The preservation of pulp vitality is one of the most important goals in restorative dentistry and endodontics. While traditional endodontic therapy has focused on treating diseases of the pulp by removing necrotic or irreversibly inflamed tissue, modern dentistry places significant emphasis on maintaining the natural biology of the tooth whenever possible. Understanding how to preserve pulp vitality is essential not only for preventing more invasive treatments, but also for ensuring long-term function, structural integrity, and sensory capacity of the dentition.
The pulp–dentine complex is a living tissue with remarkable capacity for defense and repair. When dental tissues are exposed to caries, trauma, or restorative procedures, the pulp responds through inflammation and, when conditions allow, can undergo healing with deposition of tertiary dentine. The ability to maintain a healthy, functioning pulp is key to long-term tooth survival.
Table of Contents
ToggleUnderstanding the Importance of a Healthy Pulp
The dental pulp is a highly specialized soft tissue enclosed within the rigid structure of dentine. It plays several essential roles throughout the life of the tooth:
1. Completion of root formation (Primary dentine formation)
In immature permanent teeth, a vital pulp is necessary for continued root development, apexogenesis, and thickening of dentinal walls. Loss of vitality during this stage can compromise prognosis and complicate treatment.
2. Lifelong dentine deposition (Secondary dentine formation)
Even after root formation is complete, the pulp continues to lay down secondary dentine. This contributes to:
- reinforcement of tooth structure
- reduction of pulp chamber size with age
- long-term resilience against fractures
3. Defensive and reparative capacity
When enamel or dentine integrity is compromised due to caries, trauma, or wear, the pulp responds by forming reactionary or reparative tertiary dentine. This natural barrier helps protect the pulp from microbial invasion and thermal or mechanical insults.
4. Sensory and nociceptive function
The pulp houses nerve fibers responsible for transmitting pain, temperature, and pressure sensations. These sensory mechanisms act as protective warnings against harmful stimuli.
5. Maintenance of dentine elasticity
Vital pulp contributes to the hydration and resilience of dentine, allowing it to flex under functional loads. Loss of pulp vitality leads to a more brittle tooth structure, increasing fracture risk.
Given these crucial roles, maintaining pulp health should be a primary goal whenever clinically feasible.
Pulpal Infection and Its Consequences
When the pulp is exposed to bacterial invasion—most commonly from caries—it initiates an inflammatory response. Initially, this can be reversible, but without intervention, inflammation becomes progressively severe and may culminate in irreversible pulpitis.
If irreversible pulpitis is left untreated, pulp necrosis and periapical periodontitis ensue. At this stage, root canal treatment (RCT) becomes necessary to eliminate infection and preserve the tooth.
The primary aim of endodontic therapy has historically been to treat or prevent periapical disease. However, the modern scope of endodontics extends further, encompassing preventive and minimally invasive therapies that aim to retain the vitality of the pulp whenever conditions permit.
Pulp-Preserving Therapies
Pulp-preserving procedures include:
- Biological caries removal
- Indirect pulp protection (indirect pulp capping)
- Direct pulp protection (direct pulp capping)
- Pulpotomy (partial or full coronal pulp removal)
These procedures leverage the biological capacity of the pulp to heal when suitably protected from bacterial insult.
Biological Basis and Evolving Clinical Philosophy
Advances in adhesive dentistry and biomaterials have transformed the approach to cavity preparation. We now recognize that:
- Not all softened dentine needs to be removed.
- Over-instrumentation risks unnecessary pulp exposure.
- A well-sealed restoration is more important than absolute caries removal.
The Pulp–Dentine Complex as a Dynamic Tissue
The concept of the pulp–dentine complex emphasizes that:
- Pulp and dentine are interdependent.
- Dentine contains tubules that communicate with pulp tissue.
- The pulp can respond biologically with inflammation, healing, and dentinogenesis.
When caries-infected dentine is removed, caries-affected dentine may remain if it is free of active infection and can be sealed beneath a restoration. This approach reduces pulpal stress and encourages natural healing.
Indirect Pulp Protection (Indirect Pulp Capping)
Indirect pulp protection is indicated when caries is deep but the pulp is not exposed and remains vital. In such cases, a thin layer of softened but disinfected dentine may be left behind to avoid pulp exposure.
