Access cavity preparation is an integral step in root canal therapy that involves creating an opening through the crown of a tooth to gain entry into the pulp chamber and the root canal system. This initial phase is not merely about gaining entry, it establishes a pathway that allows for adequate cleaning, shaping, and disinfection of the complex internal anatomy of the tooth. An appropriately designed access cavity directly influences the success of subsequent endodontic procedures by ensuring that all pulp tissue, infected debris, and potential microbial contaminants are effectively removed.
A successful access cavity must accomplish several critical objectives. It must provide unobstructed visibility and straight-line access to canal orifices while preserving as much of the tooth’s natural structure as possible. The delicate balance between sufficient exposure for endodontic instrumentation and conservation of tooth structure has led to evolving philosophies in access cavity design. While traditional methods focused on creating large openings to ease canal location and instrumentation, modern techniques emphasize minimally invasive strategies that aim to preserve tooth strength and reduce the risk of fracture.
The significance of the access cavity extends beyond simply facilitating mechanical procedures; it is pivotal in establishing an environment where effective irrigation and disinfection protocols can be applied. Inadequate access can result in missed canals, insufficient debridement, and even instrument separation, which may compromise treatment outcomes. Furthermore, an optimal access cavity design minimizes the potential for procedural errors such as perforations and helps maintain the integrity of the tooth structure, thus contributing to the longevity of the restoration.
In this article, we explore the evolution of access cavity techniques, the anatomical and clinical principles guiding their design, and the various modern approaches that have emerged over time. Whether you are a seasoned practitioner or a student of endodontics, understanding these elements is essential for achieving consistent and favorable clinical results.
Table of Contents
ToggleHistorical Evolution of Access Cavity Design
The concept of accessing the root canal system has been a cornerstone of endodontic therapy since its inception. Early dental practitioners, with limited instrumentation and rudimentary understanding of tooth anatomy, approached access cavity preparation with a mindset focused on complete removal of pulp tissue by creating relatively large openings. These early techniques, while effective in removing diseased tissue, often resulted in substantial loss of tooth structure, rendering the tooth more susceptible to fracture post-treatment.
With advancements in dental technology and a deeper understanding of the biomechanics of the tooth, a paradigm shift occurred. The traditional “one-size-fits-all” approach gave way to more nuanced techniques that balanced the need for adequate canal visualization with the preservation of structural integrity. In the 1980s and 1990s, the integration of radiographic imaging and later the adoption of magnification tools such as dental operating microscopes allowed clinicians to better understand the complex internal morphology of teeth. This enhanced understanding paved the way for more conservative and targeted access designs.
Recent decades have seen a surge in research focusing on minimally invasive endodontics. Studies have demonstrated that preserving pericervical dentin—the critical area around the neck of the tooth—can significantly improve the tooth’s resistance to fracture. As a result, contemporary access cavity designs often incorporate contracted or “ninja” access cavities that limit unnecessary removal of healthy tissue. This evolution reflects a broader trend in dentistry toward procedures that are both biologically sound and mechanically resilient.
The historical evolution of access cavity preparation is marked by continuous improvement in clinical techniques, instrumentation, and technology. As our understanding of tooth anatomy and biomechanics continues to deepen, so too does our ability to refine these techniques, ultimately leading to better patient outcomes.
Anatomical Considerations and Rationale
Understanding tooth anatomy is fundamental to effective access cavity preparation. Each tooth exhibits a unique internal configuration that influences the approach a clinician must take. The pulp chamber, which houses the nerve and blood supply of the tooth, extends into a network of canals that vary in number, shape, and curvature. Recognizing these variations is essential for developing a tailored access strategy.
Pulp Chamber Anatomy
The pulp chamber is the central hub of the tooth’s internal anatomy. Its size, shape, and position can vary significantly among different types of teeth. For example, molars typically have larger pulp chambers with multiple canal orifices, whereas anterior teeth tend to have a single, more centralized pulp chamber. A thorough understanding of these differences allows clinicians to determine the appropriate location, dimensions, and orientation of the access cavity.
Canal Configuration and Complexity
The configuration of root canals further complicates the design of an access cavity. Teeth such as mandibular molars may have two or more canals that branch off from a single orifice, while maxillary molars often exhibit a complex network of three or four canals. Some canals may display significant curvature or even multiple apical terminations, making them challenging to negotiate without proper access. Clinicians must account for these variations when planning the shape and extent of the access cavity to avoid missing accessory canals or causing procedural errors.
