In the ever-evolving landscape of modern dentistry, tooth loss remains a major clinical concern, affecting millions of people worldwide. Whether due to trauma, decay, or periodontal disease, missing teeth can significantly impair both oral function and aesthetics. For decades, the primary solutions for replacing missing teeth have included dentures, bridges, and dental implants. However, an increasingly researched and practiced alternative—tooth transplant, also known as autotransplantation—has garnered attention for its potential benefits, particularly in young patients and select clinical scenarios.
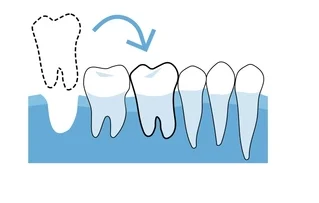
Tooth transplant refers to the surgical movement of a tooth from one site to another within the same individual. This technique harnesses the body’s natural healing mechanisms, and when performed under appropriate conditions, it can restore function, preserve alveolar bone, and maintain proprioception something dental implants cannot offer. Despite its limited mainstream awareness, tooth transplantation has a long history, with roots stretching back centuries. Today, advances in imaging, surgical techniques, and tissue regeneration have renewed interest in this innovative solution.
This article delves into the principles, procedures, indications, contraindications, advantages, disadvantages, and current research surrounding tooth transplants, providing a thorough overview of this promising dental technique.
Table of Contents
ToggleHistory and Evolution
Tooth transplantation is not a novel idea. The earliest recorded attempts date back to ancient Egypt and have been described in texts from the Middle Ages. In the 18th century, Pierre Fauchard, often considered the father of modern dentistry, documented procedures involving tooth replacement using donor teeth. However, these early efforts were fraught with issues, primarily due to a lack of understanding of sterile techniques and immune responses.
It wasn’t until the 20th century that autotransplantation—moving a tooth within the same individual—gained scientific traction. This method eliminates the immunological risks of donor rejection, as the transplanted tooth is genetically compatible. Over time, clinicians began to refine their techniques, improving success rates and expanding the range of indications.
Types of Tooth Transplantation
Tooth transplantation generally falls into three categories:
- Autogenous (Autotransplantation): Transferring a tooth from one site to another within the same person. This is the most common and successful form.
- Allogenic: Transplantation of a tooth from one individual to another. Rarely practiced due to high risk of immune rejection.
- Xenogenic: Use of teeth from a different species. This is mostly experimental and not practiced clinically.
Of these, autotransplantation is considered the most clinically viable and ethically acceptable method.
Indications for Tooth Transplantation
Tooth transplants can be considered in a variety of clinical scenarios:
1. Congenital Absence
In conditions like hypodontia, where one or more teeth are congenitally missing (commonly lateral incisors or premolars), a suitable donor tooth such as a premolar can be used to fill the gap.
2. Traumatic Tooth Loss
In cases of accidental avulsion, especially in younger patients, replacing the missing tooth with a developing premolar from another site can be a viable option.
3. Tooth with Poor Prognosis
If a molar has an end-stage periodontal disease or large carious lesion, and another tooth (such as a third molar) is healthy and impacted, the latter can be transplanted.
4. Ectopic or Impacted Teeth
Teeth that have erupted in undesirable positions or are severely impacted may be extracted and repositioned via transplantation.
5. Orthodontic Indications
Sometimes, a donor tooth may be transplanted to eliminate the need for prosthetics during or after orthodontic treatment.
