Hemostasis, the process of stopping bleeding, is a crucial aspect of dental practice. Whether in routine extractions, periodontal surgeries, implant placements, or other invasive procedures, effective bleeding control ensures patient safety, enhances visibility during surgery, and reduces postoperative complications. Local hemostatic agents play a pivotal role in achieving hemostasis in dentistry, particularly when traditional methods such as direct pressure or sutures are insufficient.
This article explores the various local hemostatic agents used in dentistry, their mechanisms of action, indications, advantages, limitations, and emerging trends in the field.
Table of Contents
ToggleUnderstanding Hemostasis
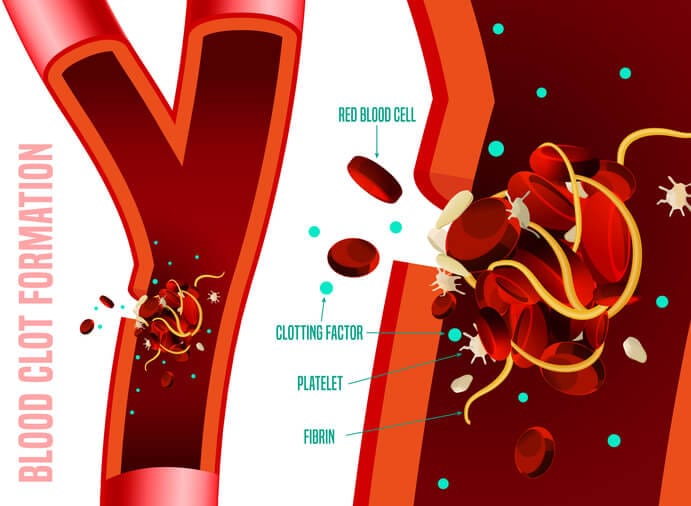
Hemostasis is the physiological process by which the body prevents and stops bleeding, or hemorrhage, after an injury. It involves a highly coordinated interplay between blood vessels, platelets, and coagulation factors. The process can be broadly divided into four key phases:
- Vascular Spasm
- Platelet Plug Formation
- Coagulation Cascade
- Clot Retraction and Remodeling
Vascular Spasm
When a blood vessel is injured, the first response is vasoconstriction, or the narrowing of the blood vessel, to reduce blood flow to the damaged area. This response is mediated by the contraction of smooth muscle in the vessel wall and is influenced by local signaling molecules such as endothelins. The vascular spasm provides time for the subsequent stages of hemostasis to take effect.
Platelet Plug Formation
Platelets, also known as thrombocytes, play a critical role in primary hemostasis. When a blood vessel is injured, platelets adhere to the exposed collagen fibers of the vessel wall via receptors such as glycoprotein Ib, which interacts with von Willebrand factor. Once adhered, platelets become activated, releasing granules containing ADP, thromboxane A2, and serotonin. These substances recruit additional platelets to the site and stimulate their aggregation, forming a temporary plug that seals small breaks in the vessel wall.
Coagulation Cascade
The coagulation cascade involves a series of enzymatic reactions that ultimately lead to the formation of a stable fibrin clot. This cascade has two initial pathways:
- Intrinsic Pathway: Activated by damage to the endothelium and exposure of collagen.
- Extrinsic Pathway: Triggered by tissue factor (TF) released from damaged tissues. Both pathways converge into a common pathway where prothrombin is converted into thrombin. Thrombin then converts fibrinogen into fibrin, which polymerizes to form a mesh-like structure that stabilizes the platelet plug.
Clot Retraction and Remodeling
Once the fibrin clot is formed, it undergoes retraction to bring the edges of the wound closer together, facilitating tissue repair. Over time, the clot is broken down through fibrinolysis, mediated by plasmin, as the vessel heals.
These stages of hemostasis are tightly regulated by a balance between pro-coagulant and anticoagulant factors to prevent excessive bleeding or pathological clotting.
Classification of Local Hemostatic Agents
Local hemostatic agents in dentistry can be broadly classified into the following categories:
- Mechanical Agents
- Absorbable Hemostats
- Biological Agents
- Chemical Agents
- Advanced Hemostatic Agents
Mechanical Agents
Mechanical agents physically obstruct bleeding by providing a matrix for clot formation. They are straightforward and often the first line of intervention for minor to moderate bleeding. Examples include:
Gauze and Cotton Pellets
These materials apply direct pressure and act as a scaffold for clot formation. Their simplicity makes them indispensable in dental practice, though they are primarily supportive rather than active agents.