Mechanism
Once the lesion is sealed:
- Bacterial activity decreases dramatically due to lack of substrate.
- The pulp–dentine complex deposits tertiary dentine at the pulp interface.
- Gradual remineralization of affected dentine can occur.
Materials Used
Common materials include:
- Biodentine™ (bioactive dentine substitute)
- Calcium hydroxide
- Resin-modified calcium silicate materials such as TheraCal LC™
These materials:
- stimulate dentine bridge formation
- provide antibacterial effects
- form a protective barrier beneath the definitive restoration
Indirect pulp capping has shown high success rates when proper case selection and sealing are achieved.
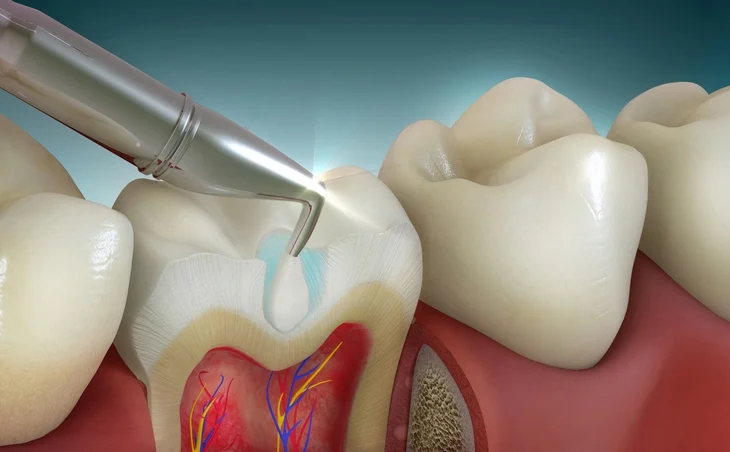
Direct Pulp Protection (Direct Pulp Capping)
Direct pulp capping is performed when the pulp is exposed, either accidentally during cavity preparation or through shallow caries. For this procedure to succeed, the pulp must be healthy or show only reversible inflammation.
Biological Requirements for Success
- No signs or symptoms of irreversible pulpitis
- Controlled bleeding at the exposure site
- A sterile field (rubber dam isolation is mandatory)
- A competent coronal seal
Materials Used
The gold-standard materials for direct pulp capping today are:
- Calcium silicate cements (e.g., ProRoot® MTA, Biodentine™)
These materials: - are highly biocompatible
- stimulate odontoblastic differentiation and dentine bridge formation
- provide superior sealing ability compared to calcium hydroxide
Calcium hydroxide, historically the mainstay, is now less commonly used due to tunnel defects in dentine bridges and inferior long-term performance.
Pulpotomy: A Vital Pulp Therapy for Reversible Inflammation
A pulpotomy involves removing the inflamed coronal pulp while preserving the healthy radicular pulp within the root canal system. This therapy is well-established in pediatric dentistry but is increasingly explored in adult teeth as well.
Indications
- Symptomatic or asymptomatic reversible pulpitis affecting the coronal pulp
- Exposure due to caries or trauma
- Immature teeth requiring continued root development
Procedure and Biological Rationale
Once the inflamed pulp tissue is removed:
- Hemostasis must be achieved
- A biologically active material (e.g., MTA, Biodentine™) is placed
- The radicular pulp is left intact to continue its protective and sensory functions
The success of pulpotomy depends heavily on:
- correct diagnosis
- complete removal of diseased tissue
- adequate sealing restoration
Recent studies have shown high success rates of full pulpotomy in adult permanent teeth, positioning it as a less invasive alternative to root canal treatment in selected cases.
Prerequisites for All Pulp-Preserving Therapies
To consider any pulp-preserving approach, the clinician must ensure:
- No symptoms of irreversible pulpitis (e.g., lingering thermal pain)
- A positive response to pulp vitality testing
- No radiographic signs of periapical pathology
- Good periodontal support
- Ability to isolate the tooth with a rubber dam
- Restoration with an excellent seal
Case selection is the single most important determinant of success.
Follow-Up and Monitoring
Vital pulp therapy requires ongoing assessment to confirm continued pulpal health. Follow-up should occur within 6–12 months, including:
- Sensibility testing
- Clinical evaluation for symptoms
- Radiographs to evaluate root development and periapical status
If at any point the pulp becomes irreversibly inflamed or necrotic, conventional RCT is indicated.