Biomechanical Considerations
From a biomechanical perspective, the integrity of the remaining tooth structure after access preparation is crucial for the tooth’s long-term survival. The preservation of pericervical dentin, in particular, is vital as it plays a key role in distributing occlusal forces and maintaining structural integrity. An overly aggressive access cavity can weaken the tooth, increasing the risk of vertical root fracture or other complications. Thus, the rationale behind modern access cavity preparation lies in achieving a balance between sufficient canal access and the conservation of critical tooth structure.
Rationale for Access Cavity Preparation
The primary rationale behind access cavity preparation is to create a direct and unobstructed pathway to the root canal system. This enables the clinician to:
- Remove Infected Tissue: Effective debridement of necrotic or infected pulp tissue is critical in preventing the spread of infection and ensuring the success of root canal therapy.
- Facilitate Instrumentation: A well-designed access cavity allows for the introduction of endodontic files and rotary instruments, enabling precise shaping and cleaning of the canals.
- Optimize Irrigation: Adequate access ensures that irrigants can effectively reach all areas of the canal system, improving disinfection outcomes.
- Prevent Iatrogenic Damage: By providing straight-line access, the risk of instrument separation, ledging, and canal transportation is minimized.
- Preserve Tooth Structure: Modern designs emphasize conservation of tooth tissue to maintain the structural integrity and longevity of the tooth following treatment.
Design Principles of Access Cavity Preparation
The design of an access cavity is governed by several key principles aimed at optimizing clinical outcomes while minimizing the removal of healthy tooth structure. These principles include ensuring visibility, creating straight-line access, preserving pericervical dentin, and adapting to the specific anatomical variations of each tooth.
Ensuring Adequate Visibility
One of the foremost goals of access cavity preparation is to provide the clinician with unobstructed visibility of the pulp chamber and canal orifices. Adequate visibility is essential for:
- Identifying Canal Anatomy: Precise visualization of the internal anatomy helps locate all canal orifices, including accessory and lateral canals that may otherwise be missed.
- Preventing Procedural Errors: Clear visibility reduces the risk of perforations, ledging, or canal transportation that can occur when instruments are used blindly.
- Facilitating Instrumentation: Enhanced visibility enables more accurate placement and movement of endodontic instruments, ensuring thorough debridement and shaping.
Creating Straight-Line Access
Straight-line access refers to the alignment of the access cavity with the long axis of the canal. This alignment is critical for several reasons:
- Ease of Instrumentation: A direct path allows for the smooth passage of instruments, reducing the likelihood of instrument separation or binding within the canal.
- Reduced Canal Deviation: By minimizing curvature and obstructions, straight-line access helps prevent canal transportation and preserves the original anatomy.
- Improved Irrigation: A clear, unobstructed canal facilitates the effective delivery of irrigants, enhancing disinfection throughout the canal system.
Achieving straight-line access often requires the removal of obstructive dentin and careful adjustment of the cavity walls. The use of magnification and illumination, such as operating microscopes, has significantly improved clinicians’ ability to create and assess this access.
Preservation of Tooth Structure
While ensuring adequate access is critical, preserving as much of the tooth’s natural structure as possible remains a primary objective. The loss of pericervical dentin, in particular, can compromise the tooth’s resistance to fracture. Modern access cavity designs often employ a more conservative approach, minimizing unnecessary removal of healthy tissue. This trend towards minimally invasive endodontics is supported by evidence suggesting that a smaller access cavity can maintain or even improve the tooth’s long-term structural integrity.
Adapting to Tooth-Specific Anatomy
No two teeth are exactly alike, and the access cavity design must be tailored to the specific anatomical features of the tooth being treated. For instance:
- Anterior Teeth: Generally have a single canal and a relatively simple pulp chamber, allowing for a straightforward, centered access preparation.
- Premolars: May require a slightly modified approach due to variations in canal configuration, including the presence of multiple canals or bifurcations.
- Molars: Often present the greatest challenge due to their complex pulp chamber anatomy and multiple canals. In these cases, the access cavity must be designed to expose all canal orifices while still preserving as much coronal structure as possible.
By adapting the design to the unique anatomy of each tooth, clinicians can achieve both optimal canal access and the conservation of vital tooth structure.
