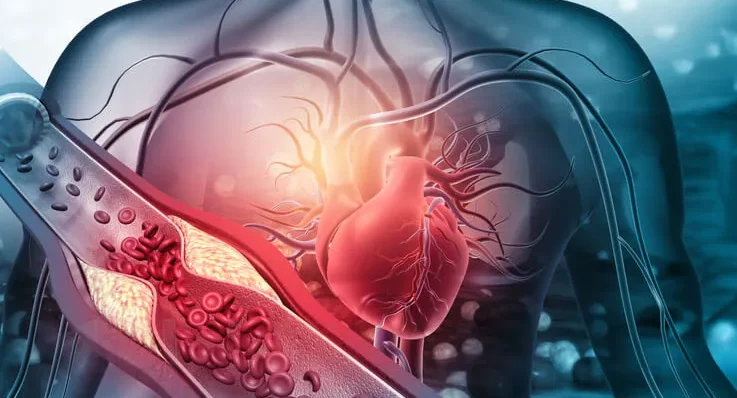
Atherosclerosis, a chronic inflammatory disease characterized by the buildup of plaques in arterial walls, is a leading cause of cardiovascular diseases, including heart attacks and strokes. While its direct impacts are well-studied in cardiology, a growing body of research suggests significant implications in other medical fields, including dentistry. This article delves into the intersection of atherosclerosis and dentistry, exploring the bidirectional relationship between oral health and cardiovascular health, the mechanisms linking the two, and the clinical implications for dental practice.
Table of Contents
ToggleThe Pathophysiology of Atherosclerosis
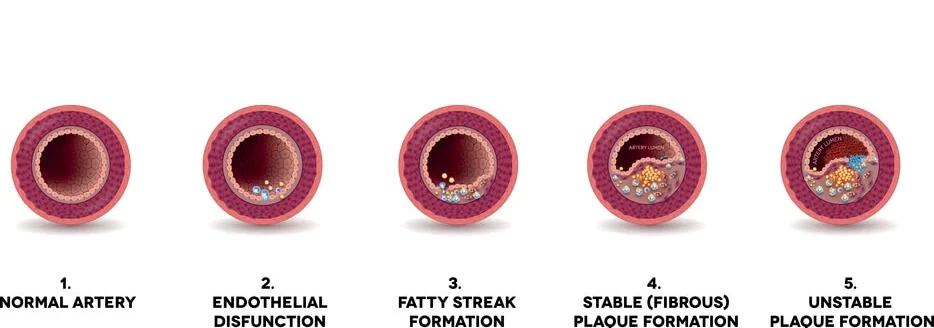
Atherosclerosis begins with endothelial dysfunction, where the inner lining of the arteries (endothelium) becomes damaged due to factors such as hypertension, hyperlipidemia, smoking, and diabetes. This damage leads to an inflammatory response, with immune cells infiltrating the arterial wall. Low-density lipoprotein (LDL) cholesterol accumulates and oxidizes within the intima layer of the artery, prompting further immune response and plaque formation. Over time, these plaques can harden and narrow the arteries, restricting blood flow and potentially leading to acute cardiovascular events if plaques rupture.
Oral Health and Systemic Inflammation
Oral health is increasingly recognized as a window to overall health, with periodontal disease (PD) emerging as a significant factor in systemic inflammation. Periodontal disease, a chronic inflammatory condition affecting the gums and supporting structures of the teeth, has been linked to various systemic conditions, including atherosclerosis.
Mechanisms Linking Periodontal Disease and Atherosclerosis
- Bacteremia and Endotoxemia
- Inflammatory Mediators
- Molecular Mimicry
Bacteremia and Endotoxemia
Periodontal pathogens, such as Porphyromonas gingivalis, can enter the bloodstream during routine activities like chewing or tooth brushing. These bacteria, along with their endotoxins, can contribute to systemic inflammation and endothelial dysfunction, both critical in the development of atherosclerosis.
