Liver diseases present significant challenges in the field of dentistry, requiring careful consideration and management to avoid complications and ensure patient safety. The liver plays a crucial role in various physiological processes, including metabolism, detoxification, and synthesis of clotting factors. Consequently, any compromise in liver function can have far-reaching implications for dental treatment. This article will explore the various liver diseases relevant to dentistry, their impact on dental procedures, and the necessary precautions and modifications that must be made to provide safe and effective care.
Table of Contents
ToggleOverview of Liver Diseases
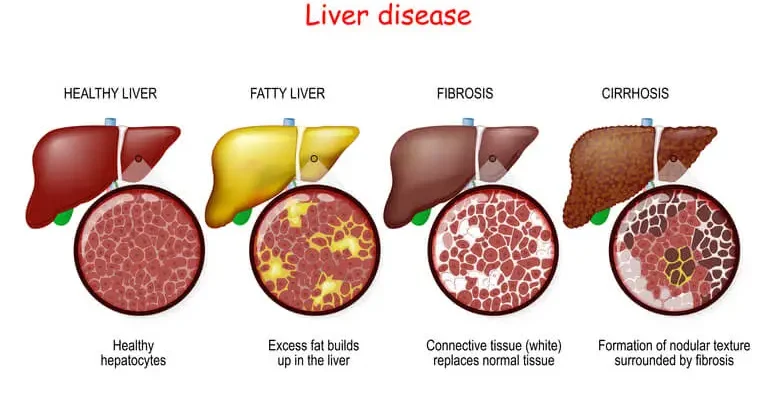
Liver diseases encompass a wide range of conditions that can affect the liver’s structure and function. These include viral hepatitis, cirrhosis, liver cancer, alcoholic liver disease, and non-alcoholic fatty liver disease (NAFLD), among others. Each of these conditions can impact dental treatment in different ways, necessitating a tailored approach to patient care.
Viral Hepatitis
Viral hepatitis, primarily hepatitis B (HBV) and hepatitis C (HCV), is a significant concern in dentistry due to its potential for transmission and its effects on liver function. Both HBV and HCV can lead to chronic liver disease, cirrhosis, and hepatocellular carcinoma. Dentists must be aware of the transmission risks, as these viruses can be spread through blood and saliva, making strict infection control protocols essential.
Impact on Dental Treatment
Patients with chronic hepatitis may present with impaired liver function, which can affect drug metabolism, bleeding tendencies, and immune response. Dentists must take these factors into account when planning treatment. For example, drugs that are metabolized by the liver, such as certain analgesics, antibiotics, and anesthetics, may require dosage adjustments or alternatives to avoid toxicity.
Bleeding tendencies in patients with hepatitis are of particular concern. The liver produces several clotting factors, and liver dysfunction can lead to coagulopathy, increasing the risk of excessive bleeding during dental procedures. Therefore, assessing the patient’s clotting status, including prothrombin time (PT) and international normalized ratio (INR), is crucial before performing any invasive procedures.
Cirrhosis
Cirrhosis is the end-stage of chronic liver disease, characterized by extensive fibrosis and liver dysfunction. It can result from various causes, including chronic viral hepatitis, alcoholic liver disease, and NAFLD. Cirrhosis is associated with numerous complications, such as portal hypertension, variceal bleeding, ascites, and hepatic encephalopathy, all of which can impact dental care.
Impact on Dental Treatment
Patients with cirrhosis are at high risk for bleeding due to reduced production of clotting factors and thrombocytopenia, which results from splenic sequestration of platelets. Dentists must be vigilant in assessing bleeding risk and may need to consult with the patient’s physician to determine the safety of invasive procedures.
Portal hypertension, a common complication of cirrhosis, can lead to the development of varices, particularly in the esophagus and stomach. Although less common, oral varices can also occur and pose a risk of bleeding during dental treatment. Careful examination of the oral cavity for signs of varices is important in these patients.
