
Hemorrhage
Cause: Disruption of the facial arterial supply (e.g., internal maxillary artery, sphenopalatine artery).
Signs: Profuse epistaxis, hematoma formation, hypotension.
Management:
Anterior/posterior nasal packing.
Balloon tamponade (e.g., Foley catheter).
Surgical or endovascular ligation of bleeding vessel.
Cerebrospinal Fluid (CSF) Leak
Cause: Skull base fracture, particularly in Le Fort III or ethmoid plate fractures.
Signs:
Clear, watery rhinorrhea (especially unilateral).
Halo sign on gauze.
Positivity on β2-transferrin test.
Risks: Meningitis, pneumocephalus.
Management:
Elevation of head, bed rest.
Avoid nose blowing or Valsalva.
Lumbar drain or surgical repair if persistent (>7 days).
Globe Injury and Vision Loss
Cause: Orbital trauma, optic nerve damage, globe rupture.
Signs:
Sudden vision loss.
Proptosis or enophthalmos.
Restricted extraocular movement.
Management:
Emergent ophthalmologic evaluation.
High-dose corticosteroids (controversial).
Orbital decompression or nerve decompression if indicated.
Early Complications (First 4 Weeks)
Infection
Sites:
Sinus cavity (sinusitis)
Surgical wounds
Hardware-related infection
Signs: Fever, swelling, purulent discharge, localized tenderness.
Prevention:
Prophylactic antibiotics.
Sterile surgical technique.
Management:
Oral or IV antibiotics.
Drainage or debridement if abscess or osteomyelitis.
Hardware removal if necessary.
Malocclusion
Cause: Inadequate fracture reduction or stabilization.
Signs:
Misaligned bite.
Difficulty chewing or speaking.
Management:
Early adjustment of fixation or occlusion.
MMF or revision surgery.
Orthodontic consultation.
Trismus
Cause: Muscle injury, pain, fibrosis, or temporomandibular joint (TMJ) involvement.
Signs:
Restricted mouth opening.
Pain with chewing or yawning.
Management:
Analgesics and muscle relaxants.
Physical therapy and jaw stretching exercises.
Botulinum toxin in refractory cases.
Sensory Nerve Injuries
Most commonly affected: Infraorbital nerve (branch of CN V2).
Signs:
Numbness or tingling of the cheek, upper lip, or upper teeth.
Can persist for months or become permanent.
Management:
Observation (most cases resolve spontaneously).
Neurotrophic agents (e.g., B-vitamins).
Microsurgical repair (rare).
Late Complications (Weeks to Years Post-Injury)
Malunion or Nonunion
Cause: Inadequate reduction or fixation, infection, smoking, systemic illness.
Signs:
Facial asymmetry.
Persistent pain or instability.
Radiographic evidence of poor healing.
Management:
Surgical re-osteotomy and refixation.
Bone grafting if necessary.
Removal and replacement of failed hardware.
Persistent Sinusitis
Cause: Disruption of sinus drainage pathways.
Signs:
Facial pressure or fullness.
Purulent nasal discharge.
Headache or postnasal drip.
Management:
Antibiotics.
Nasal decongestants or steroids.
Functional endoscopic sinus surgery (FESS) in chronic cases.
Oroantral Fistula
Cause: Communication between oral cavity and maxillary sinus, often following alveolar fractures or tooth extraction.
Signs:
Passage of fluid/air from mouth to nose.
Nasal regurgitation during swallowing.
Whistling sound when speaking.
Management:
Small fistulas may close spontaneously.
Surgical closure using:
Buccal advancement flap.
Palatal flap.
Buccal fat pad graft.
Enophthalmos or Diplopia
Cause: Orbital floor malunion, loss of orbital volume, muscle entrapment.
Signs:
Sunken globe (enophthalmos).
Double vision (especially on upward gaze).
Gaze restriction.
Management:
Orbital floor reconstruction.
Release of entrapped muscle.
Orbital implants for volume restoration.
Facial Deformity
Cause: Malpositioned bone fragments, soft tissue loss, scarring.
Signs:
Flattened midface.
Asymmetry of cheeks or nose.
Residual scars.
Management:
Secondary reconstructive surgery.
Autologous fat grafting or implants.
Scar revision and dermatological treatments.
Dental Sequelae
Common issues:
Tooth loss or fracture.
Pulp necrosis.
Periodontal disease due to poor hygiene or trauma.
Management:
Dental splinting, root canal therapy.
Tooth replacement with implants, bridges, or dentures.
Orthodontic alignment if needed.
Risk Factors for Complications
| Risk Factor | Associated Complications |
|---|---|
| Smoking | Nonunion, infection, delayed healing |
| Diabetes | Infection, poor wound healing |
| Immunosuppression | Chronic infection, osteomyelitis |
| Poor oral hygiene | Dental infections, osteitis |
| Delayed treatment | Malunion, cosmetic defects |
| Inadequate fixation | Instability, malocclusion |
Prevention Strategies
- Preoperative planning with high-resolution CT imaging and 3D reconstruction.
- Meticulous surgical technique, including proper reduction and fixation.
- Prophylactic antibiotics for sinus and intraoral injuries.
- Strict postoperative care including hygiene, nutrition, and early follow-up.
- Patient education on activity restrictions, signs of complications, and oral care.
Long-Term Outcomes
Most patients recover well with appropriate management. Key determinants of a favorable prognosis include:
- Early and accurate diagnosis.
- Surgical expertise and fixation quality.
- Patient adherence to follow-up and rehab.
- Timely intervention in the event of complications.
Residual functional or aesthetic issues may persist in some patients, necessitating revision procedures, cosmetic surgery, or dental rehabilitation.