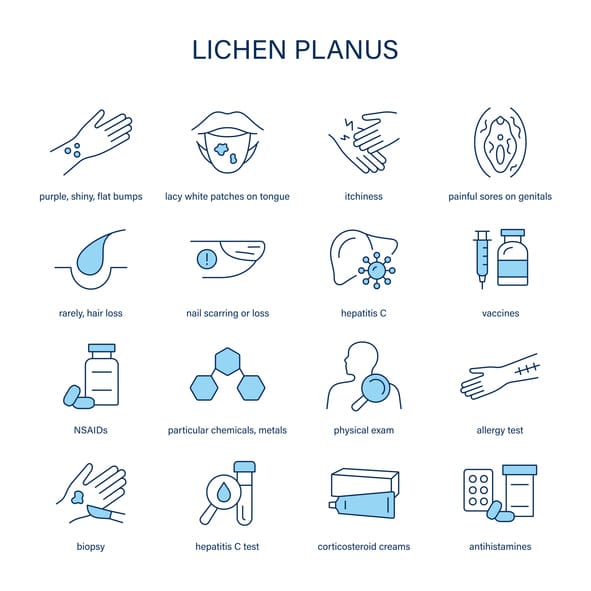
Lichen planus is a chronic inflammatory condition that affects the skin, mucous membranes, hair, and nails. It is characterized by purple, itchy, flat-topped papules on the skin and white, lacy patches or ulcers in the oral cavity and other mucosal surfaces. The exact cause of lichen planus remains unknown, but it is believed to involve an immune-mediated mechanism. Although the condition is not contagious or life-threatening, it can cause significant discomfort and affect the quality of life. This article explores the etiology, symptoms, diagnosis, treatment, and management of lichen planus in detail.
Table of Contents
ToggleEtiology and Pathogenesis
Lichen planus is considered an autoimmune condition in which the immune system mistakenly attacks keratinocytes, leading to inflammation and damage. The precise trigger is unknown, but several factors may contribute to its onset:
- Immune System Dysfunction
- Genetic Predisposition
- Triggers and Risk Factors
Immune System Dysfunction
T-cell-mediated immune responses play a crucial role in the pathogenesis of lichen planus. CD8+ cytotoxic T cells target basal keratinocytes, causing apoptosis and leading to the characteristic lesions. It is hypothesized that an unknown antigenic stimulus triggers this immune response, leading to persistent inflammation.
Genetic Predisposition
Genetic factors may play a role, as some cases show familial occurrence. However, no specific genetic mutation has been conclusively linked to the condition. Studies suggest that variations in immune response genes might contribute to susceptibility.
Triggers and Risk Factors
Several external and internal factors may trigger or exacerbate lichen planus:
- Medications: Certain drugs, such as nonsteroidal anti-inflammatory drugs (NSAIDs), beta-blockers, and angiotensin-converting enzyme (ACE) inhibitors, have been associated with lichenoid drug reactions.
- Infections: Hepatitis C virus (HCV) has been linked to oral lichen planus, especially in some geographical regions.
- Allergens and Chemicals: Dental materials like amalgam fillings and certain flavoring agents can trigger oral lichen planus.
- Stress and Trauma: Psychological stress and mechanical trauma (Koebner phenomenon) can exacerbate the condition. Emotional distress may contribute to immune dysregulation, leading to flare-ups.
- Hormonal Factors: Some studies suggest that hormonal changes, particularly in postmenopausal women, may influence the development of oral lichen planus.
Clinical Manifestations
Lichen planus can affect various body parts, and its presentation depends on the site of involvement. The disease can be classified into several variants based on its clinical features.
- Cutaneous Lichen Planus
- Oral Lichen Planus
- Genital and Esophageal Lichen Planus
- Nail and Scalp Involvement
Cutaneous Lichen Planus
The skin manifestations include:
- Papular Lesions: Small, polygonal, violaceous, flat-topped papules with fine white lines (Wickham’s striae).
- Distribution: Commonly seen on the flexor surfaces of the wrists, forearms, ankles, and lumbar region.
- Itching: Intense pruritus is a hallmark symptom, often leading to excoriation.
- Koebner Phenomenon: Lesions appear in areas of trauma.
- Hypertrophic Lichen Planus: Thickened, hyperpigmented plaques, usually on the shins. These plaques can be intensely pruritic and persist for years.
- Vesiculobullous Lichen Planus: Rarely, blistering lesions can develop, mimicking other bullous disorders.
Oral Lichen Planus
Affects the mucous membranes inside the mouth, presenting as:
- Reticular Form: White, lacy patches (Wickham’s striae) on the buccal mucosa, usually asymptomatic.
- Erosive Form: Painful, ulcerated lesions causing burning sensations, especially when consuming spicy or acidic foods.
- Atrophic Form: Red, inflamed patches, often misdiagnosed as other conditions like candidiasis.
- Plaque-like Form: Homogeneous white patches resembling leukoplakia.
- Gingival Lichen Planus: Characterized by desquamative gingivitis, leading to sore and bleeding gums.
Genital and Esophageal Lichen Planus
- Genital Involvement: White plaques, erosions, and scarring, leading to pain and discomfort, particularly in women. Severe cases may lead to vaginal stenosis.
- Esophageal Involvement: Strictures and difficulty in swallowing in severe cases, which may require dilation therapy.
Nail and Scalp Involvement
- Nail Changes: Longitudinal ridging, thinning, splitting, and nail loss. Severe cases may result in pterygium formation, where the nail matrix is permanently damaged.