Cirrhosis can also affect drug metabolism, necessitating adjustments in drug dosages to prevent toxicity. Additionally, patients with cirrhosis may have compromised immune function, making them more susceptible to infections. Dentists should consider prophylactic antibiotics for certain procedures and ensure meticulous infection control.
Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD is a spectrum of liver diseases ranging from simple steatosis (fatty liver) to non-alcoholic steatohepatitis (NASH), which can progress to cirrhosis and liver failure. NAFLD is strongly associated with obesity, diabetes, and metabolic syndrome, making it increasingly common in the general population.
Impact on Dental Treatment
The implications of NAFLD in dentistry are similar to those of other liver diseases, with concerns about bleeding, drug metabolism, and infection risk. However, the association of NAFLD with metabolic syndrome means that patients may also have other comorbidities, such as hypertension and cardiovascular disease, which require careful consideration in treatment planning.
Dentists should be aware that NAFLD may not always be diagnosed in its early stages, as it can be asymptomatic. Therefore, a thorough medical history and assessment of risk factors are important in identifying patients who may have undiagnosed liver disease.
Alcoholic Liver Disease
Chronic alcohol consumption is a leading cause of liver disease, ranging from fatty liver to alcoholic hepatitis and cirrhosis. Alcoholic liver disease is associated with a high risk of bleeding, malnutrition, and immunosuppression, all of which can complicate dental care.
Impact on Dental Treatment
Patients with alcoholic liver disease may present with poor oral hygiene, periodontal disease, and a higher incidence of oral cancer. Dentists should be vigilant in screening for oral lesions and providing appropriate oral hygiene education and interventions.
The management of bleeding risk is critical in these patients, particularly if they have cirrhosis. Dentists should assess clotting status and consider using local hemostatic measures, such as sutures, topical thrombin, or tranexamic acid, to minimize bleeding during procedures.
Alcohol can also interact with many medications used in dentistry, including sedatives, analgesics, and antibiotics. Dentists should avoid prescribing medications that may have harmful interactions with alcohol or that are metabolized by the liver, opting for alternatives when necessary.
Liver Cancer
Primary liver cancer, such as hepatocellular carcinoma, often arises in the context of chronic liver disease, particularly cirrhosis. The management of liver cancer may involve surgery, chemotherapy, and radiotherapy, all of which can have implications for dental care.
Impact on Dental Treatment
Patients with liver cancer may have compromised liver function, affecting drug metabolism and bleeding risk. Additionally, those undergoing chemotherapy or radiotherapy may experience oral mucositis, xerostomia, and increased susceptibility to infections.
Dentists should work closely with the patient’s oncologist to coordinate care and manage the side effects of cancer treatment. Preventive dental care, including fluoride treatments and the use of saliva substitutes, can help mitigate the oral complications of cancer therapy.
Considerations for Liver diseases in Dental Treatment Planning
When treating patients with liver disease, dentists must take a comprehensive approach to treatment planning, considering the patient’s overall health, liver function, and potential complications. The following are key considerations in dental treatment planning for these patients:
- Medical History and Liver Function Assessment
- Risk of Bleeding
- Drug Metabolism and Dosage Adjustments
- Infection Control and Prophylaxis
- Management of Oral Complications
- Multidisciplinary Collaboration
- Patient Education and Communication
- Emergency Preparedness
Medical History and Liver Function Assessment
A thorough medical history is essential for identifying patients with liver disease. Dentists should inquire about any history of liver disease, alcohol consumption, viral hepatitis, and other risk factors. If liver disease is suspected, further assessment of liver function may be warranted, including laboratory tests such as liver function tests (LFTs), PT, INR, and platelet count.
In some cases, collaboration with the patient’s physician may be necessary to obtain a complete understanding of the patient’s liver status and to determine the need for any additional diagnostic tests or imaging studies.
Risk of Bleeding
Bleeding risk is a major concern in patients with liver disease, particularly those with cirrhosis. Dentists should assess clotting status using PT, INR, and platelet count before performing any invasive procedures. If the INR is elevated or platelet count is low, consultation with the patient’s physician is recommended to determine the need for any preoperative measures, such as vitamin K administration, platelet transfusion, or the use of antifibrinolytic agents.