Step-by-Step Clinical Procedure
The clinical procedure for access cavity preparation is a meticulous process that requires careful planning, precision, and adherence to established protocols. The following steps outline a comprehensive approach to access cavity preparation in endodontics.
1. Preoperative Assessment
Before beginning the procedure, a thorough assessment of the tooth is essential:
- Clinical Examination: Evaluate the tooth for signs of decay, previous restorations, or structural weaknesses.
- Radiographic Analysis: Use periapical or cone-beam computed tomography (CBCT) imaging to assess the internal anatomy, canal configuration, and the extent of any periapical pathology.
- Treatment Planning: Consider the patient’s overall dental health, occlusal forces, and the restorative plan post-treatment. This comprehensive evaluation helps in formulating an approach that maximizes the success of the access cavity preparation while safeguarding the tooth’s structural integrity.
2. Anesthesia and Isolation
Effective anesthesia and isolation are prerequisites for a successful endodontic procedure:
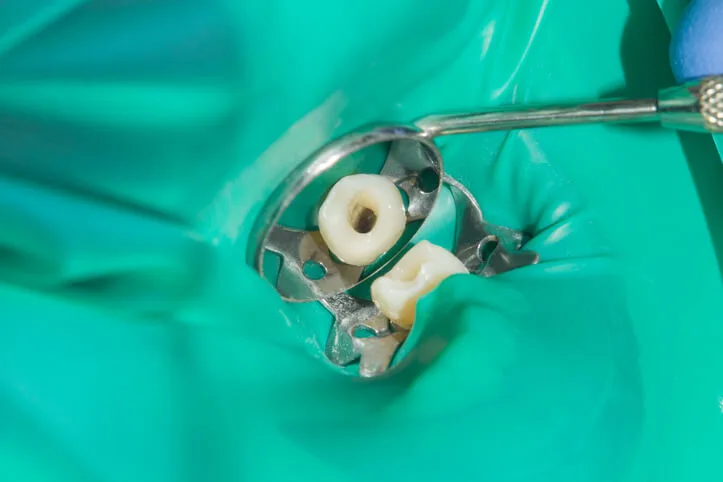
- Local Anesthesia: Administer appropriate local anesthesia to ensure patient comfort throughout the procedure.
- Rubber Dam Placement: Isolate the tooth using a rubber dam. This not only provides a clean working field free from saliva and contaminants but also enhances visibility and prevents accidental ingestion or aspiration of instruments and debris.
3. Initial Outline Form
Once the tooth is properly isolated, the next step is to create an outline form for the access cavity:
- Identify Landmarks: Using visual and tactile methods, locate the pulp chamber floor and identify key landmarks such as canal orifices.
- Marking the Outline: Gently mark the anticipated boundaries of the access cavity. This outline should be designed to allow for straight-line access to the canals while preserving as much of the pericervical dentin as possible.
4. Removal of Overlying Tooth Structure
Using high-speed burs, carefully remove the overlying enamel and dentin:
- Burs and Techniques: Begin with a tapered diamond or carbide bur to penetrate the occlusal surface or the incisal edge. The bur should be used with a light touch to gradually remove tooth structure and reveal the pulp chamber.
- Adjusting the Outline: As the cavity is prepared, continuously evaluate the outline form. Adjustments may be needed to ensure that all canal orifices are accessible and that the access cavity provides adequate visibility and straight-line access.
5. Refinement of the Access Cavity
Once the initial opening is made, the cavity is refined to ensure optimal access:
- Clearing the Pulp Chamber: Remove any remaining pulp tissue and debris using endodontic files and irrigation. This step is crucial to prevent blockage and to facilitate subsequent canal instrumentation.
- Identifying Canal Orifices: Under magnification, use endodontic explorers and small files to locate and confirm the position of all canal orifices. In molars and other multi-rooted teeth, this step may require additional modifications to the cavity walls.
- Smoothing and Shaping: Use finishing burs or ultrasonic tips to smooth the walls of the access cavity. This not only aids in the removal of any residual tissue but also helps in creating a clean, well-defined path to the canals.
6. Verification and Final Adjustments
After the access cavity has been refined, final verification is necessary:
- Radiographic Confirmation: Take a radiograph to confirm that the access cavity adequately exposes the root canal system without excessive removal of tooth structure.
- Final Inspection: Under magnification, perform a final inspection to ensure that the access cavity meets the objectives of clear visibility, straight-line access, and structural preservation.