- Scalp Involvement (Lichen Planopilaris): Permanent hair loss due to follicular destruction, often presenting with perifollicular erythema and scaling.
Diagnosis
Diagnosis is primarily clinical, based on the characteristic appearance of lesions. However, additional tests may be required for confirmation:
- Clinical Examination
- Histopathology
- Direct Immunofluorescence (DIF)
- Laboratory Tests
Clinical Examination
- Inspection of the skin, mucous membranes, nails, and scalp.
- Assessment of symptoms such as itching, pain, or burning sensations.
- Examination of Wickham’s striae under magnification.
Histopathology
A skin or mucosal biopsy shows:
- Hyperkeratosis, acanthosis, and basal layer degeneration.
- Band-like infiltrate of lymphocytes in the dermoepidermal junction.
- Civatte bodies (apoptotic keratinocytes), indicative of keratinocyte damage.
Direct Immunofluorescence (DIF)
DIF of biopsy specimens may show IgM, C3, or fibrin deposits along the basement membrane, confirming autoimmune involvement.
Laboratory Tests
- Hepatitis C screening (if suspected).
- Blood tests to rule out other autoimmune diseases.
- Patch testing to rule out contact allergens in oral cases.
Treatment and Management
There is no permanent cure for lichen planus, but treatment focuses on symptom relief and controlling inflammation.
- Topical Treatments
- Systemic Treatments
- Phototherapy
- Lifestyle and Home Remedies
Topical Treatments
- Corticosteroids: First line treatment for cutaneous and oral lesions, reducing inflammation.
- Calcineurin Inhibitors: Tacrolimus and pimecrolimus are used for oral and genital lesions when steroids are ineffective.
- Retinoids: Effective for hypertrophic lichen planus, reducing hyperkeratosis.
- Mouth Rinses: Corticosteroid or antifungal rinses for oral involvement.
Systemic Treatments
For severe cases:
- Oral Corticosteroids: Prednisone is used for short-term management.
- Immunosuppressants: Methotrexate, cyclosporine, or mycophenolate mofetil.
- Biologics: Emerging treatments targeting inflammatory pathways, such as TNF-alpha inhibitors.
Phototherapy
Narrowband UVB or PUVA therapy for widespread skin involvement, reducing inflammation.
Lifestyle and Home Remedies
- Avoiding Triggers: Discontinue medications that may cause lichenoid reactions.
- Oral Hygiene: Regular dental care and avoiding spicy foods.
- Stress Management: Meditation, yoga, and cognitive behavioral therapy.
Prognosis and Complications
Lichen planus is a chronic condition with periods of remission and flare-ups. Most cutaneous lesions resolve within 1-2 years, but oral and genital lichen planus may persist longer.
Complications
- Hyperpigmentation and Scarring: Common in hypertrophic and mucosal forms.
- Secondary Infections: Due to ulceration and irritation.
- Squamous Cell Carcinoma (SCC): Rarely, oral lichen planus may undergo malignant transformations.
Frequently Asked Questions (FAQs)
Is lichen planus contagious?
No, lichen planus is not contagious. It is an autoimmune condition and cannot be transmitted through contact with an affected person.
Can lichen planus go away on its own?
In some cases, lichen planus may resolve spontaneously within a few months to years. However, chronic cases, especially oral and genital lichen planus, may persist and require ongoing management.
What triggers lichen planus flare-ups?
Common triggers include stress, certain medications, infections (like Hepatitis C), and exposure to allergens or irritants.
Can lichen planus turn into cancer?
Oral lichen planus, particularly the erosive form, has a small risk of malignant transformation into squamous cell carcinoma. Regular monitoring and biopsy of suspicious lesions are recommended.
What foods should I avoid if I have oral lichen planus?
Spicy, acidic, and crunchy foods can exacerbate symptoms. It is best to follow a soft diet and avoid irritants such as alcohol and tobacco.
How is lichen planus diagnosed?
Diagnosis is based on clinical examination, biopsy, histopathology, and direct immunofluorescence studies to confirm the presence of characteristic immune deposits.
Can stress worsen lichen planus?
Yes, stress is a known trigger for lichen planus flare-ups. Stress management techniques like yoga, meditation, and therapy can help in symptom control.
What is the best treatment for lichen planus?
Treatment varies based on severity and site of involvement. Topical corticosteroids, calcineurin inhibitors, systemic immunosuppressants, and phototherapy are commonly used treatments.
Can children develop lichen planus?
Yes, although it is more common in adults, children can develop lichen planus, particularly oral and cutaneous forms.
Is there a cure for lichen planus?
Currently, there is no permanent cure, but treatments can effectively manage symptoms and improve quality of life.
Why does lichen planus occur?
The exact cause of lichen planus is unknown, but it is believed to be an autoimmune disorder where the immune system attacks skin or mucosal cells. It may be triggered by medications, infections, allergens, or stress.
How do you get rid of lichen planus?
There is no permanent cure for lichen planus, but treatments like topical and systemic corticosteroids, immunosuppressants, and phototherapy can help manage symptoms and reduce flare-ups.
Is lichen planus caused by stress?
While stress is not a direct cause of lichen planus, it can exacerbate symptoms and trigger flare-ups. Stress management techniques like meditation and therapy may help control the condition.
What foods should you avoid if you have lichen planus?
Spicy, acidic, and crunchy foods can irritate oral lichen planus. It is best to avoid citrus fruits, tomatoes, hot spices, alcohol, and tobacco to prevent symptom flare-ups.