Local hemostatic measures, such as sutures, topical thrombin, and tranexamic acid mouthwash, can be used to control bleeding during and after procedures. It is also advisable to schedule procedures in the morning when clotting factors may be at their peak and to limit the extent of surgery to minimize the risk of bleeding.
Drug Metabolism and Dosage Adjustments
Liver disease can significantly impact the metabolism of drugs commonly used in dentistry, such as local anesthetics, analgesics, antibiotics, and sedatives. Dentists must be aware of the potential for drug accumulation and toxicity in patients with impaired liver function and adjust dosages accordingly.
For example, local anesthetics like lidocaine are metabolized in the liver, and reduced dosages may be necessary to prevent systemic toxicity. Similarly, nonsteroidal anti-inflammatory drugs (NSAIDs) should be used with caution, as they can exacerbate liver dysfunction and increase the risk of gastrointestinal bleeding.
When prescribing antibiotics, dentists should consider the patient’s liver function and choose agents that are less hepatotoxic. Amoxicillin, for example, is generally considered safe in patients with liver disease, while drugs like metronidazole and tetracyclines should be used with caution or avoided altogether.
Infection Control and Prophylaxis
Patients with liver disease, particularly those with cirrhosis or undergoing cancer treatment, may have compromised immune function and are at increased risk of infections. Dentists should adhere to strict infection control protocols to prevent the transmission of bloodborne pathogens and other infections.
In some cases, prophylactic antibiotics may be indicated to prevent infective endocarditis or other systemic infections. The decision to use prophylaxis should be based on the patient’s overall health, the type of procedure being performed, and current guidelines.
Management of Oral Complications
Liver disease can lead to a variety of oral manifestations, including jaundice, petechiae, gingival bleeding, and oral infections. In patients with chronic liver disease, oral hygiene may be compromised, leading to an increased risk of periodontal disease and caries.
Dentists should provide comprehensive oral hygiene education and preventive care to these patients, including regular dental cleanings, fluoride treatments, and the use of antimicrobial mouthwashes. For patients with xerostomia, saliva substitutes and other palliative measures can help manage dry mouth and reduce the risk of dental caries.
Patients undergoing treatment for liver cancer may experience oral mucositis, a painful inflammation and ulceration of the mucous membranes, as a side effect of chemotherapy or radiation therapy. Dentists can help manage mucositis by recommending gentle oral care practices, such as the use of soft-bristled toothbrushes, non-alcoholic mouthwashes, and avoiding irritants like spicy or acidic foods. Topical anesthetics or protective coating agents may also be prescribed to alleviate pain and discomfort associated with mucositis.
Multidisciplinary Collaboration
Effective management of patients with liver disease in a dental setting often requires collaboration with other healthcare professionals, including hepatologists, primary care physicians, and oncologists. This multidisciplinary approach ensures that the patient’s overall health is taken into account when planning and executing dental treatment.
For example, in patients with cirrhosis who require invasive dental procedures, it may be necessary to coordinate with the patient’s physician to manage bleeding risk through preoperative administration of clotting factors or platelets. In the case of patients undergoing chemotherapy for liver cancer, coordination with the oncologist is important to time dental treatments appropriately, ideally when the patient’s blood counts are stable and the risk of infection is lower.
Patient Education and Communication
Patient education is a critical component of dental care for individuals with liver disease. Patients should be informed about the potential oral complications of their condition and the importance of maintaining good oral hygiene. Dentists should take the time to explain the specific risks associated with their liver disease, such as bleeding tendencies and infection risk, and the need for regular dental check-ups.
Clear communication is also essential when discussing treatment plans and potential modifications. For instance, patients should be made aware of the reasons behind any adjustments in medication dosages or the need for additional tests before undergoing dental procedures. Providing written instructions or educational materials can help reinforce these points and ensure that patients understand the importance of following their dentist’s recommendations.
