Stomatitis is a term that broadly refers to inflammation within the oral cavity, affecting the mucous membranes of the mouth. It can present in various forms, ranging from mild irritation to severe ulceration, causing significant discomfort and pain. Stomatitis can be caused by numerous factors, including infections, allergies, autoimmune conditions, and lifestyle factors. Understanding stomatitis, its subtypes, and its management is crucial for both healthcare providers and individuals affected by the condition.
This article explores stomatitis in detail, covering its types, causes, symptoms, diagnosis, treatment, and preventive strategies.
Table of Contents
ToggleAnatomy of the Oral Cavity
Before delving into stomatitis, it is important to understand the structure of the oral cavity. The mouth is lined with a mucous membrane, consisting of epithelial cells that protect the tissues beneath from the harsh environment inside the mouth, including mechanical forces from chewing, chemical exposure from foods, and microbial invasion. Any damage or disruption to this delicate mucous lining can lead to inflammation and ulceration, the hallmark features of stomatitis.
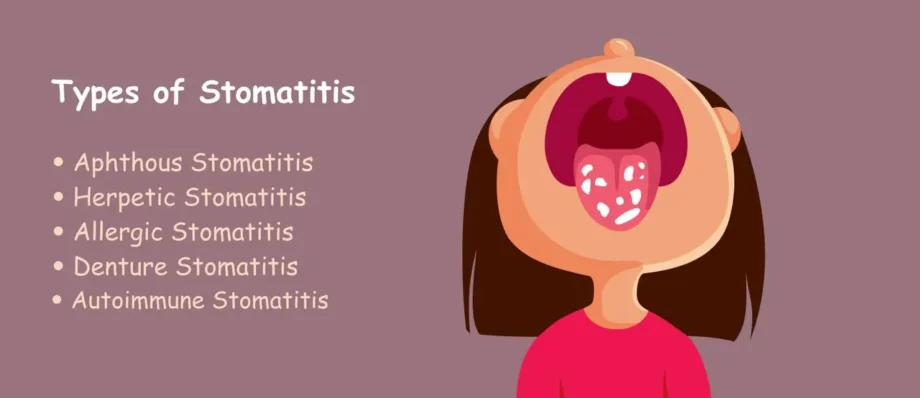
Types of Stomatitis
There are several types of stomatitis, each with different causes, manifestations, and treatments. The most common forms include:
- Aphthous Stomatitis (Canker Sores)
- Herpetic Stomatitis
- Allergic Stomatitis
- Denture Stomatitis
- Autoimmune Stomatitis (Lichen Planus and Pemphigus Vulgaris)
Aphthous Stomatitis (Canker Sores)
Aphthous stomatitis, commonly known as canker sores, is the most prevalent type of stomatitis. These sores are small, round, or oval ulcers that appear inside the mouth, typically on the tongue, the inner lining of the cheeks, or the base of the gums. They can be painful and make eating or talking uncomfortable. Aphthous ulcers are not contagious and typically resolve within one to two weeks.
Causes of Aphthous Stomatitis
The exact cause of aphthous stomatitis is unclear, but several factors can trigger it, including:
- Trauma: Biting the cheek, harsh brushing, or dental work can cause irritation.
- Nutritional Deficiencies: Deficiency in iron, vitamin B12, folate, and zinc may predispose individuals to aphthous ulcers.
- Stress: Emotional stress and anxiety are often linked to the appearance of canker sores.
- Hormonal Fluctuations: Women may experience outbreaks related to hormonal changes during menstruation.
- Food Sensitivities: Acidic or spicy foods can sometimes irritate the mouth and trigger sores.
Symptoms of Aphthous Stomatitis
- Small, round, or oval ulcers with a red border and a yellow or white center.
- Painful lesions, especially during eating or speaking.
- Sores typically last between 7 to 14 days.
- In severe cases, fever and swollen lymph nodes may accompany the ulcers.
Treatment
- Topical Treatments: Over-the-counter gels, creams, or mouth rinses containing anesthetics (lidocaine) or anti-inflammatory agents (hydrocortisone) can reduce pain and inflammation.
- Oral Medications: For severe or recurrent cases, oral corticosteroids or other immune-modulating drugs may be prescribed.