Contraindications
While promising, tooth transplantation isn’t suitable for everyone. Contraindications include:
- Poor systemic health or immunocompromised status
- Active periodontal disease
- Uncontrolled diabetes
- Inadequate alveolar bone volume at the recipient site
- Donor tooth with incomplete root development beyond optimal stages
- High risk of non-compliance with post-operative care
Procedure: Step-by-Step
1. Preoperative Planning
Comprehensive clinical and radiographic evaluation is crucial. This includes:
- Clinical examination of both donor and recipient sites
- Periapical radiographs and CBCT scans to evaluate root anatomy and surrounding bone
- Assessment of root development stage in donor tooth (ideally ¾ root formation with open apex)
- Digital modeling or 3D printing may be used to simulate the procedure beforehand
2. Selection of Donor Tooth
Typically, premolars and third molars are the most common donor teeth due to their anatomical features and dispensability. The ideal donor tooth should have:
- Incomplete root development (preferably ¾ to ⅘ complete)
- No anomalies or root curvature
- Minimal trauma risk during extraction
3. Recipient Site Preparation
The recipient site must be prepared carefully to accommodate the donor tooth with minimal trauma. This may involve socket creation or modification.
4. Tooth Extraction and Transplantation
- The donor tooth is carefully extracted with minimal damage to the periodontal ligament (PDL).
- Extraoral time should be minimized (ideally <15 minutes).
- The tooth is inserted into the prepared socket and adjusted for occlusion.
- It may be stabilized using sutures or splints.
5. Postoperative Care
- Antibiotics and chlorhexidine mouthwash may be prescribed.
- A soft diet is recommended for several weeks.
- Splint removal is usually done within 2–4 weeks.
- Root canal treatment may be necessary, particularly for teeth with completed root formation.
Success Rates and Prognosis
The reported success rate for autotransplanted teeth ranges from 80% to 95%, particularly when performed under ideal conditions. Several factors influence the outcome:
Positive Predictors
- Young age (especially children and adolescents)
- Open apex in donor tooth (promotes revascularization)
- Minimally traumatic extraction
- Short extraoral time
- Proper splinting and post-op care
Complications
- Root resorption (inflammatory or replacement)
- Ankylosis (fusion with bone)
- Pulpal necrosis
- Infection
- Failure to integrate or loosening
Proper case selection and technique are vital to avoiding these complications.
Advantages of Tooth Transplantation
Tooth autotransplantation offers several unique benefits over implants or dentures:
1. Natural Proprioception
The transplanted tooth retains its periodontal ligament, enabling proprioceptive feedback, which is lost in implants.
2. Alveolar Bone Preservation
Presence of the PDL supports normal bone remodeling and prevents resorption.
3. Growth Compatibility
In growing children, implants are contraindicated. Transplanted teeth can continue to erupt and adapt to growth.
4. Biological Integration
Unlike prosthetics, a successful transplant becomes a living, functional part of the mouth.
5. Cost-Effective
Compared to implants and bridges, transplantation can be less expensive in many cases.
Limitations and Challenges
Despite its promise, tooth transplantation is not without challenges:
- It demands high surgical skill and experience.
- Donor teeth must be available and suitable.
- Not all patients are ideal candidates.
- Post-operative care is critical and patient compliance is essential.
- Public and even professional awareness remains limited.
Case Studies and Clinical Examples
Case 1: Premolar Transplant in a Hypodontia Patient
A 14-year-old female missing a lateral incisor underwent autotransplantation using her lower premolar. The tooth successfully integrated and remained functional and esthetic five years post-op.
Case 2: Third Molar to First Molar Replacement
A 20-year-old male had a non-restorable first molar. His unerupted third molar was transplanted into the site. With proper endodontic therapy and occlusal adjustment, the tooth served as a successful molar replacement.
Ethical and Legal Considerations
Autotransplantation raises fewer ethical concerns compared to allogenic transplants. However, informed consent is critical. Patients (or guardians) must be made fully aware of:
- Risks and benefits
- Possible complications
- Alternative treatments
- Long-term expectations
Documentation and follow-up are essential for medicolegal protection.
Conclusion
Tooth transplantation, particularly autotransplantation, represents a unique blend of surgical precision and biological integration. While not a panacea for all tooth loss cases, it offers remarkable benefits in the right clinical context—especially in growing patients and when appropriate donor teeth are available.
As dentistry continues to push the boundaries of biomimetic and regenerative solutions, tooth transplantation is poised to become more mainstream. With further research, increased clinician training, and public awareness, this age-old technique may find renewed prominence in 21st-century dental care.