Emergency Preparedness
Dentists treating patients with liver disease should be prepared to manage potential emergencies that may arise during dental procedures. This includes being ready to control unexpected bleeding, manage adverse drug reactions, and address any signs of infection promptly.
Having a well-equipped dental office with the necessary emergency supplies, such as local hemostatic agents, epinephrine, and oxygen, is crucial. Dentists should also have protocols in place for handling emergencies and know when to refer patients to a medical facility for further care.
Oral Manifestations of Liver Diseases
Liver disease can present with a variety of oral manifestations, some of which may be the first signs of underlying systemic issues. Recognizing these oral signs can help dentists identify liver disease early and refer patients for appropriate medical evaluation and treatment.
- Jaundice
- Petechiae and Ecchymoses
- Gingival Bleeding
- Glossitis and Atrophic Tongue
- Oral Candidiasis
Jaundice
Jaundice, characterized by yellowing of the skin and mucous membranes, is a common sign of liver dysfunction. In the oral cavity, jaundice may present as yellow discoloration of the soft tissues, including the hard palate, gingiva, and tongue. This discoloration is due to the accumulation of bilirubin, a byproduct of hemoglobin breakdown that is normally processed by the liver.
While jaundice is not specific to any particular liver disease, its presence should prompt further investigation into the patient’s liver function. Dentists should be aware of this sign and consider referring the patient for medical evaluation if jaundice is observed during a dental examination.
Petechiae and Ecchymoses
Petechiae (small red or purple spots) and ecchymoses (larger bruises) may appear in the oral cavity of patients with liver disease, particularly those with coagulopathy or thrombocytopenia. These lesions result from minor trauma to the blood vessels in the mucous membranes, which are unable to properly clot due to impaired liver function.
In the context of dentistry, these lesions may be mistaken for trauma-related injuries, so it is important to take a thorough history to determine if they are related to underlying liver disease. The presence of petechiae or ecchymoses should raise concerns about the patient’s bleeding risk, and appropriate precautions should be taken during dental procedures.
Gingival Bleeding
Patients with liver disease, especially those with cirrhosis, may experience spontaneous gingival bleeding or prolonged bleeding after minor trauma, such as brushing or flossing. This is due to the impaired synthesis of clotting factors by the liver and the associated thrombocytopenia.
Dentists should be vigilant in assessing the extent of gingival bleeding and consider it a potential indicator of liver dysfunction. In such cases, a referral to the patient’s physician for further evaluation of liver function and coagulation status may be necessary.
Glossitis and Atrophic Tongue
Glossitis, or inflammation of the tongue, and atrophic changes in the tongue’s surface (smooth, red tongue) can occur in patients with liver disease due to nutritional deficiencies. Liver disease, particularly cirrhosis, is often associated with malabsorption of nutrients, including B vitamins and iron, which are essential for maintaining healthy mucous membranes.
These oral changes may present as a smooth, shiny, and erythematous (red) tongue, sometimes accompanied by a burning sensation or sensitivity to certain foods. Dentists should consider the possibility of liver disease or nutritional deficiencies in patients presenting with these symptoms and refer them for further medical assessment if indicated.
Oral Candidiasis
Oral candidiasis, a fungal infection caused by Candida species, is more common in patients with liver disease, especially those with compromised immune function or who are undergoing cancer treatment. The condition typically presents as white, curd-like plaques on the mucous membranes, which can be scraped off, leaving a red, sometimes bleeding surface.
In patients with liver disease, oral candidiasis may be more difficult to manage due to the underlying immunosuppression. Dentists should treat oral candidiasis promptly with antifungal agents, and in recurrent cases, consider investigating potential systemic causes, including liver dysfunction.
Special Considerations for Dental Anesthesia
The administration of local anesthesia in patients with liver disease requires special consideration due to the potential for altered drug metabolism and increased sensitivity to certain anesthetics. Local anesthetics like lidocaine are metabolized in the liver, and patients with impaired liver function may be at higher risk for systemic toxicity.