- Lifestyle Modifications: Avoiding trigger foods, practicing good oral hygiene, and reducing stress can help prevent flare-ups.
Herpetic Stomatitis
Herpetic stomatitis, also known as cold sores or fever blisters, is caused by the herpes simplex virus (HSV), most commonly HSV-1. This condition is highly contagious and can spread through direct contact with infected saliva or skin. Herpetic stomatitis is more common in children and can present as a primary infection or recurrent outbreaks.
Causes of Herpetic Stomatitis
- Primary Infection: Herpes simplex virus (HSV-1) enters the body through breaks in the skin or mucous membranes. After the initial infection, the virus becomes latent in the body and can reactivate later.
- Triggers for Recurrence: Factors like stress, fever, sun exposure, illness, or a weakened immune system can trigger a reactivation of the virus.
Symptoms of Herpetic Stomatitis
- Painful, fluid-filled blisters or sores on the lips, gums, tongue, or inside the mouth.
- Fever, swollen lymph nodes, and general malaise during the primary infection.
- The blisters eventually rupture, leaving painful ulcers that can take 7 to 10 days to heal.
Treatment
- Antiviral Medications: Prescription antiviral drugs like acyclovir, valacyclovir, or famciclovir can reduce the severity and duration of symptoms.
- Pain Relief: Over-the-counter pain relievers (ibuprofen, acetaminophen) and topical anesthetics can help alleviate discomfort.
- Supportive Care: Maintaining hydration and consuming soft, bland foods to avoid irritating the sores is essential during the healing process.
Allergic Stomatitis
Allergic stomatitis is an inflammatory reaction in the mouth caused by contact with allergens. This form of stomatitis can be triggered by food, dental materials, medications, or even toothpaste.
Causes of Allergic Stomatitis
- Food Allergies: Certain foods, especially those containing artificial additives or preservatives, can trigger oral inflammation.
- Dental Materials: Reactions to materials used in dental restorations, such as metals or acrylics, may result in stomatitis.
- Medications: Some drugs, particularly those used in chemotherapy, can cause allergic reactions in the mouth.
- Toothpaste and Mouthwash: Ingredients like sodium lauryl sulfate (SLS) in toothpaste or alcohol in mouthwash can sometimes cause irritation or allergic reactions.
Symptoms of Allergic Stomatitis
- Redness, swelling, and irritation of the oral mucosa.
- Burning or itching sensation in the mouth.
- In severe cases, ulcers or blisters may develop.
- Symptoms may improve once the allergen is removed.
Treatment
- Identification and Elimination of Allergens: Allergy testing or elimination diets can help identify the specific cause.
- Topical Corticosteroids: Prescription corticosteroid gels or rinses may be used to reduce inflammation.
- Antihistamines: Oral or topical antihistamines can help alleviate allergic symptoms.
Denture Stomatitis
Denture stomatitis, also known as denture-related stomatitis, is a common condition in individuals who wear dentures, particularly ill-fitting ones. It is characterized by inflammation and redness of the oral mucosa in areas that come into contact with the denture.
Causes of Denture Stomatitis
- Poor Oral Hygiene: Not properly cleaning dentures can lead to the accumulation of plaque and bacteria.
- Ill-Fitting Dentures: Dentures that do not fit well can cause chronic irritation to the oral mucosa.
- Candida Infection: Overgrowth of the fungus Candida albicans (Oral Candidiasis) is commonly associated with denture stomatitis, particularly in immunocompromised individuals.
Symptoms of Denture Stomatitis
- Red, inflamed mucous membranes under the denture.
- Mild discomfort or burning sensation.
- Presence of a whitish coating (in cases associated with fungal infection).
Treatment
- Proper Denture Hygiene: Regular cleaning of dentures and oral tissues is essential to prevent infection and irritation.
- Adjustment or Replacement of Dentures: Ensuring that the dentures fit properly can help alleviate symptoms.
- Antifungal Medications: If Candida overgrowth is present, antifungal agents like nystatin or fluconazole may be prescribed.
Autoimmune Stomatitis (Lichen Planus and Pemphigus Vulgaris)
Autoimmune conditions can also manifest as stomatitis, causing chronic inflammation and ulceration of the oral mucosa. Two significant autoimmune-related types of stomatitis are lichen planus and pemphigus vulgaris.
