Tooth extraction is among the most common procedures performed in dentistry. While extraction is often necessary to address infection, advanced periodontal disease, trauma, or non-restorable caries, it inevitably leads to a cascade of biological events that alter the alveolar ridge. Post-extraction remodeling typically results in significant resorption of alveolar bone, especially within the first few months. This reduction in both vertical and horizontal ridge dimensions can compromise function, esthetics, and future prosthetic rehabilitation, particularly dental implant placement.
Socket preservation (also known as alveolar ridge preservation or extraction socket management) refers to the set of surgical and biomaterial techniques aimed at minimizing post-extraction bone loss. By intervening immediately following tooth removal, clinicians can stabilize the alveolus, maintain ridge volume, and create more favorable conditions for prosthetic or implant therapy.
This article provides a comprehensive discussion of socket preservation, covering the biological basis, remodeling processes, clinical indications, techniques, biomaterials, outcomes, limitations, and future directions.
Table of Contents
ToggleBiological Basis of Post-Extraction Bone Remodeling
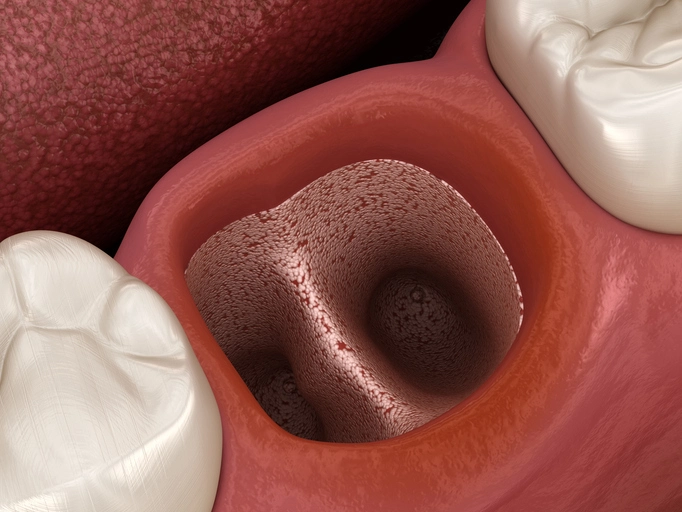
When a tooth is extracted, it triggers a series of healing processes within the socket. Understanding this biology is essential for appreciating why socket preservation is important.
1. Immediate Healing Events
- Formation of a blood clot, rich in platelets and growth factors, fills the extraction socket.
- Migration of neutrophils and macrophages initiates inflammation and wound debridement.
- Angiogenesis and fibroblast proliferation occur within days.
2. Early Bone Healing (Weeks 1–4)
- Osteoclast-mediated bone resorption begins along the bundle bone (the alveolar bone proper that anchors periodontal fibers).
- Woven bone gradually replaces the blood clot through intramembranous ossification.
3. Remodeling Phase (Weeks 6–12)
- Bundle bone, dependent on the periodontal ligament, is lost.
- Rapid horizontal and vertical ridge resorption occurs, most prominently in the buccal plate.
- Studies report 29–63% horizontal reduction and 11–22% vertical reduction within 6 months post-extraction.
4. Long-Term Changes
- Continued remodeling leads to ridge narrowing and centripetal bone resorption.
- Esthetic zones (anterior maxilla) are particularly vulnerable due to thin buccal plates.
This natural bone loss explains the clinical rationale for socket preservation: to maintain ridge architecture and optimize conditions for future restorative therapy.
Indications for Socket Preservation
Socket preservation is not universally required for all extractions. Indications include:
- Future Implant Placement: Preserves alveolar volume, reducing the need for later grafting.
- Esthetic Zones: Maintains buccal contour and gingival architecture, critical for anterior implants or prostheses.
- Thin Buccal Plate (<1 mm): High risk of collapse without intervention.
- Multi-rooted Extractions: Larger sockets predispose to resorption and collapse.
- Periodontal or Endodontic Involvement: Infection and bone loss require regenerative management.
- Patients with Systemic Risks: Smokers, osteoporotic patients, or those with compromised healing may benefit from bone substitutes that slow resorption.
Contraindications include uncontrolled infection, insufficient soft tissue for closure, or medically unstable patients.
Techniques for Socket Preservation
Socket preservation encompasses various surgical approaches depending on clinical goals, bone anatomy, and prosthetic requirements.
1. Atraumatic Tooth Extraction
The foundation of socket preservation begins with careful extraction.
- Minimize trauma: Use periotomes, luxators, and physics forceps rather than elevators that fracture bone.
- Preserve cortical plates: Buccal bone is thin and easily damaged.
- Flapless approaches: Avoid periosteal elevation, which accelerates bone resorption.
2. Socket Grafting
The socket is filled with graft material to stabilize the clot and maintain volume.