- Choice of Anesthetic Agent
- Dosage Adjustments
- Use of Vasoconstrictors
Choice of Anesthetic Agent
When selecting a local anesthetic for patients with liver disease, dentists should consider using agents that are less dependent on hepatic metabolism. For example, articaine is primarily metabolized by plasma esterases and may be a safer choice for these patients. However, its use should still be approached with caution, and the lowest effective dose should be administered.
Dosage Adjustments
Given the potential for reduced drug clearance in patients with liver disease, it is important to adjust the dosage of local anesthetics accordingly. Dentists should use the minimum effective dose to achieve adequate anesthesia while minimizing the risk of toxicity.
Use of Vasoconstrictors
Vasoconstrictors, such as epinephrine, are commonly added to local anesthetics to prolong their effect and reduce bleeding. However, in patients with advanced liver disease, the use of vasoconstrictors should be approached with caution due to the potential for cardiovascular side effects, such as increased blood pressure and arrhythmias.
Dentists should consider using a lower concentration of epinephrine or avoiding it altogether in patients with severe liver disease. The patient’s cardiovascular status should also be assessed before administering any anesthetic containing vasoconstrictors.
Frequently Asked Questions (FAQs)
How does liver disease affect dental treatment?
Liver disease can significantly impact dental treatment due to its effects on blood clotting, drug metabolism, and immune function. Patients with liver disease often have a reduced ability to form blood clots, increasing the risk of prolonged bleeding during and after dental procedures. Additionally, many medications commonly used in dentistry, such as analgesics, antibiotics, and local anesthetics, are metabolized in the liver, requiring dosage adjustments or alternative drug choices. Moreover, individuals with liver disease may have a weakened immune response, increasing their susceptibility to infections following dental procedures.
What to consider for anesthesia with liver disease?
When administering anesthesia to patients with liver disease, careful selection and dosage adjustments of anesthetic agents are crucial. The liver is responsible for metabolizing many anesthetic drugs, and its dysfunction can lead to prolonged drug effects or toxicity. Short-acting anesthetics and those with extrahepatic metabolism, such as articaine or propofol, are generally preferred. Additionally, the risk of bleeding should be assessed before any invasive procedures requiring anesthesia, and coagulation status should be evaluated to prevent complications.
Why is tooth extraction contraindicated in liver cirrhosis?
Tooth extraction is often contraindicated in patients with liver cirrhosis due to the increased risk of excessive bleeding and poor wound healing. Cirrhosis affects the liver’s ability to produce essential clotting factors, leading to a higher likelihood of prolonged or uncontrolled bleeding during extraction. Furthermore, compromised liver function can impair the body’s ability to fight infections, increasing the risk of post-extraction complications. In cases where extraction is necessary, preoperative evaluation of clotting status and consultation with a hepatologist may be required.
What precautions should be taken for liver disease?
Several precautions should be taken when treating dental patients with liver disease:
- Assess clotting function using tests such as INR, PT, and aPTT before invasive procedures.
- Modify medication dosages or select alternatives that are safer for patients with impaired liver function.
- Use local anesthetics with extrahepatic metabolism to avoid prolonged drug effects.
- Maintain strict infection control measures, as liver disease patients may have compromised immune function.
- Avoid medications that may further impair liver function, such as hepatotoxic antibiotics or NSAIDs.
Which antibiotic should be avoided in liver disease?
Certain antibiotics should be avoided in liver disease due to their potential hepatotoxicity or altered metabolism. Tetracyclines (such as doxycycline) and macrolides (such as erythromycin and clarithromycin) should generally be avoided, as they can cause liver damage or lead to drug accumulation in patients with hepatic impairment. Instead, antibiotics such as amoxicillin or clindamycin, which have a safer hepatic profile, may be preferred in these patients.
How can hepatitis affect dental treatment?