Lichen Planus
Lichen planus is an inflammatory condition that affects the skin and mucous membranes. In the mouth, it appears as white, lacy patches, red swollen tissues, or painful sores.
Causes of Lichen Planus
The exact cause of lichen planus is unknown, but it is believed to result from an autoimmune response, where the body’s immune system attacks its own tissues.
Symptoms of Lichen Planus
- White, lacy patches (Wickham striae) on the inside of the cheeks, tongue, or gums.
- Painful, red, or ulcerative lesions.
- Burning sensation in the mouth, especially when consuming acidic or spicy foods.
Treatment
- Topical Corticosteroids: These are the first line of treatment for reducing inflammation and controlling symptoms.
- Immune-Modulating Drugs: In severe cases, systemic immune-modulating drugs like cyclosporine may be used.
Pemphigus Vulgaris
Pemphigus vulgaris is a rare but serious autoimmune condition that causes blistering and erosion of the skin and mucous membranes, including the mouth.
Causes of Pemphigus Vulgaris
Pemphigus vulgaris is caused by the immune system mistakenly attacking proteins in the skin and mucous membranes that hold cells together, leading to the formation of blisters and sores.
Symptoms of Pemphigus Vulgaris
- Painful blisters or sores that rupture, leaving raw, ulcerated areas.
- Oral pain, difficulty eating, and sometimes difficulty speaking.
- Blisters can occur on other parts of the body, including the throat, esophagus, and skin.
Treatment
- Corticosteroids: High doses of systemic corticosteroids, such as prednisone, are typically used to control the inflammation and suppress the immune response.
- Immunosuppressive Drugs: Medications like azathioprine or mycophenolate mofetil may be used to control the autoimmune response.
- Biologic Therapy: Rituximab, a monoclonal antibody, has shown effectiveness in managing pemphigus vulgaris in more severe cases.
- Wound Care: Gentle oral hygiene and using soothing mouth rinses can help manage pain and prevent secondary infection.
Causes of Stomatitis
The causes of stomatitis are diverse and range from simple irritants to complex systemic diseases. Understanding the underlying cause is essential for effective treatment and prevention. Here are the primary causes of stomatitis:
- Infections
- Trauma and Irritation
- Allergic Reactions
- Nutritional Deficiencies
- Autoimmune Diseases
- Systemic Conditions
Infections
- Viral Infections
- Fungal Infections
- Bacterial Infections
Viral Infections
Herpes simplex virus (HSV) is a common cause of stomatitis. Other viruses, such as coxsackievirus, which causes hand-foot-and-mouth disease, and the varicella-zoster virus, responsible for chickenpox and shingles, can also lead to mouth ulcers.
Fungal Infections
Candida albicans, a fungal organism that causes oral thrush, is a common cause of stomatitis in immunocompromised individuals, such as those with HIV/AIDS, or those undergoing chemotherapy.
Bacterial Infections
Bacterial infections, particularly from Streptococcus and Staphylococcus species, can also lead to stomatitis, especially when oral hygiene is poor.
Trauma and Irritation
- Physical Trauma
- Chemical Irritation
Physical Trauma
Injury to the oral mucosa from biting the cheek or tongue, ill-fitting dental appliances, or burns from hot food can lead to stomatitis.
Chemical Irritation
Exposure to harsh chemicals, including tobacco smoke, alcohol, or ingredients in certain mouthwashes or toothpastes, can irritate the sensitive lining of the mouth.
Allergic Reactions
- Food Allergies
- Medications
- Contact Allergens
Food Allergies
Certain foods, especially citrus fruits, nuts, or shellfish, can cause allergic reactions that manifest as stomatitis.
Medications
Drugs, especially chemotherapeutic agents, NSAIDs, or antibiotics, can induce stomatitis as a side effect.
Contact Allergens
Some individuals may react to materials in dental work, such as metal fillings, braces, or denture adhesives.
Nutritional Deficiencies
- Vitamin and Mineral Deficiencies
- General Malnutrition
Vitamin and Mineral Deficiencies
Deficiencies in iron, vitamin B12, folate, or zinc can lead to stomatitis, particularly aphthous ulcers.