Collagen-based Products
These include collagen sponges, plugs, or tapes derived from bovine or porcine sources. Collagen promotes platelet aggregation and activation, enhancing natural hemostasis. These products also assist in wound stabilization and healing.
Example: CollaPlug®, CollaTape®, CollaCote®.
Absorbable Hemostats
Absorbable agents dissolve over time and do not require removal. Their biocompatibility and ease of use make them highly effective in surgical contexts. Commonly used absorbable hemostats include:
Gelatin Sponges
Derived from porcine gelatin, these sponges provide a physical barrier and absorb blood. Upon contact with blood, they swell, exerting pressure on the bleeding vessel and accelerating clot formation.
Example: Gelfoam®, Surgifoam®.
Oxidized Regenerated Cellulose (ORC)
ORC materials are acidic, which helps denature blood proteins and promote clot formation. Additionally, they possess some antimicrobial properties, reducing the risk of infection at the surgical site.
Example: Surgicel®, Surgicel Fibrillar®.
Polysaccharide-based Agents
Derived from plant starch, these agents are biodegradable and facilitate hemostasis by absorbing fluid and concentrating clotting factors. They degrade quickly, minimizing any inflammatory response.
Example: Hemostatic Powder®.
Biological Agents
Biological hemostatic agents mimic or augment the body’s natural coagulation cascade and are particularly useful for patients with coagulopathies or in scenarios where standard measures fail.
Thrombin
A key enzyme in the coagulation pathway, thrombin converts fibrinogen to fibrin, accelerating clot formation. It is available in bovine, human recombinant, or synthetic forms and is often used in conjunction with other agents for enhanced effect.
Example: Thrombin-JMI®, Recothrom®.
Fibrin Sealants
These are composed of fibrinogen and thrombin and are applied directly to the site of bleeding. Fibrin sealants are particularly valuable in managing diffuse bleeding and enhancing wound closure.
Example: Tisseel®, Evicel®.
Chemical Agents
Chemical agents act by vasoconstriction or protein precipitation, forming a protective barrier over the bleeding site. These agents are especially useful for minor bleeding or in periodontal procedures.
Ferric Sulfate
Commonly used in periodontal and endodontic procedures, ferric sulfate promotes hemostasis through rapid protein denaturation and clot formation. However, it may cause temporary discoloration of the tissues.
Example: Astringedent®.
Aluminum Chloride
Primarily used in gingival retraction cords, aluminum chloride acts as a potent astringent, reducing capillary bleeding. It is gentle on tissues and widely accepted in routine procedures.
Example: Hemodent®.
Adrenaline/Epinephrine
Found in local anesthetics or applied topically, adrenaline induces vasoconstriction, effectively reducing blood flow and controlling bleeding. Its use requires caution in patients with cardiovascular conditions.
Advanced Hemostatic Agents
Recent advances have introduced novel agents with enhanced efficacy, biocompatibility, and additional functionalities like antimicrobial action. Examples include:
Chitosan-based Products
Chitosan, a polysaccharide derived from crustaceans, has inherent hemostatic and antimicrobial properties. It works by electrostatically interacting with red blood cells and platelets to form a gel-like clot.
Example: HemCon®, Celox®.
Microporous Polysaccharide Hemospheres (MPH)
These advanced agents absorb water from blood, concentrating clotting factors and platelets at the site, enhancing clot stability. They are biodegradable and leave no residue.
Example: Arista™.
Hydrogel Hemostats
These are emerging as an effective option for complex surgical sites, combining hemostatic action with wound protection and tissue hydration.
Applications in Dentistry
- Extraction Sites
- Periodontal Surgeries
- Implantology
- Endodontics
- Management of Patients with Coagulopathies
Extraction Sites
Post extraction bleeding is a common concern, especially in patients on anticoagulants or with bleeding disorders. Collagen sponges and gelatin sponges are widely used in these cases as they promote clot stability without requiring removal.
