Alveolar ridge augmentation is a cornerstone procedure in modern implant dentistry and oral rehabilitation. It refers to the surgical techniques employed to increase the quantity and quality of alveolar bone in edentulous or partially edentulous patients. The alveolar ridge is a dynamic structure that undergoes continuous remodeling after tooth loss, trauma, periodontal disease, or congenital malformations. Such processes often result in insufficient bone volume or unfavorable ridge morphology, making dental implant placement challenging or, in many cases, impossible without augmentation.
The increasing demand for implant-supported restorations has stimulated significant advances in alveolar ridge augmentation techniques. These include autogenous bone grafting, guided bone regeneration (GBR), ridge splitting, distraction osteogenesis, and the use of biomaterials and growth factors. Each method has its own indications, advantages, and limitations, and successful treatment outcomes depend on careful case selection, surgical expertise, and proper prosthetic planning.
This article provides a detailed overview of alveolar ridge augmentation, including the biological basis, indications, surgical techniques, materials, complications, and future perspectives in regenerative dentistry.
Table of Contents
ToggleAnatomy and Biology of the Alveolar Ridge
The alveolar ridge is the bony structure that houses the teeth and provides support for the periodontal ligament and gingival tissues. Its integrity is vital for both function and aesthetics. When a tooth is lost, the alveolar bone undergoes resorption, primarily due to the absence of mechanical loading through the periodontal ligament. This resorption is most pronounced in the first six months following extraction, during which 30–60% of the ridge width can be lost.
Resorption patterns differ between the maxilla and mandible. The maxilla tends to resorb centripetally (towards the palate), whereas the mandible resorbs centrifugally (towards the tongue and floor of the mouth). These patterns often result in discrepancy in the arch form, complicating implant positioning and prosthetic alignment.
Bone biology plays a critical role in augmentation success. Autogenous bone grafts remain the gold standard due to their osteogenic, osteoinductive, and osteoconductive properties. However, advances in biomaterials and growth factors, such as recombinant human bone morphogenetic proteins (rhBMPs), have significantly expanded the regenerative potential of allogeneic and xenogeneic substitutes.
Indications for Alveolar Ridge Augmentation
The primary indication for alveolar ridge augmentation is inadequate bone volume that precludes ideal implant placement. Specific scenarios include:
- Post-extraction resorption – Severe horizontal and/or vertical loss of bone after tooth loss.
- Periodontal disease – Chronic infection leading to bone destruction.
- Trauma – Accidents or iatrogenic damage causing ridge deformity.
- Congenital defects – Conditions such as cleft lip and palate.
- Pathologic lesions – Tumors or cysts requiring surgical removal.
- Prosthetic requirements – Need for improved ridge contour to achieve optimal esthetics and function.
Ridge augmentation can be performed prior to implant placement (staged approach) or simultaneously with implant placement (simultaneous approach), depending on the residual bone volume and primary stability requirements.
Classification of Ridge Defects
Alveolar ridge defects are commonly classified according to Seibert’s classification:
- Class I: Buccolingual loss of ridge width with normal ridge height.
- Class II: Apicocoronal loss of ridge height with normal ridge width.
- Class III: Combination of both width and height loss.
This classification helps in choosing the appropriate augmentation technique, as horizontal deficiencies are usually more predictable to manage than vertical ones.
Techniques of Alveolar Ridge Augmentation
1. Autogenous Bone Grafting
Autogenous bone grafts are considered the gold standard due to their osteogenic capacity. They can be harvested intraorally (mandibular symphysis, ramus, tuberosity) or extraorally (iliac crest, calvarium, tibia).
- Block grafts: Corticocancellous blocks fixed to the deficient ridge with screws. Ideal for severe horizontal or vertical defects.
- Particulate grafts: Bone chips mixed with blood or platelet concentrates and packed into the defect.
Advantages: High biocompatibility, osteogenic potential.
Disadvantages: Donor site morbidity, limited volume in intraoral sites, increased surgical time.
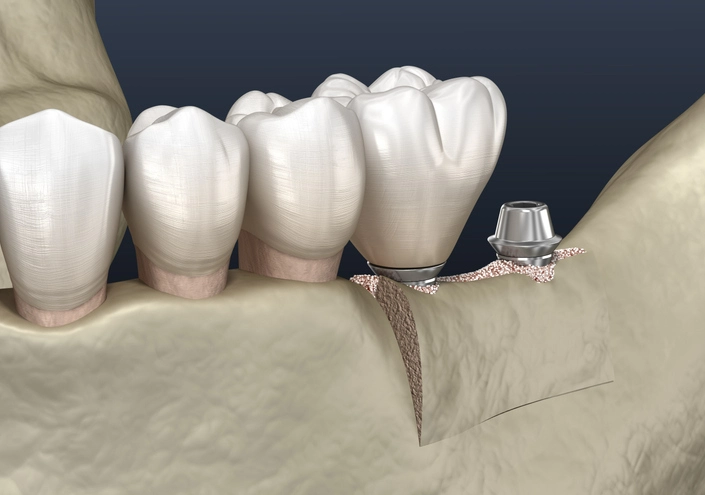
2. Guided Bone Regeneration (GBR)
GBR employs barrier membranes (resorbable or non-resorbable) to exclude soft tissue cells from the defect, thereby allowing bone regeneration. Often combined with particulate grafts.