- Irrigation and Temporary Sealing: Prior to canal instrumentation, irrigate the access cavity thoroughly to remove any debris. A temporary restorative material may be placed if there is a delay before proceeding to the next phase of treatment.
Modern Advances and Minimally Invasive Techniques
Recent advancements in technology and a growing emphasis on minimally invasive dentistry have significantly impacted the approach to access cavity preparation. Modern techniques aim to balance the need for adequate canal exposure with the imperative to conserve as much tooth structure as possible.
Contracted Access Cavities
The traditional approach to access cavity preparation often involved creating a relatively large opening, which, while facilitating easy access, compromised the structural integrity of the tooth. In response, clinicians have developed the concept of contracted or “ninja” access cavities. These minimally invasive designs:
- Preserve Pericervical Dentin: By limiting the extent of the access cavity, these techniques conserve the dentin around the cervical area, which is critical for resisting occlusal forces.
- Enhance Fracture Resistance: Studies have shown that teeth with contracted access cavities exhibit greater resistance to fracture compared to those with traditional, larger openings.
- Require Advanced Techniques: The success of contracted access cavities often relies on enhanced visualization through the use of dental microscopes, ultrasonics, and precise instrumentation, all of which facilitate accurate and conservative removal of tooth structure.
Use of Magnification and Illumination
The integration of magnification tools such as dental operating microscopes and endoscopes has revolutionized access cavity preparation:
- Improved Visualization: Enhanced magnification allows clinicians to clearly identify canal orifices and subtle anatomical features that may be missed with the naked eye.
- Precision in Instrumentation: With better illumination and magnification, the risk of procedural errors such as perforations is minimized. This precision is especially valuable when performing minimally invasive access procedures.
- Documentation and Training: Magnification also offers the advantage of recording procedures for documentation and educational purposes, thereby improving overall clinical practice.
Digital Imaging and CBCT
Digital imaging technologies, including cone-beam computed tomography (CBCT), have further refined access cavity preparation:
- Preoperative Planning: CBCT imaging provides a three-dimensional view of the tooth’s internal anatomy, allowing clinicians to plan the access cavity design with greater accuracy.
- Detection of Complex Anatomy: The detailed images obtained from CBCT scans help identify complex canal configurations, accessory canals, and anatomical variations that might influence the design of the access cavity.
- Risk Reduction: By using digital imaging to guide the access preparation, the likelihood of inadvertent damage to critical structures is significantly reduced.
Ultrasonic Instruments and Laser-Assisted Techniques
In recent years, ultrasonic instruments and laser-assisted technologies have been introduced to improve the precision and safety of access cavity preparation:
- Ultrasonics: Ultrasonic tips offer a controlled and conservative method for refining the access cavity. They are particularly useful for removing residual dentin and cleaning the cavity walls without causing excessive structural loss.
- Laser-Assisted Techniques: Lasers provide an additional modality for achieving precise removal of tooth structure. Their ability to ablate tissue with minimal thermal damage offers a promising adjunct to conventional rotary instrumentation.
Potential Complications and Troubleshooting
Despite advances in technology and technique, access cavity preparation is not without its challenges. Recognizing potential complications and implementing strategies to address them is essential for minimizing procedural errors and ensuring successful outcomes.
Iatrogenic Errors
Several iatrogenic errors can occur during access cavity preparation:
- Perforations: Overzealous removal of tooth structure can lead to perforations, which compromise the integrity of the tooth and may necessitate complex reparative procedures.
- Missed Canals: Inadequate access or failure to recognize anatomical variations can result in missed canals, which can harbor residual infection and lead to treatment failure.
- Instrument Separation: A poorly designed access cavity that does not provide straight-line access increases the risk of instrument separation. This complication can hinder complete debridement and complicate the treatment process.
Strategies for Troubleshooting
To mitigate the risk of complications, clinicians should adopt several key strategies:
- Enhanced Visualization: Utilizing magnification and proper illumination can greatly reduce the risk of iatrogenic damage. Clear visualization helps in accurately identifying canal orifices and anatomical landmarks.
- Preoperative Imaging: Comprehensive preoperative imaging, including CBCT scans when indicated, allows for better planning and anticipation of anatomical challenges.
- Incremental Preparation: Adopting an incremental approach to cavity preparation—regularly reassessing the progress and making minor adjustments—can prevent over-preparation and preserve tooth structure.