Inflammatory Mediators
Periodontal disease is characterized by elevated levels of inflammatory cytokines, such as C-reactive protein (CRP), interleukins (IL-1, IL-6), and tumor necrosis factor-alpha (TNF-α). These mediators can exacerbate systemic inflammation and contribute to the inflammatory milieu within atherosclerotic plaques.
Molecular Mimicry
Some antigens from periodontal pathogens can mimic host tissues, potentially leading to an autoimmune response that accelerates the atherosclerotic process.
Evidence from Epidemiological Studies
Numerous epidemiological studies have identified a correlation between periodontal disease and cardiovascular diseases. Meta-analyses have shown that individuals with periodontitis have a higher risk of developing coronary artery disease and stroke. While these studies establish a correlation, they do not prove causation, highlighting the need for further research to elucidate the underlying mechanisms.
Clinical Implications for Dental Practice
Given the established link between periodontal disease and systemic inflammation, dental professionals play a crucial role in the early detection and management of conditions that could influence cardiovascular health.
- Comprehensive Periodontal Examination
- Patient Education
- Collaborative Care
- Periodontal Therapy and Cardiovascular Health
Comprehensive Periodontal Examination
Regular periodontal examinations should be an integral part of dental check-ups, especially for patients with known cardiovascular risk factors such as hypertension, diabetes, or a family history of heart disease. Early detection of periodontal disease allows for timely intervention, which could potentially mitigate systemic inflammatory burden.
Patient Education
Dental practitioners should educate patients about the importance of oral hygiene not only for preventing dental issues but also for its potential impact on overall health. Patients should be made aware of the link between periodontal health and systemic conditions, emphasizing the importance of regular dental visits and proper oral hygiene practices.
Collaborative Care
Interdisciplinary collaboration between dental and medical professionals is essential for holistic patient care. For patients with known cardiovascular conditions, communication between dentists and cardiologists can help in the formulation of comprehensive care plans that address both oral and cardiovascular health.
Periodontal Therapy and Cardiovascular Health
Evidence suggests that periodontal treatment can lead to improvements in markers of systemic inflammation and endothelial function. Scaling and root planing, the cornerstone of periodontal therapy, can reduce bacterial load and inflammation, potentially translating to a lower systemic inflammatory burden. Adjunctive therapies, such as systemic antibiotics and host modulation agents, may also play a role in managing the inflammatory component of periodontal disease.
Emerging Research and Future Directions
- Biomarkers and Diagnostic Tools
- Genetic Studies
- Novel Therapeutics
Biomarkers and Diagnostic Tools
Advancements in biomarker research could lead to the development of diagnostic tools that predict cardiovascular risk based on oral health status. Salivary diagnostics, for instance, are being explored for their potential to detect inflammatory markers and pathogenic bacteria associated with both periodontal disease and atherosclerosis.
Genetic Studies
Genetic predisposition plays a role in both periodontal disease and atherosclerosis. Future research exploring the genetic links between these conditions could lead to personalized treatment approaches, targeting individuals at higher risk for both diseases.
Novel Therapeutics
Innovative therapeutic strategies are being investigated to address the underlying inflammatory processes common to both periodontal disease and atherosclerosis. Anti-inflammatory agents, probiotics, and vaccines targeting periodontal pathogens are among the potential treatments that could have dual benefits for oral and cardiovascular health.
Frequently Asked Questions (FAQs)
What is the cause of arteriosclerosis?
Arteriosclerosis is caused by the thickening and hardening of the arterial walls, which reduces blood flow to vital organs. This condition develops over time due to aging, high blood pressure, high cholesterol, smoking, diabetes, and lifestyle factors such as a poor diet and lack of exercise. The buildup of fatty deposits, calcium, and other substances in the arteries can narrow and stiffen them, increasing the risk of cardiovascular complications.
Can you live a long life with arteriosclerosis?
Yes, it is possible to live a long and healthy life with arteriosclerosis if it is managed properly. Treatment includes adopting a heart-healthy diet, regular physical activity, quitting smoking, managing stress, and taking prescribed medications such as blood pressure or cholesterol-lowering drugs. Routine medical check-ups and monitoring are also crucial to preventing complications and slowing disease progression.