General Malnutrition
Malnourished individuals are more prone to infections and ulcerations of the oral cavity due to a weakened immune response.
Autoimmune Diseases
- Lupus Erythematosus
- Behçet’s Disease
- Inflammatory Bowel Disease (IBD)
Lupus Erythematosus
Systemic lupus erythematosus (SLE) can cause oral ulcers as part of its systemic involvement.
Behçet’s Disease
This chronic condition (Behchet’s Disease) causes recurrent mouth ulcers, along with genital ulcers and inflammation in other areas of the body, including the eyes and joints.
Inflammatory Bowel Disease (IBD)
Conditions such as Crohn’s disease and ulcerative colitis are often associated with aphthous stomatitis.
Systemic Conditions
- HIV/AIDS
- Chemotherapy and Radiation Therapy
HIV/AIDS
People living with HIV/AIDS are at a higher risk for various forms of stomatitis, including viral, fungal, and bacterial infections due to immunosuppression.
Chemotherapy and Radiation Therapy
Both chemotherapy and radiation therapy can cause mucositis, a severe form of stomatitis characterized by widespread inflammation and ulceration of the oral mucosa.
Symptoms of Stomatitis
Stomatitis can present with a variety of symptoms depending on the underlying cause and type. The most common symptoms include:
- Pain and Discomfort
- Redness and Swelling
- Ulceration and Blisters
- Dry Mouth and Burning Sensation
- Difficulty Eating or Drinking
- Fever and Fatigue
Pain and Discomfort
Pain is the hallmark symptom of stomatitis. It can range from mild irritation to severe discomfort, especially when eating, drinking, or speaking. The location and intensity of the pain depend on the type and cause of stomatitis.
Redness and Swelling
Inflammation often leads to redness and swelling of the affected areas. In more severe cases, the swelling may make it difficult to open the mouth or chew food properly.
Ulceration and Blisters
Most types of stomatitis are associated with ulcer formation. These ulcers may be shallow or deep, round or oval, and can have a yellow, gray, or white center surrounded by a red halo. In herpetic stomatitis, fluid-filled blisters that burst and leave painful sores are common.
Dry Mouth and Burning Sensation
Individuals with stomatitis may experience a dry, burning sensation, particularly if the salivary glands are affected or the mucous membranes are severely inflamed. This can exacerbate the discomfort caused by the ulcers or lesions.
Difficulty Eating or Drinking
Due to the pain and discomfort, individuals with stomatitis may avoid eating or drinking, leading to dehydration or malnutrition in severe cases.
Fever and Fatigue
Systemic symptoms like fever, malaise, and fatigue can accompany more severe forms of stomatitis, particularly if it is caused by a viral infection or an autoimmune disorder.
Diagnosis of Stomatitis
Diagnosing stomatitis typically involves a combination of clinical examination, patient history, and sometimes additional tests to identify the underlying cause.
- Clinical Examination
- Patient History
- Laboratory Tests
- Allergy Testing
Clinical Examination
A healthcare provider will visually examine the mouth for signs of inflammation, ulcers, blisters, or other abnormalities. They may also inspect for signs of infection, such as the presence of white patches indicative of fungal infection or clusters of blisters typical of herpes stomatitis.
Patient History
A thorough medical history helps identify potential triggers for stomatitis, such as recent infections, food sensitivities, medication use, or systemic illnesses like autoimmune diseases.
Laboratory Tests
In some cases, laboratory tests may be necessary to identify the cause of stomatitis:
- Viral or Bacterial Cultures: Swabs of the affected area may be taken to test for the presence of bacteria, viruses, or fungi.
- Blood Tests: Blood tests can check for underlying conditions like autoimmune diseases, nutritional deficiencies, or systemic infections.
- Biopsy: A small tissue sample may be taken for biopsy in cases where autoimmune diseases or more serious conditions like oral cancer are suspected.
Allergy Testing
If allergic stomatitis is suspected, allergy testing may be performed to identify potential allergens responsible for triggering the condition.
Treatment of Stomatitis
The treatment of stomatitis depends on its cause, severity, and the individual’s overall health. Here are the primary treatment options:
- Topical Treatments
- Oral Medications
- Pain Relief
- Treatment of Underlying Conditions
- Lifestyle Modifications
Topical Treatments
- Anesthetics: Topical anesthetic gels or sprays (e.g., lidocaine) can provide temporary pain relief by numbing the area.