- Continued Education: Regular training and staying abreast of the latest research and technological advances are essential for refining technique and improving clinical outcomes.
Managing Complications
When complications do arise, timely and effective management is critical:
- Perforation Repair: If a perforation occurs, immediate repair using biocompatible materials such as mineral trioxide aggregate (MTA) can help seal the defect and prevent further complications.
- Retrieval of Separated Instruments: In cases of instrument separation, specialized retrieval techniques or referral to a specialist may be necessary to address the complication without compromising the treatment outcome.
- Secondary Access Modifications: If a canal is missed during the initial access preparation, secondary modifications to the access cavity can sometimes be performed to locate and treat the overlooked canal. This underscores the importance of thorough initial evaluation and cautious preparation.
Clinical Outcomes and Prognosis
The design and execution of the access cavity preparation have direct implications for the overall success of endodontic treatment. Numerous studies have demonstrated that a well-designed access cavity is associated with improved clinical outcomes, including enhanced disinfection, more efficient canal instrumentation, and reduced incidence of procedural complications.
Improved Disinfection and Shaping
A properly executed access cavity allows for effective irrigation and instrumentation:
- Enhanced Irrigation: With unobstructed access to the canal system, irrigants can penetrate more deeply, ensuring that bacteria and debris are effectively removed.
- Accurate Instrumentation: Straight-line access facilitates the use of rotary and hand files, leading to more precise shaping of the canal and better removal of necrotic tissue.
Preservation of Tooth Structure
The trend toward minimally invasive access designs has shown promising results:
- Increased Fracture Resistance: Conserving pericervical dentin and minimizing unnecessary removal of tooth structure directly contribute to the tooth’s ability to withstand functional stresses.
- Long-Term Survival: Studies comparing traditional and contracted access cavities have indicated that conservative designs may offer a superior prognosis by maintaining structural integrity, thereby reducing the risk of post-treatment fractures.
Evidence from Clinical Studies
The growing body of literature on access cavity preparation reinforces the importance of adhering to contemporary design principles:
- Success Rates: Clinical studies have correlated successful endodontic outcomes with the quality of the access cavity. Teeth treated with carefully planned and executed access openings exhibit lower rates of reinfection and retreatment.
- Patient-Centered Outcomes: Beyond technical success, a well-executed access cavity contributes to improved patient outcomes by reducing treatment time, minimizing discomfort, and enhancing overall satisfaction with endodontic therapy.
Frequently Asked Questions
What is an access cavity?
An access cavity is the opening prepared in the crown of a tooth during endodontic treatment. It provides the entry point into the pulp chamber and root canal system. This opening allows the clinician to remove infected or necrotic tissue, access all canal orifices, and properly shape and disinfect the canals as part of a successful root canal therapy.
What is the access cavity in a tooth?
The access cavity in a tooth refers to the entry point created on the occlusal (biting) or incisal (cutting) surface through which the pulp chamber is reached. It is strategically designed to expose the internal canal system, ensuring that instruments and irrigants can reach every part of the canal network while conserving as much of the surrounding healthy tooth structure as possible.
How to open an access cavity?
Opening an access cavity involves several critical steps:
- Preoperative Assessment: Evaluate the tooth using clinical and radiographic examinations (including CBCT if necessary) to understand the tooth’s internal anatomy.
- Isolation and Anesthesia: Administer local anesthesia and isolate the tooth with a rubber dam to provide a clean, dry field.
- Outline Form Preparation: Identify key anatomical landmarks on the pulp chamber floor and mark the intended boundaries of the access cavity.
- Removal of Tooth Structure: Use high-speed diamond or carbide burs to carefully remove enamel and dentin. This is done gradually, with intermittent checks under magnification.
- Refinement: Once the pulp chamber is reached, clear out residual pulp tissue and refine the cavity walls to expose all canal orifices.
- Verification: Use radiographs and magnification to confirm that the access cavity offers straight-line entry to the canals, ensuring efficient cleaning and instrumentation.
What is the hardest tooth to get a root canal on?
The difficulty of performing a root canal varies with each patient’s unique anatomy. However, many endodontists consider the maxillary second molar to be among the most challenging due to its variable canal morphology, unpredictable anatomy, and sometimes limited access because of its posterior location. Additionally, certain mandibular molars—with severe curvature or calcification—can also present significant challenges during endodontic treatment.