How serious is atherosclerosis?
Atherosclerosis is a potentially life-threatening condition as it can lead to severe cardiovascular diseases such as heart attacks, strokes, aneurysms, and peripheral artery disease. As plaque builds up in the arteries, it can restrict or completely block blood flow, leading to tissue damage and increasing the risk of fatal events. Early detection and treatment are essential to managing the disease and reducing the risk of severe complications.
What should you avoid if you have atherosclerosis?
If you have atherosclerosis, it is important to avoid foods high in saturated fats, trans fats, and cholesterol, such as fried foods, red meat, and processed foods. You should also reduce salt intake to help control blood pressure and avoid excessive sugar consumption to lower the risk of diabetes. Smoking and excessive alcohol intake can further damage the arteries and should be avoided. A sedentary lifestyle should also be replaced with regular physical activity to improve cardiovascular health.
What are 5 symptoms of atherosclerosis?
The symptoms of atherosclerosis vary depending on which arteries are affected. Five common symptoms include:
- Chest pain (angina): A sign of reduced blood flow to the heart, which may indicate coronary artery disease.
- Shortness of breath: Caused by restricted blood flow to the lungs and heart, leading to difficulty breathing, especially during physical activity.
- Fatigue: Insufficient blood supply to muscles and organs can cause a lack of energy and overall tiredness.
- Numbness or weakness in limbs: If arteries supplying the arms or legs are narrowed, it can result in pain, tingling, or weakness in the affected areas.
- High blood pressure: A result of the heart working harder to pump blood through stiffened or narrowed arteries.
What is the number one food to clean arteries?
Leafy green vegetables, such as spinach, kale, and Swiss chard, are considered among the best foods for keeping arteries clear. They are rich in antioxidants, fiber, and nitrates, which help improve blood flow, reduce inflammation, and lower blood pressure. Other beneficial foods include fatty fish, nuts, berries, and olive oil, which help lower cholesterol levels and support heart health.
What will dissolve plaque in arteries?
While no food or medication can completely dissolve plaque, lifestyle changes and medications can help reduce and stabilize it. A diet rich in healthy fats (such as omega-3 fatty acids), fiber, and antioxidants can help slow plaque buildup. Regular exercise improves circulation and heart function, while medications like statins can lower cholesterol and reduce plaque formation. In severe cases, medical procedures such as angioplasty or bypass surgery may be needed to restore proper blood flow.
What is the new drug that melts plaque in arteries?
Researchers are developing new medications to target arterial plaque more effectively. Currently, statins and PCSK9 inhibitors are the most widely used drugs for lowering cholesterol and stabilizing plaque in arteries. Additionally, some studies suggest that anti-inflammatory drugs, such as colchicine, may help reduce plaque-related complications. However, new treatments are still undergoing clinical trials to determine their effectiveness in reversing atherosclerosis.
What food causes calcium buildup in arteries?
Foods high in processed fats, excessive dairy products, and added sugars can contribute to calcium buildup in the arteries. Processed meats, fried foods, and foods high in trans fats can increase cholesterol levels, leading to plaque accumulation. Additionally, an imbalance of calcium intake, particularly from supplements rather than natural food sources, may contribute to arterial calcification. A balanced diet with adequate vitamin K2, magnesium, and omega-3 fatty acids can help regulate calcium metabolism and prevent excessive buildup in the arteries.
Conclusion
The relationship between atherosclerosis and dentistry underscores the importance of an interdisciplinary approach to healthcare. Periodontal disease, a prevalent condition managed by dental professionals, has significant implications for cardiovascular health through its contribution to systemic inflammation. By recognizing the interconnectedness of oral and systemic health, dental practitioners can play a pivotal role in the prevention and management of atherosclerosis and its complications. Continued research and collaboration between dental and medical fields are essential to fully understand and leverage this relationship for improved patient outcomes.