- Particulate grafts: Bone substitutes are the most common.
- Block grafts: Occasionally used in large sockets but less common.
3. Barrier Membranes
Membranes prevent soft tissue invasion and allow osteogenic cells to populate the graft.
- Resorbable membranes (e.g., collagen): Easy handling, no second surgery required.
- Non-resorbable membranes (e.g., PTFE): Superior space maintenance but require removal.
4. Socket Sealing
Soft tissue closure enhances healing. Options include:
- Primary flap closure.
- Collagen sponge or membrane tucked under gingival margins (“socket seal”).
- Autogenous connective tissue grafts.
5. Advanced Variations
- Sticky bone: Particulate grafts mixed with platelet-rich fibrin (PRF).
- Bone ring or shell techniques: For severe defects needing simultaneous augmentation.
- Immediate implant placement with grafting: Implants stabilize the socket while grafts fill voids.
Biomaterials in Socket Preservation
The choice of graft material is central to socket preservation. Materials differ in their osteogenic, osteoinductive, and osteoconductive properties.
1. Autografts
- Harvested from patient (intraoral or extraoral).
- Gold standard due to osteogenic cells and growth factors.
- Limited volume and donor site morbidity restrict use.
2. Allografts
- Derived from cadaveric human bone (FDBA – freeze-dried bone allograft; DFDBA – demineralized freeze-dried).
- Osteoconductive and, in DFDBA, mildly osteoinductive.
- Widely used with favorable outcomes.
3. Xenografts
- Bovine, porcine, or equine origin.
- Highly osteoconductive, slow resorption maintains volume long-term.
- Popular in esthetic and implant sites.
4. Alloplasts
- Synthetic materials (e.g., hydroxyapatite, β-TCP, bioactive glass).
- Osteoconductive scaffold, resorption varies.
- Often used in combination with biologics.
5. Growth Factors and Biologics
- PRF/PRP: Enhance angiogenesis and healing.
- BMPs (Bone Morphogenetic Proteins): Potent osteoinduction but costly and regulated.
- EMD (Enamel Matrix Derivatives): Aid in periodontal regeneration.
6. Membrane Selection
- Collagen resorbable membranes dominate clinical practice.
- PTFE and titanium-reinforced barriers for larger or complex defects.
Clinical Outcomes of Socket Preservation
Ridge Dimensional Changes
- Systematic reviews show socket preservation reduces horizontal bone loss by ~2 mm and vertical loss by ~1 mm compared to ungrafted sites.
- Not a complete prevention: Some degree of remodeling still occurs.
Implant Therapy Benefits
- Higher implant survival rates in grafted sockets.
- Greater primary stability and better esthetic outcomes.
- Reduced need for secondary augmentation at implant placement.
Prosthetic Outcomes
- Maintains ridge contour for removable and fixed prostheses.
- Improves esthetics by preserving papilla and gingival architecture.
Histological Findings
- Most grafts show partial resorption and replacement with vital bone.
- Xenografts may persist long-term but provide stable volume.
- Autografts and allografts typically integrate faster.
Limitations and Challenges
Despite advantages, socket preservation is not without challenges.
Incomplete Ridge Preservation
Remodeling is reduced but not eliminated.
Material Selection Dilemmas
Clinicians must balance resorption rate, handling, and long-term stability.
Cost and Patient Factors
Graft materials and membranes increase procedural expense.
Patient compliance with post-op care influences success.
Complications
Membrane exposure and infection.
Graft material loss or soft tissue dehiscence.
Evidence Gaps
Long-term randomized controlled trials are limited.
Debate persists over ideal biomaterials and protocols.
Future Directions in Socket Preservation
Research is advancing toward biologically driven regeneration and minimally invasive methods. Promising trends include:
- Next generation biomaterials: Smart scaffolds that release growth factors in a controlled manner.
- Stem cell therapy: Harnessing mesenchymal stem cells for enhanced osteogenesis.
- 3D printing: Customized scaffolds for patient-specific defects.
- Tissue engineering: Combining biomaterials with biologics and gene therapy.
- Minimally invasive protocols: Flapless regenerative techniques for faster recovery.
Conclusion
Socket preservation has emerged as a cornerstone in modern oral surgery and implant dentistry. While natural post-extraction bone resorption is unavoidable, clinical techniques and biomaterials can significantly mitigate dimensional changes. Atraumatic extraction, careful case selection, appropriate grafting, and membrane use yield predictable outcomes that enhance prosthetic rehabilitation.
Though not a substitute for comprehensive ridge augmentation in severely atrophic sites, socket preservation provides a proactive approach to maintaining ridge volume, especially in esthetically demanding zones and implant-driven treatment plans. As regenerative technologies evolve, socket preservation will continue to refine toward more predictable, minimally invasive, and biologically enhanced solutions.