- Corticosteroids: Topical corticosteroids, such as hydrocortisone or triamcinolone, help reduce inflammation and pain, particularly in autoimmune or severe aphthous stomatitis.
- Antimicrobial Mouthwashes: Antimicrobial or antifungal rinses can be used to reduce bacterial or fungal load, especially in cases of infectious stomatitis.
Oral Medications
- Antiviral Drugs: In cases of herpetic stomatitis, antiviral medications like acyclovir or valacyclovir can reduce the severity and duration of the infection.
- Immunosuppressive Drugs: For autoimmune-related stomatitis, systemic immunosuppressants like azathioprine or methotrexate may be required to control the underlying immune response.
- Systemic Corticosteroids: In severe cases, oral corticosteroids like prednisone may be prescribed to reduce inflammation throughout the body, including the oral cavity.
Pain Relief
- Over-the-Counter Analgesics: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or acetaminophen, can help relieve pain and reduce inflammation.
Treatment of Underlying Conditions
Treating the underlying cause is essential in managing stomatitis. For example:
- Nutritional Supplementation: If nutritional deficiencies are the cause, supplementation with iron, B vitamins, or zinc may help resolve the symptoms.
- Treatment of Autoimmune Disorders: In cases of autoimmune-related stomatitis, controlling the underlying condition (e.g., lupus, Crohn’s disease) is crucial for managing oral symptoms.
Lifestyle Modifications
- Oral Hygiene: Maintaining good oral hygiene by brushing with a soft toothbrush and avoiding harsh mouthwashes can help prevent further irritation and infection.
- Dietary Changes: Avoiding spicy, acidic, or hard foods can minimize irritation during flare-ups of stomatitis.
Prevention of Stomatitis
Preventing stomatitis often involves addressing the underlying triggers or risk factors. Here are some effective prevention strategies:
- Good Oral Hygiene
- Balanced Diet
- Avoiding Triggers
- Managing Stress
- Proper Denture Care
- Immune System Support
Good Oral Hygiene
Regular brushing, flossing, and the use of an antimicrobial mouthwash can help maintain oral health and prevent infections that lead to stomatitis.
Balanced Diet
Maintaining a balanced diet rich in essential vitamins and minerals is important for overall oral health and can help prevent stomatitis, particularly for individuals prone to nutritional deficiencies. Key nutrients to focus on include:
- Iron: Found in red meat, leafy greens, and legumes, iron deficiency can lead to sores and ulcerations in the mouth.
- Vitamin B12: Present in animal products like fish, eggs, and dairy, vitamin B12 is essential for maintaining healthy oral tissues.
- Folate (Vitamin B9): Found in fortified cereals, green vegetables, and beans, folate supports tissue repair and reduces the risk of ulcer formation.
- Zinc: Zinc, available in nuts, seeds, and whole grains, is critical for immune function and wound healing.
Avoiding Triggers
For individuals prone to allergic or irritant-induced stomatitis, avoiding common triggers can significantly reduce flare-ups. Some key avoidance strategies include:
- Elimination of Irritant Foods: Acidic, spicy, or rough-textured foods can irritate the oral mucosa. Avoiding foods like citrus fruits, tomatoes, and crunchy snacks during stomatitis outbreaks may reduce irritation.
- Identifying and Avoiding Allergens: Individuals who develop stomatitis as a result of allergic reactions to foods, dental materials, or medications may benefit from working with an allergist to identify and avoid specific allergens.
- Switching Oral Care Products: If toothpaste or mouthwash ingredients like sodium lauryl sulfate or alcohol are causing irritation, switching to gentler products formulated for sensitive mouths may help prevent stomatitis.
Managing Stress
Since stress is a known trigger for aphthous stomatitis and other forms of mouth ulcers, stress management techniques can be an effective preventive measure. These strategies include:
- Mindfulness and Meditation: Engaging in relaxation techniques, such as mindfulness meditation or yoga, can help reduce stress levels.
- Regular Physical Activity: Exercise is known to improve mood and reduce stress, which may decrease the frequency of stress-related mouth ulcers.