Periodontal Surgeries
In procedures such as gingivectomy, flap surgeries, or crown lengthening, agents like ferric sulfate and aluminum chloride are used to manage bleeding and improve visibility.
Implantology
Hemostatic agents are often required to control bleeding from bone or soft tissues during implant placement. Fibrin sealants and chitosan based products are particularly effective in this context.
Endodontics
In pulpotomy or apexification procedures, ferric sulfate is frequently employed to achieve hemostasis and maintain pulp vitality.
Management of Patients with Coagulopathies
For patients with hemophilia, von Willebrand disease, or those on anticoagulants, fibrin sealants and thrombin are preferred as they enhance clot formation without relying on the patient’s coagulation pathway.
Advantages and Limitations
Advantages
- Targeted Action: Local agents act specifically at the bleeding site, minimizing systemic effects.
- Ease of Use: Most agents are easy to apply and integrate seamlessly into dental procedures.
- Compatibility: Many agents are compatible with other dental materials, such as sutures or adhesives.
Limitations
- Cost: Advanced agents like fibrin sealants can be expensive.
- Foreign Body Reaction: Some materials may provoke an inflammatory response or delay healing.
- Limited Effectiveness: In cases of severe bleeding or coagulopathies, local agents alone may be insufficient.
Emerging Trends and Innovations
- Nanotechnology in Hemostasis
- Biodegradable Polymers
- Personalized Hemostatic Solutions
- Combination Products
Nanotechnology in Hemostasis
Nanoparticles with hemostatic properties are being developed to enhance clot stability and antimicrobial effects. For example, silver nanoparticles integrated into sponges or gels.
Biodegradable Polymers
Biodegradable hemostatic materials that release growth factors or antimicrobial agents are gaining attention for their dual functionality.
Personalized Hemostatic Solutions
Tailoring hemostatic agents based on a patient’s specific needs, such as coagulation profile or surgical site characteristics, represents the future of dental hemostasis.
Combination Products
Agents combining hemostatic, antimicrobial, and regenerative properties are being designed to optimize surgical outcomes.
Frequently Asked Questions (FAQs)
What is the best hemostatic agent for tooth extractions?
The choice depends on the patient’s bleeding risk and clinical scenario. Collagen sponges, gelatin sponges, and oxidized regenerated cellulose (ORC) are commonly used due to their ability to promote clot formation and stability.
Can hemostatic agents be used for patients on anticoagulants?
Yes, certain hemostatic agents such as fibrin sealants and thrombin-based products can be used in patients on anticoagulants. These agents enhance clot formation without interfering with systemic anticoagulation therapy.
Are there any side effects of using local hemostatic agents?
While most hemostatic agents are well tolerated, some may cause mild inflammation, foreign body reactions, or allergic responses. Additionally, agents like ferric sulfate may cause temporary tissue discoloration.
How long does it take for absorbable hemostatic agents to dissolve?
The dissolution time varies based on the agent used. Gelatin sponges may take 2-5 days, while oxidized regenerated cellulose may take up to 7-14 days to fully resorb.
Can chemical hemostatic agents be used on soft tissues?
Yes, chemical agents such as aluminum chloride and ferric sulfate are commonly used in soft tissue procedures, particularly in periodontal surgeries, to control capillary bleeding and improve visibility.
What precautions should be taken while using local hemostatic agents?
It is important to ensure that the hemostatic agent is biocompatible with the surgical site. Overuse or improper placement may lead to delayed healing or foreign body reactions. Additionally, thorough irrigation should be performed to remove any excess material that may interfere with wound healing.
What are the latest advancements in hemostatic agents?
Advancements include chitosan-based products, microporous polysaccharide hemospheres (MPH), and hydrogel-based hemostats, which provide enhanced clot stability, antimicrobial properties, and improved biocompatibility.
Conclusion
Local hemostatic agents are indispensable tools in modern dentistry, ensuring safe and efficient management of bleeding across a range of procedures. While traditional agents like collagen sponges and ferric sulfate remain widely used, advancements in biomaterials and technology are paving the way for more effective and versatile options. A thorough understanding of the properties, applications, and limitations of these agents allows dental practitioners to select the most appropriate hemostatic solution for each clinical scenario, ultimately improving patient outcomes and satisfaction.