- Resorbable membranes: Collagen-based, no need for removal.
- Non-resorbable membranes: ePTFE, require a second surgery for removal.
GBR is predictable for horizontal augmentation, but vertical augmentation remains challenging.
3. Ridge Splitting and Expansion
This technique involves splitting the narrow ridge and expanding it to create space for implant placement. Typically used in cases with at least 3 mm ridge width. Bone expanders or chisels are used, and implants may be placed simultaneously.
Read more about Ridge Splitting
Advantages: Avoids graft harvesting, single surgical site.
Limitations: Risk of fracture, not suitable for very atrophic ridges.
4. Distraction Osteogenesis
This technique involves gradual mechanical separation of a bone segment, inducing new bone formation in the gap. Used mainly for vertical augmentation.
Advantages: Can achieve substantial vertical height, maintains soft tissue volume.
Disadvantages: Technically demanding, requires patient compliance, risk of infection or device failure.
5. Use of Allogeneic, Xenogeneic, and Synthetic Grafts
- Allografts: Processed cadaveric bone, osteoconductive and sometimes osteoinductive.
- Xenografts: Derived from bovine or porcine sources, primarily osteoconductive.
- Synthetic grafts: Materials like hydroxyapatite, beta-tricalcium phosphate, bioactive glass.
These substitutes reduce donor site morbidity and are widely used in combination with autografts or growth factors.
6. Growth Factors and Biologics
- Platelet-rich plasma (PRP) and platelet-rich fibrin (PRF): Provide growth factors that accelerate healing.
- Bone morphogenetic proteins (BMPs): Strong osteoinductive potential, though costly.
- Enamel matrix derivatives and stem cell-based approaches: Emerging technologies with promising results.
Clinical Considerations
Case Selection and Planning
- Detailed clinical and radiographic evaluation (CBCT is standard).
- Prosthetically driven planning to ensure implant placement in optimal position.
- Evaluation of patient factors: systemic health, smoking, oral hygiene, compliance.
Surgical Protocol
- Atraumatic flap design with tension-free closure is essential.
- Meticulous handling of graft material and avoidance of contamination.
- Adequate fixation of grafts and membranes to prevent micromotion.
Healing and Timing
- Healing periods range from 4–9 months depending on the graft type and site.
- Staged approach is preferred in large or complex defects.
- Simultaneous implant placement possible in select cases with adequate stability.
Complications
- Infection: Can lead to graft loss, especially with membrane exposure.
- Membrane exposure: Reduces regenerative potential.
- Graft resorption: Particularly with particulate autografts.
- Donor site morbidity: Pain, paresthesia, esthetic concerns.
- Implant failure: If inadequate bone is regenerated.
Meticulous surgical technique and postoperative care are crucial to minimize complications.
Success Rates and Prognosis
Numerous studies have reported predictable outcomes with ridge augmentation, especially for horizontal augmentation. Vertical augmentation remains more challenging but is achievable with distraction osteogenesis and GBR. Long-term implant survival rates in augmented sites are comparable to those in native bone when protocols are followed correctly.
The esthetic outcome is equally important, particularly in the anterior maxilla. Soft tissue management, papilla preservation, and simultaneous connective tissue grafting may be required for optimal results.
Future Perspectives
The field of alveolar ridge augmentation continues to evolve. Promising directions include:
- Tissue engineering: Use of stem cells, scaffolds, and growth factors for predictable regeneration.
- 3D printing: Customized grafts and scaffolds tailored to defect morphology.
- Biomimetic materials: New generation biomaterials that mimic natural bone physiology.
- Minimally invasive techniques: Flapless and digital-guided approaches to reduce morbidity.
As regenerative medicine advances, the reliance on autogenous bone grafts may decrease, reducing patient discomfort and improving predictability.
Conclusion
Alveolar ridge augmentation is an indispensable procedure for successful implant therapy in cases of deficient bone volume. A wide array of techniques and materials are available, each suited for specific clinical scenarios. While autogenous bone grafting remains the gold standard, the integration of biomaterials, biologics, and digital technologies continues to refine outcomes.
Ultimately, careful diagnosis, individualized treatment planning, surgical precision, and long-term maintenance are the key determinants of success. With ongoing research and technological innovations, alveolar ridge augmentation is set to become more predictable, less invasive, and more widely accessible, thereby enhancing the quality of life for patients seeking implant-based rehabilitation.