- Adequate Sleep: Ensuring sufficient rest and maintaining a healthy sleep routine can also help mitigate the effects of stress on the body, including oral health.
Proper Denture Care
For individuals who wear dentures, proper care and maintenance are critical to preventing denture-related stomatitis. Key preventive steps include:
- Cleaning Dentures Regularly: Dentures should be cleaned daily with a brush and mild soap, followed by soaking them in a cleansing solution. This helps reduce plaque buildup and prevent fungal infections like Candida.
- Proper Fit of Dentures: Ensuring that dentures fit well and do not rub against the oral mucosa can prevent irritation and inflammation.
- Removing Dentures at Night: Giving the mouth a break by removing dentures at night allows the tissues to heal and reduces the risk of developing denture stomatitis.
Immune System Support
Strengthening the immune system can help prevent infections that lead to stomatitis. Some ways to support immune health include:
- Vaccinations: Receiving vaccinations for viruses such as the herpes simplex virus can reduce the risk of herpetic stomatitis.
- Healthy Lifestyle Choices: Regular exercise, a balanced diet, and avoiding smoking and excessive alcohol consumption contribute to a strong immune system.
- Managing Chronic Conditions: Keeping chronic conditions like diabetes, HIV, or autoimmune diseases well-managed helps prevent infections and mouth sores associated with compromised immune function.
Complications of Stomatitis
If left untreated or poorly managed, stomatitis can lead to several complications that may significantly affect a person’s quality of life. These complications include:
- Secondary Infections
- Nutritional Deficiencies
- Dehydration
- Impaired Oral Function
- Psychological Impact
Secondary Infections
Stomatitis can create open sores or ulcers in the mouth, which may become infected with bacteria, viruses, or fungi. Secondary infections can prolong healing times, worsen pain, and increase the risk of more serious conditions, such as cellulitis or oral abscesses.
Nutritional Deficiencies
Individuals with severe or recurrent stomatitis may avoid eating due to pain, which can lead to malnutrition, weight loss, or exacerbation of existing nutritional deficiencies. This is especially true for those who already have conditions that impair nutrient absorption, such as Crohn’s disease or celiac disease.
Dehydration
Painful ulcers or blisters in the mouth can make drinking fluids uncomfortable, leading to dehydration. This is especially common in children or older adults who may not express discomfort but avoid eating and drinking.
Impaired Oral Function
Severe cases of stomatitis can significantly impair a person’s ability to speak, chew, or swallow, affecting day-to-day activities. In some cases, chronic stomatitis can lead to scarring or permanent damage to the oral mucosa.
Psychological Impact
Chronic or recurrent stomatitis can take a toll on mental health, leading to anxiety or depression, especially when it interferes with basic activities such as eating, speaking, or interacting socially. The stress and frustration of managing a chronic condition can also exacerbate symptoms, creating a cycle of flare-ups and emotional distress.
When to Seek Medical Attention
While many cases of stomatitis resolve on their own or with over-the-counter treatments, there are times when medical intervention is necessary. Individuals should seek medical advice if they experience:
- Severe pain or difficulty eating and drinking.
- Sores that persist longer than two weeks.
- Recurrent episodes of stomatitis.
- Fever, swollen lymph nodes, or signs of systemic infection.
- Unexplained weight loss or signs of malnutrition.
- Blisters or ulcers spreading beyond the mouth.
- Symptoms of autoimmune disorders, such as joint pain, skin rashes, or gastrointestinal issues.
A healthcare provider can help determine the underlying cause of stomatitis and recommend appropriate treatment options. In some cases, referral to a specialist, such as a dermatologist, immunologist, or gastroenterologist, may be required to manage more complex underlying conditions.
Frequently Asked Questions (FAQs)
Will stomatitis go away on its own?
Stomatitis may resolve on its own, depending on the cause. Mild cases, such as those due to minor irritation or stress, often improve without treatment. However, if stomatitis is caused by an infection, vitamin deficiency, or an underlying health condition, medical treatment may be required to speed up recovery and prevent complications.
Is stomatitis contagious?
Stomatitis itself is not always contagious, but if it results from a viral or bacterial infection, such as herpes simplex virus (HSV) or hand, foot, and mouth disease, it can be spread through saliva, direct contact, or sharing utensils. Practicing good hygiene and avoiding close contact with others when experiencing symptoms can help prevent transmission.