Hepatitis, an inflammatory condition of the liver caused by viral infections (Hepatitis A, B, C, D, or E), can impact dental treatment in several ways. Patients with hepatitis may have impaired liver function, leading to altered drug metabolism and increased bleeding risks. Additionally, there is a concern for cross-infection in the dental setting. Dental professionals should follow strict infection control protocols, including proper sterilization of instruments, wearing personal protective equipment (PPE), and ensuring proper vaccination for Hepatitis B. Pre-treatment liver function tests may be necessary for patients with chronic hepatitis.
What dental local anesthetic is safe for liver disease?
In patients with liver disease, local anesthetics that undergo extrahepatic metabolism are preferred. Articaine is often a safer choice than lidocaine because it is primarily metabolized by plasma esterases rather than the liver, reducing the risk of prolonged drug effects in patients with hepatic impairment. If lidocaine is used, the dosage should be carefully adjusted to prevent toxicity.
Which anesthesia drugs should be avoided in liver failure?
Several anesthesia drugs should be used cautiously or avoided in liver failure due to their hepatic metabolism and potential toxicity. These include:
- Halothane: Can cause hepatotoxicity and is generally avoided.
- Benzodiazepines (such as diazepam and midazolam): Their metabolism may be prolonged in liver disease, leading to prolonged sedation.
- Opioids (such as morphine and codeine): These drugs are metabolized in the liver and can accumulate, leading to excessive sedation and respiratory depression. Alternatives such as fentanyl, which undergoes extrahepatic metabolism, may be safer.
What should you not take if you have liver problems?
If you have liver disease, it is essential to avoid substances that can further impair liver function or cause toxicity. These include:
- Alcohol: Can exacerbate liver damage and lead to further deterioration of liver function.
- NSAIDs (such as ibuprofen, aspirin, and naproxen): Can increase the risk of gastrointestinal bleeding and worsen liver function.
- High doses of acetaminophen (Tylenol): Although it is commonly used as a pain reliever, excessive doses can cause severe liver damage.
- Certain antibiotics and antifungals: Drugs such as tetracyclines, erythromycin, and ketoconazole should be avoided due to hepatotoxic potential.
What is the best drink to flush your liver?
While no drink can “flush” the liver in a medical sense, certain beverages can support liver function and overall health. Water is the most important drink to keep the liver hydrated and functioning optimally. Green tea contains antioxidants that may help protect liver cells, while lemon water is sometimes recommended for its vitamin C content, which supports detoxification. However, these drinks should be viewed as part of a healthy lifestyle rather than a cure for liver disease.
How do you manage a patient with liver disease?
Managing a dental patient with liver disease requires a comprehensive approach, including:
- Evaluating liver function: Checking liver enzyme levels, clotting function, and overall hepatic status before any invasive procedures.
- Adjusting drug dosages: Using medications that are safer for hepatic impairment and avoiding those that require extensive liver metabolism.
- Minimizing bleeding risks: Assessing clotting factors and using local hemostatic agents or suturing techniques to control bleeding.
- Preventing infections: Maintaining strict hygiene protocols and considering prophylactic antibiotics in high-risk cases.
- Coordinating with the patient’s physician: Consulting with the hepatologist or primary care provider for guidance on medication management and overall patient care.
By following these guidelines, dental professionals can ensure safe and effective treatment for patients with liver disease while minimizing risks and complications.
Conclusion
Liver diseases present a complex set of challenges in the field of dentistry, requiring careful consideration of the patient’s overall health, liver function, and potential complications. Dentists must be vigilant in assessing the impact of liver diseases on dental treatment, including the risks of bleeding, altered drug metabolism, and increased susceptibility to infections.
A comprehensive approach to treatment planning, including thorough medical history taking, collaboration with other healthcare professionals, and patient education, is essential to providing safe and effective dental care for patients with liver diseases. By understanding the unique needs of these patients and taking appropriate precautions, dentists can help prevent complications and improve the overall quality of care.
In summary, the management of dental patients with liver disease requires a nuanced understanding of the disease’s impact on oral health and dental treatment. Through careful assessment, appropriate modifications to treatment, and ongoing communication with the patient and their medical team, dentists can ensure that these patients receive the best possible care while minimizing risks and complications.