At present, evidence is still developing regarding the use of pulpotomy as a definitive treatment in adult permanent teeth. While promising, more long-term research is required.
The Future of Vital Pulp Therapy: Regenerative Endodontics
A rapidly evolving area in dental research is the regeneration of pulp tissue through:
1. Stem cell therapy
Stem cells derived from the apical papilla or dental pulp can potentially regenerate pulp-like tissues capable of dentinogenesis.
2. Tissue engineering
Combines scaffolds, signaling molecules, and stem cells to recreate functional tissue.
3. Revascularization
Used primarily in immature necrotic teeth, where bleeding is induced to introduce mesenchymal stem cells into the canal space, facilitating root development and tissue regeneration.
These biologically driven therapies are collectively termed regenerative endodontic procedures (REPs). They hold the promise of restoring true biological function rather than merely replacing tissue with inert filling materials.
Conclusion
Preserving pulp vitality is at the heart of modern minimally invasive dentistry. The dental pulp plays critical roles in tooth development, defense, sensation, and structural resilience. When disease or trauma threatens the pulp, clinicians now have a spectrum of vital pulp therapies—ranging from indirect and direct pulp capping to pulpotomy—that can maintain pulp function and delay or avoid more invasive procedures such as root canal therapy.
Successful vital pulp therapy hinges on:
- accurate diagnosis
- understanding pulp biology
- meticulous technique
- effective isolation and restoration
- appropriate follow-up
As materials science and biological understanding advance, regenerative endodontics promises a future in which damaged pulps can be restored rather than replaced. This shift represents a profound transformation in dental philosophy—one that prioritizes preservation of natural tissues and harnesses the body’s own healing potential.
References
- American Association of Endodontists (AAE). Guide to Clinical Endodontics. 6th ed. Chicago: AAE; 2013.
- Aguilar P, Linsuwanont P. Vital pulp therapy in vital permanent teeth with cariously exposed pulp: A systematic review. J Endod. 2011;37(5):581–587.
- Bogen G, Kim JS, Bakland LK. Direct pulp capping with mineral trioxide aggregate: An observational study. J Am Dent Assoc. 2008;139(3):305–315.
- Cox CF, Subay RK, Ostro E, Suzuki S, Suzuki SH. Tunnel defects in dentin bridges: Their formation following direct pulp capping. Oper Dent. 1996;21(1):4–11.
- Duncan HF, Galler KM, Tomson PL, et al. European Society of Endodontology position statement: Management of deep caries and the exposed pulp. Int Endod J. 2019;52(7):923–934.
- Galler KM. Clinical procedures for revitalization: Current knowledge and considerations. Int Endod J. 2016;49(10):926–936.
- Heithersay GS. Emergency pulpotomy in mature teeth. Aust Dent J. 1975;20(1):1–9.
- Hilton TJ. Keys to clinical success with pulp capping: A review of the literature. Oper Dent. 2009;34(5):615–625.
- Murray PE, Hafez AA, Smith AJ, Cox CF. Biological bases for endodontic therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(6):751–766.
- Nekoofar MH, Oloomi K, Sheykhrezae MS, et al. Comparison of the effect of calcium hydroxide and mineral trioxide aggregate on inflammatory cells in direct pulp capping. J Endod. 2008;34(7):818–821.
- Nowicka A, Lipski M, Parafiniuk M, et al. Response of human dental pulp capped with biodentine and mineral trioxide aggregate. J Endod. 2013;39(6):743–747.
- Ricucci D, Siqueira JF Jr. Biofilms and apical periodontitis: Study of prevalence and association with clinical and histopathologic findings. J Endod. 2010;36(8):1277–1288.
- Witherspoon DE. Vital pulp therapy with new materials: New directions and treatment perspectives—permanent teeth. J Endod. 2008;34(7 Suppl):S25–S28.
- Yasuda Y, Ogawa M, Arakawa T, et al. Pulpal responses after direct pulp capping with calcium-silicate cement in rats. Med Oral Patol Oral Cir Bucal. 2017;22(5):e555–e562.
- Zhang W, Yelick PC. Vital pulp therapy—current progress of dental pulp regeneration and revascularization. Int J Dent. 2010;2010:856087.