Does mouthwash help stomatitis?
Certain mouthwashes, especially those containing antiseptic, antifungal, or anti-inflammatory ingredients, may help alleviate symptoms and promote healing. Mouthwashes with chlorhexidine or hydrogen peroxide can help reduce bacterial infections, while those containing lidocaine may provide pain relief. However, alcohol-based mouthwashes should be avoided as they can further irritate the affected area.
Does denture stomatitis go away on its own?
Denture stomatitis may persist without proper intervention. It is usually caused by a fungal infection (Candida) and can be exacerbated by poor denture hygiene. To resolve it, proper cleaning of dentures, soaking them in antifungal solutions, and maintaining good oral hygiene are essential. In some cases, antifungal medications may be required to treat persistent infections.
What is the fastest way to cure stomatitis?
The fastest way to cure stomatitis depends on the underlying cause. If caused by an infection, antiviral, antifungal, or antibacterial treatments may be necessary. Maintaining good oral hygiene, using soothing oral rinses (such as warm salt water or medicated mouthwashes), avoiding irritants (such as spicy foods, alcohol, and tobacco), and ensuring adequate hydration can speed up healing. In cases of nutritional deficiencies, supplementing with the necessary vitamins can help resolve symptoms more quickly.
How did I get stomatitis?
Stomatitis can result from a variety of causes, including infections (viral, bacterial, or fungal), exposure to irritants (such as spicy or acidic foods, tobacco, and alcohol), allergic reactions, nutritional deficiencies, or an underlying health condition such as autoimmune diseases or diabetes. Stress and trauma to the mouth (such as biting the cheek or ill-fitting dentures) can also contribute to its development.
What STD causes stomatitis?
Certain sexually transmitted diseases (STDs) can cause stomatitis or oral ulcers. Herpes simplex virus (HSV-1 and HSV-2) is a common cause, leading to painful cold sores or blisters in the mouth. Syphilis can also cause oral sores, particularly in the secondary stage of the infection. Additionally, HIV can increase susceptibility to oral infections, including stomatitis.
What vitamin deficiency causes stomatitis?
Deficiencies in essential vitamins and minerals can contribute to the development of stomatitis. Common deficiencies include:
- Vitamin B2 (riboflavin): Causes cracked lips and mouth sores.
- Vitamin B3 (niacin): Associated with painful ulcers and inflammation in the mouth.
- Vitamin B6 and B12: Deficiencies can lead to burning sensations and sores in the mouth.
- Iron: Low iron levels can result in oral ulcers and glossitis (inflammation of the tongue).
- Folic acid: Plays a role in cell regeneration; its deficiency can lead to mouth sores and gum irritation. Correcting these deficiencies through dietary changes or supplementation can help resolve symptoms.
Can anxiety cause stomatitis?
Yes, stress and anxiety can contribute to stomatitis in several ways. Chronic stress can weaken the immune system, making the body more susceptible to infections, including those that cause stomatitis. Additionally, anxiety-related habits such as lip or cheek biting, teeth grinding, or increased acid production in the mouth can lead to irritation and ulcer formation. Managing stress through relaxation techniques, proper sleep, and a balanced diet may help prevent recurrent episodes of stomatitis.
Conclusion
Stomatitis is a common and often painful condition affecting the mucous membranes of the mouth. Its many forms—including aphthous ulcers, herpetic stomatitis, allergic reactions, and autoimmune-related stomatitis—each have distinct causes, symptoms, and treatment options. While mild cases of stomatitis often resolve on their own, more severe or recurrent forms may require medical intervention.
Prevention plays a critical role in managing stomatitis, especially for individuals prone to flare-ups. Maintaining good oral hygiene, eating a balanced diet, avoiding known triggers, and managing stress can help reduce the incidence and severity of stomatitis. Early diagnosis and treatment can prevent complications, allowing individuals to manage their symptoms effectively and maintain their quality of life.
Ultimately, by understanding the various types of stomatitis and their underlying causes, healthcare providers and patients alike can take proactive steps to ensure timely treatment and minimize discomfort associated with this common oral condition.